NuLiv Science is one of the industry's leading nutraceutical and dietary-supplement formulators. You've likely heard of them before: One of their patented ingredients, AstraGin, is used by countless brands to help boost ingredient bioavailability, and it's quite effective in doing so. With AstraGin's success, the industry took notice when they came to market with their metabolic enhancement ingredient:
InnoSlim: NuLiv’s Multi-Faceted Weight Loss Ingredient
InnoSlim, possibly the most novel release from NuLiv Science, is NuLiv Science's first foray into the world of fat-burning. It amplifies the body's internal engines responsible for metabolic rate, and its effects reach across multiple mechanisms involved with burning fat. InnoSlim is an ideal ingredient to help manage weight, blood sugar levels, and energy levels.
InnoSlim is a stimulant-free weight loss ingredient with human clinical data showing it can assist weight loss, improve lipids, reduce insulin resistance, and far more - all covered in this deep-dive article
InnoSlim is an innovative twist on typical fat-burning ingredients, and when we originally wrote this article in 2019, we stated that we expected to see it more often. That certainly happened - InnoSlim is now in several very well-formulated supplements - and now we discuss research published in 2021 and 2022 as well.
InnoSlim is an incredible addition to any weight loss regimen. Given that it's a non-stimulatory ingredient, we think it's perfectly suited for pairing with the following types of supplements:
- Stimulant-free fat burners
- Stimulant-based fat burners
- Glucose disposal agents
- Carnitine supplements
Now Available in Some Incredible Weight Loss Supplements
We cover some great products with InnoSlim at the end of this article, but some great examples are Glaxon Thermal (stimulant-free fat burning powder), Healthgevity Ignite (advanced glucose disposal agent), and Alpha Lion Apex Burn (stimulant-based fat-burning powder).
In this post, we'll take a deep plunge into the science behind InnoSlim by NuLiv Science, covering all of the mechanisms at play and the research behind this awesome fat-burning ingredient. Before we get to that, though, make sure you're subscribed to PricePlow for some of the best supplement deals, news, reviews, and interviews you can find!
Subscribe to PricePlow's Newsletter and Alerts on These Topics
This area is reserved for Team PricePlow's upcoming Ingredients video.
Subscribe to our channel and sign up for notifications so you catch it when it goes live!
What is InnoSlim?
InnoSlim is a patented[1-4] blend of Astragalus membranaceus and Panax notoginseng — similar to Astragin (another NuLiv Science product), but formulated to aid weight-loss efforts and reduce symptoms of metabolic syndrome. It targets several mechanisms (we discuss them in detail below), and has a whopping 18 in-vitro studies, 2 in-vivo studies, and two human studies from 2021 and 2022[5,6] backing its efficacy.
But the use of InnoSlim's constituent plants far predates the invention of the modern clinical trial:
Historical Use of Astragalus and Ginseng: Life-Extending Adaptogens
Astragalus and ginseng have a variety of uses in traditional Chinese medicine (TCM), but one important commonality is that they're thought to increase qi, a technical term for a concept that roughly translates to life force.[7,8] According to TCM, qi is the force that enables the body to renew and repair itself.[9] Accordingly, adequate qi levels confer health and longevity; low levels can lead to illness and premature death.
We should point out that scientists consider Astragalus membranaceus an adaptogen.[10]
Even the prestigious Oxford English Dictionary names ginseng as an example of an adaptogen![11] Their definition of adaptogen, by the way, is "A natural substance considered to help the body adapt to stress and to exert a normalizing effect upon bodily processes. A well-known example is ginseng."[12]
It isn't hard to see the overlap between this definition and TCM's concept of qi.
There's tons to write about the history of these plants, but, for the purposes of this article, their adaptogen status is all we really need to know.
We expect such a broad mechanism of action to have many different effects, and that's exactly what we demonstrate in the ensuing discussion. We'll see, over and over again, how astragalus and ginseng help normalize so many separate aspects of human health and metabolism.
In light of their broad mechanisms of action, it's probably not surprising that both plants have been studied as longevity supplements and have been shown to exert significant anti-aging effects.[13,14]
"Anti-aging" is obviously another broad category. But we invoke it just to show how these plants can fundamentally improve human health.
InnoSlim combats signs of metabolic syndrome!
By now, most of us have heard that metabolic health is paramount for a long and healthy life. Metabolic dysfunctions like hyperglycemia (high blood sugar) and hyperlipidemia (high levels of fatty acids in the blood, such as cholesterol and triglycerides) can, if left untreated long enough, precipitate a disorder called metabolic syndrome.
Metabolic syndrome is a term used to describe a constellation of metabolic issues, with insulin resistance and inflammation being the key mechanisms. It's basically pre-diabetes[15] and can lead to obesity.[5]
What makes metabolic syndrome so challenging to manage is that its progression could be characterized as a vicious cycle – poor metabolic function can cause an insatiable appetite, which naturally leads to poor food choices and thus damages the metabolism even more.
The modern environment can make these problems much worse by virtue of psychosocial stress. Stress does more than increase cortisol levels – it worsens nearly every marker of metabolic health and makes you more susceptible to unwanted fat gain.
At the center of this Gordian knot is insulin resistance, a condition in which cells are unable to respond to normal signaling from the hormone insulin, It's considered a major factor in the development of both hyperglycemia and hyperlipidemia.[16,17] Anything that can increase insulin sensitivity—making your cells more responsive to insulin—is thus a potential boon for long-term metabolic health.
Because of how fundamental it is to metabolic health, decreasing insulin resistance is usually the starting point for any strategy to slow or reverse the progression of metabolic syndrome.
It was with this in mind that a team of researchers from Taiwan recently set out to investigate whether astragalus and ginseng could improve metabolic health.
-
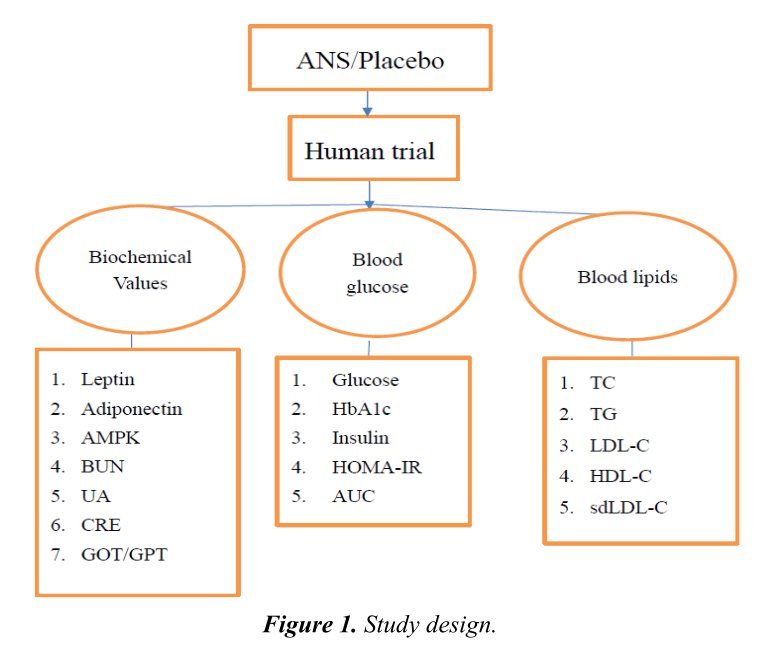
InnoSlim’s human clinical trial – Huang et al. 2022
This study was randomized, double-blind, and placebo-controlled,[5] considered the gold standard of medical research because of how effectively it eliminates the potential for biased results. It's particularly exciting because it was the first, and so far remains the only, human trial of astragalus and ginseng for hyperglycemia and hyperlipidemia.[5]
We read a lot of studies in the course of reporting for the PricePlow Blog, so take it from us, this study is impressive. Not only did the researchers opt for the RCT study design, but they also measured pretty much every major variable of metabolic health and function, leaving no proverbial stone unturned in their examination of whether astragalus and ginseng could improve human metabolism.
It was also a crossover study, meaning that the experimental subjects served as their own placebo control. They took the standardized Astragalus and notoginseng extract (ANS) for a six week period, then observed a four month washout period that served to eliminate the active effects of the supplement. Then they did another six week trial period, this time taking the placebo control.[5]
The subjects were instructed to maintain their normal lifestyle and dietary habits throughout the study.
Astragalus + Notoginseng Extract (InnoSlim) significantly improved key markers of metabolic health in the study subjects.[5]
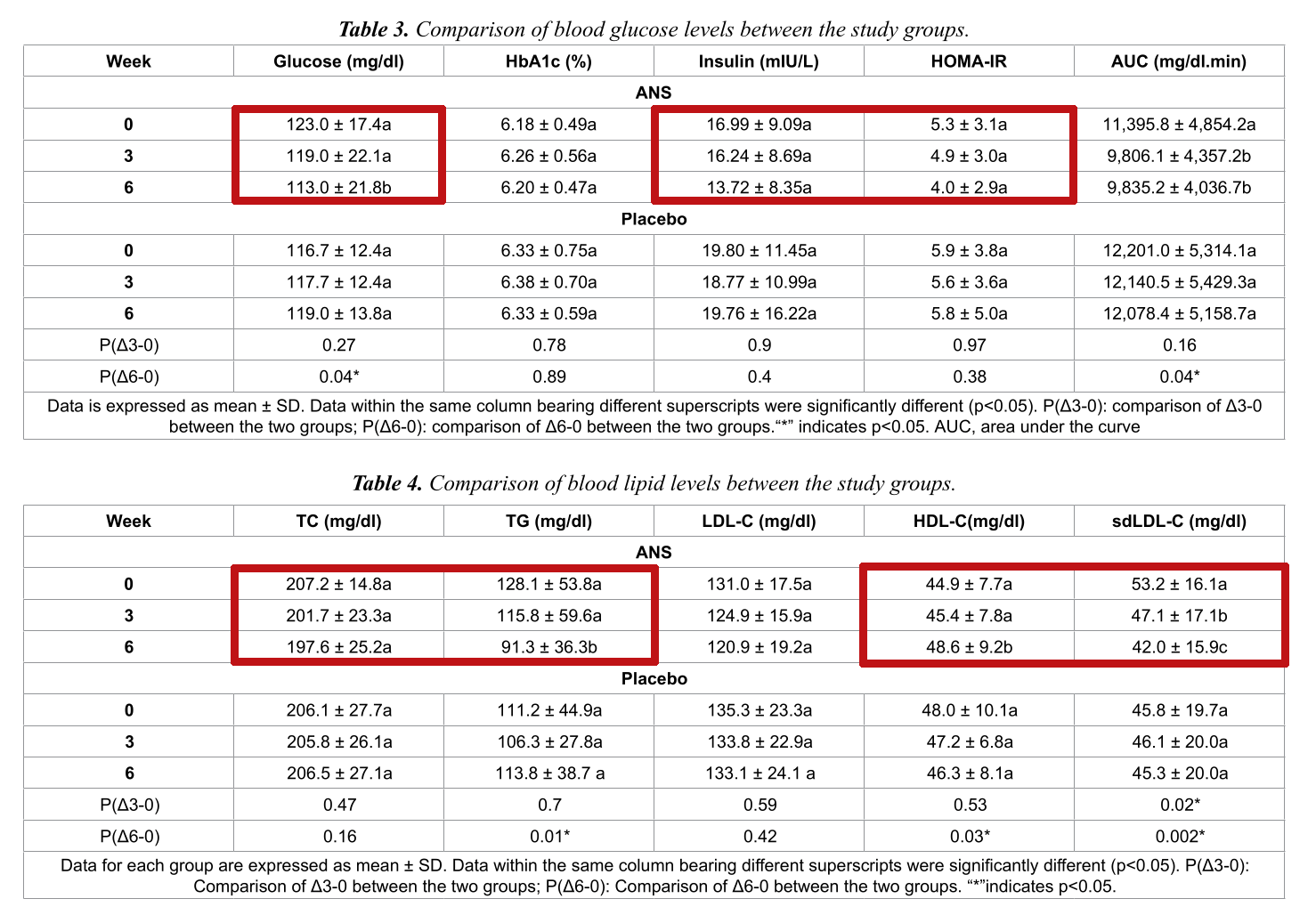
The results were striking. During the six week ANS period, study participants saw an average reduction of approximately 25% in their HOMA-IR score, which is a method researchers use to quantify insulin resistance.[5]
Incredible blood and lipid biomarker changes
Since insulin resistance leads to insulin overproduction, we hoped to see reductions in blood insulin levels as well. Fortunately, the Astragalus + Notoginseng group saw about a 20% reduction in blood insulin.[5]
Additional improvements observed during the ANS period—a 5% reduction in total cholesterol, 8% reduction in the controversial LDL cholesterol, and 8% reduction in blood glucose levels—all naturally follow from improved insulin function.
The Insulin Resistance Trifecta: Decrease in Insulin, Increase in HDL, Decrease in TG
But the real whopper is the nearly 30% reduction in blood triglycerides (TG) paired with 8% increase in "healthy" HDL cholesterol![5] There's a strong association between blood TG levels and glycemic control, making TGs a major risk factor for metabolic syndrome and diabetes.[18] Needless to say, a reduction this significant is a huge deal.
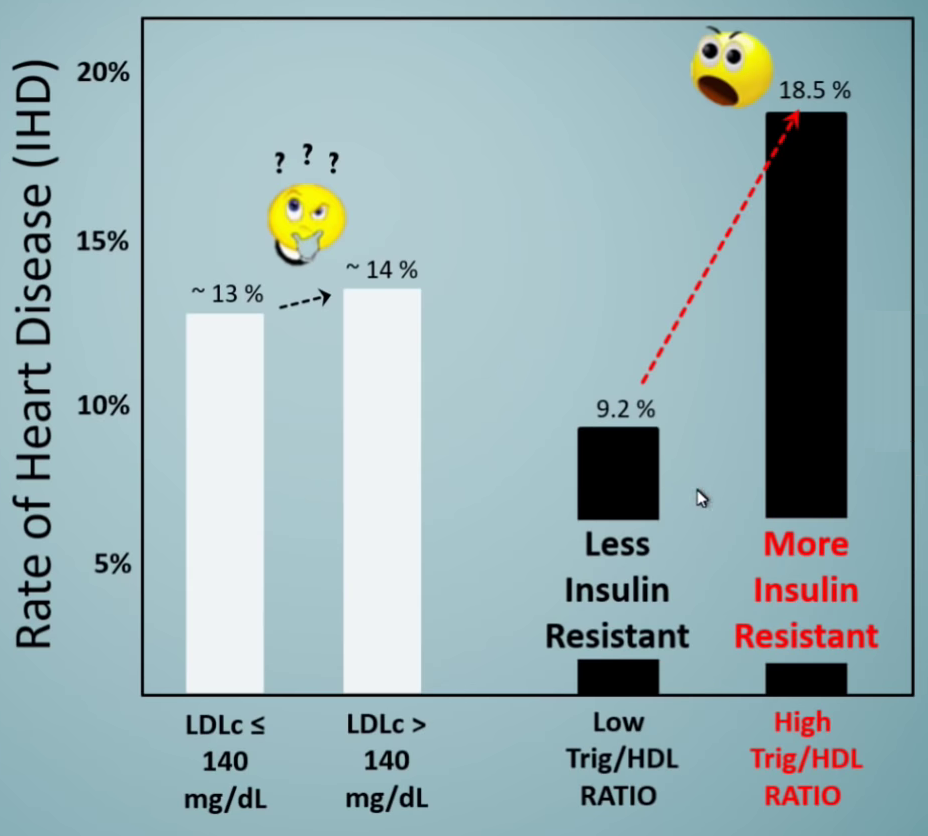
When it comes to heart disease risk, high LDL has nothing compared to higher triglycerides paired with lower HDL.[19] And guess what InnoSlim improves!
Further, we've repeatedly stated on this Blog that one's triglyceride-to-HDL cholesterol ratio is a far better risk factor than LDL cholesterol.[19-23] Sadly, LDL is the one doctors obsess over and prescribe drugs over, but it's meaningless in the context of these other two stronger variables -- HDL and TG -- which are far greater predictors of insulin resistance and mortality.[19,24]
When we see an ingredient increase HDL -- something prescription drugs cannot do effectively, we take note. When we see that coupled with a serious reduction in triglycerides, we downright get excited.
Even more importantly, these effects were coupled with a serious decrease in serum insulin,[5] leading us to believe that InnoSlim can immensely help in the fight against insulin resistance.
Another interesting category to note is sdLDL-C, which stands for small dense low-density lipoprotein-cholesterol. This isn't a standard item on routine blood work, so most readers may not have heard of it before. Let's see what the authors of the study have to say about this metric:
"sdLDL-C is a small and very low-density cholesterol. It is the end product of LDL-C oxidation. When sdLDL-C level in human body is high, it intrudes the vascular endothelial cells and induces phagocytosis of macrophages, leading to atherosclerosis. ANS decreased sdLDL-C significantly after 6 weeks of oral supplementation, indicating ANS was capable of reducing the production of LDL-C oxides. This result suggests ANS may have an anti-atherosclerotic effect, which requires further validation."[5]
Interesting stuff. This is the part of LDL we should be more concerned with -- not all LDL is bad -- hence the "LDL paradox" where individuals with high total LDL consistently live longer.[25] The hint is that there is no "LDL paradox" -- LDL, at large, isn't the demon it's made to be.
As an update in 2023, another cohort study on nearly 1,500 men found that "higher TC [total cholesterol] and LDL-C were independently and paradoxically associated with lower risk of all-cause mortality and longer survival time in men" -- the study found a 32% lower death rate in men with LDL over 190![26]
So focus on HDL and triglycerides and you get a far greater indicator... and this is something InnoSlim happens to correct.
The study illustrates a powerful mechanism
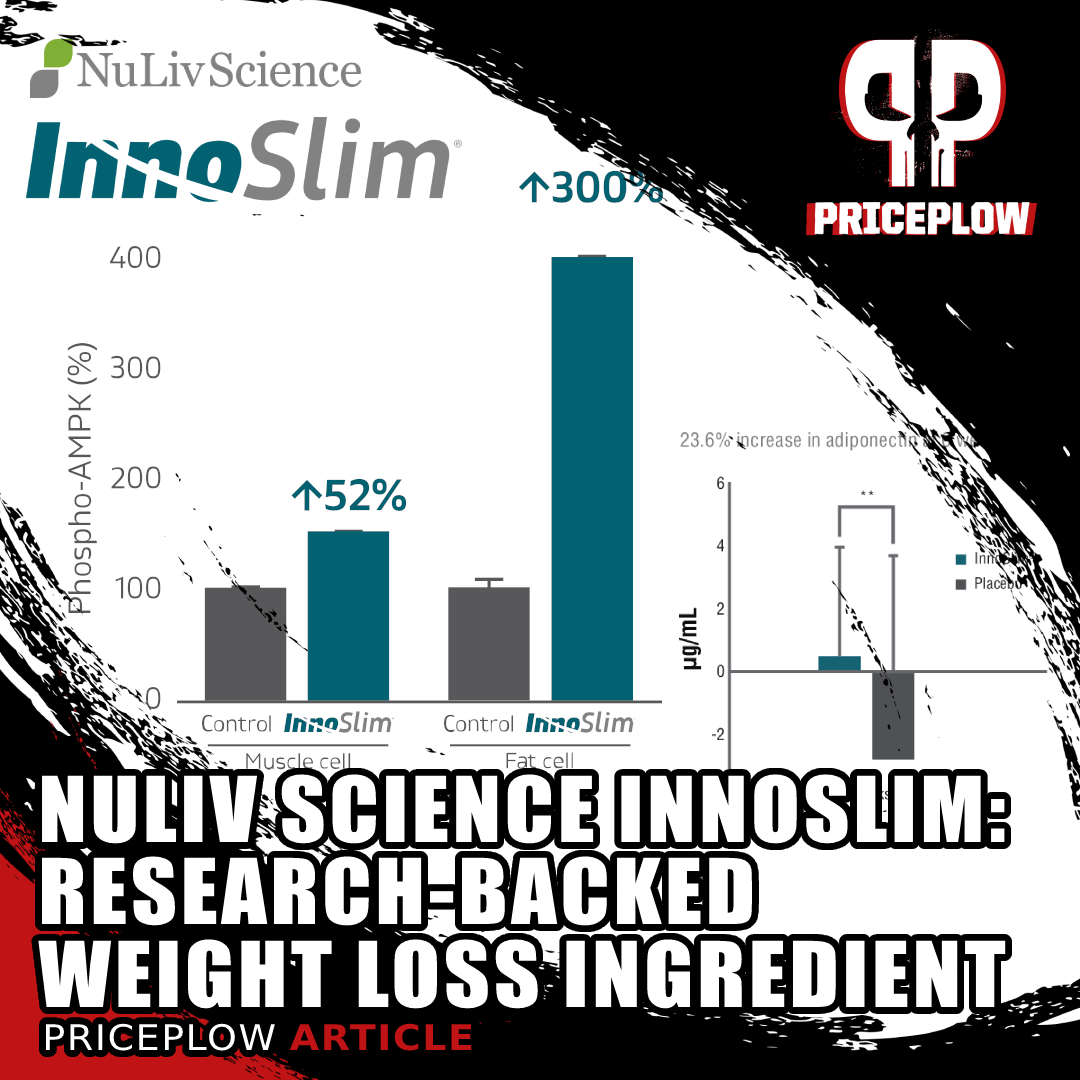
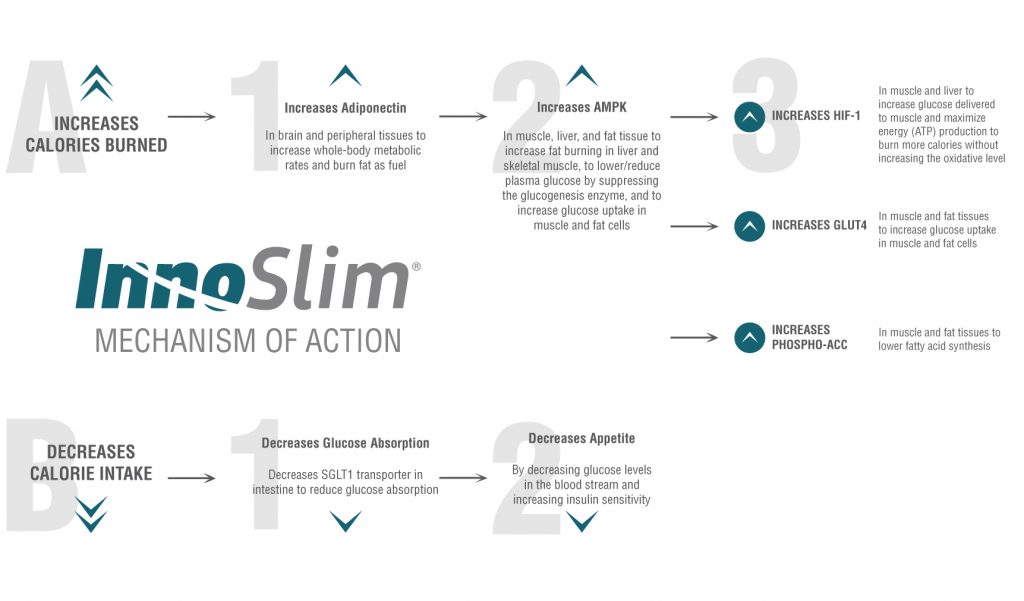
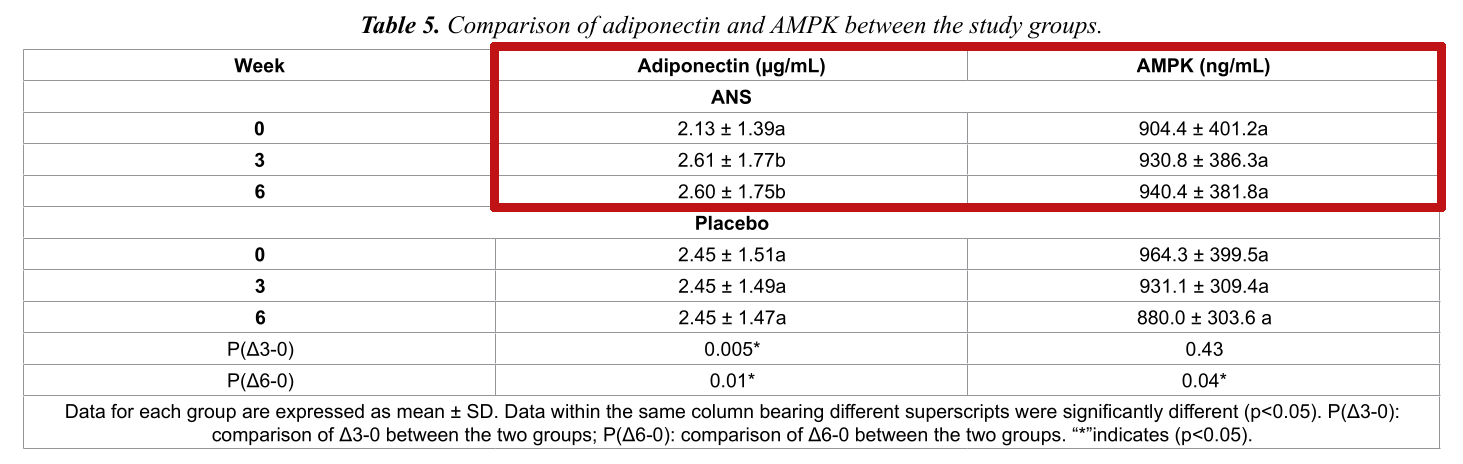
So you might be wondering how the Astragalus + Notoginseng Extract (ANS) supplement was able to trigger such wide-ranging metabolic improvements. The answer appears to lay with adiponectin and AMP-activated protein kinase (AMPK).
Astragalus + Notoginseng Extract (InnoSlim) administration significantly increased subjects' blood levels of adiponectin and AMPK.[5]
AMP-activated protein kinase (AMPK)
Every time you take a breath, make a movement, or contract a muscle, your cells use adenosine triphosphate (ATP). ATP is the base energy used by cells to function, which makes nearly every bodily process highly dependent on it.
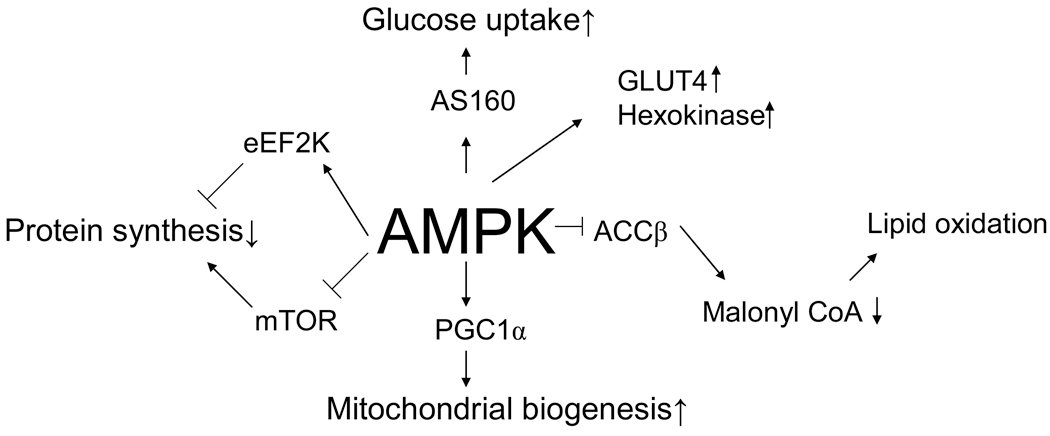
AMPK assists in regulating the AMP/ATP ratio, which is another way of saying it works to maintain energy balance.[27] AMPK kicks in when the body is in dire need of energy, especially when ATP levels fall too much.[28]
Major roles AMP Kinase (AMPK) is proposed to regulate in terms of metabolism and skeletal muscle gene expression.[27]
Due to its direct involvement with ATP production, AMPK finds itself at the center of a number of crucial processes. Chief among them is metabolism regulation – AMPK gets involved in order to boost energy levels, mainly by increasing fatty acid oxidation and glucose uptake.[27] AMPK activation spikes during exercise due to increased energy expenditure.[27] It also seems to be capable of improving symptoms of metabolic syndrome, with research finding that it helps improve insulin sensitivity.[29] There's also evidence supporting the claim that increased AMPK activity can lead to less visceral fat.[27]
It's clear from the data that the astragalus + notoginseng extract raised subjects' AMPK blood levels, an enzyme that drives cellular uptake for glucose and fatty acids.[30] AMPK upregulation is associated with increased insulin sensitivity and improved glycemic control, and is one mechanism behind the metabolic benefits of other popular supplements, prime examples being caffeine and creatine.
As the study indicates, ANS supplementation raised AMPK by about 4%.[5] That's nothing to sneeze at; and like a significant contributor to the study's positive results.
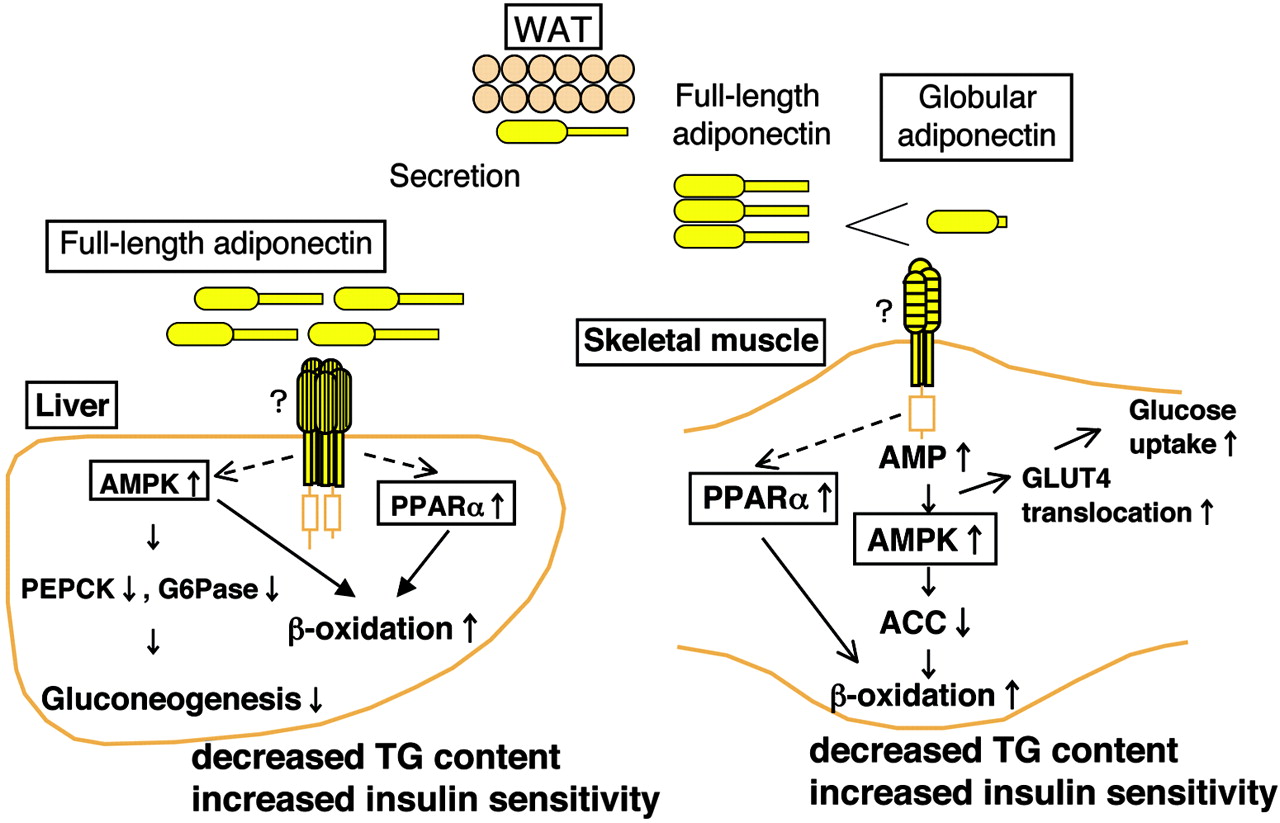
Adiponectin
Adiponectin, on the other hand, is a cytokine hormone. We hear a lot about inflammatory cytokines in supplement science in an overwhelmingly negative context.[31] Since chronic inflammation is driven by the inappropriate upregulation of these cytokines, it's a huge health problem that's linked to much of the metabolic dysfunction that ANS is supposed to address.
But in this case, we have a cytokine that's our friend. Adiponectin is actually anti-inflammatory.[31] It directly increases insulin sensitivity—particularly in the central nervous system.[33]
When it comes to fat oxidation and insulin sensitivity, few things are as powerful as adiponectin. This adipocyte-specific protein boosts fatty acid oxidation and inhibits hepatic glucose production, helping the body properly respond and use its available energy supply.[34] In fact, this hormone is so crucial that it's been directly linked to metabolic issues in multiple ways:[34]
- Low adiponectin increases a person's risk for carrying excessive visceral fat, the particularly harmful type of body fat we discussed above.
- The more adiponectin you have, the lower your blood glucose and the higher your insulin sensitivity.
- Lower adiponectin levels are commonly found in individuals who are in danger of developing type 2 diabetes.
Long story short, reduced adiponectin activity can make you more susceptible to fat gain and blood sugar irregularities, ultimately leading to an array of health problems. As one of the foremost hormones responsible for fatty acid oxidation (i.e. fat burning), keeping adiponectin circulating is extremely important!
So InnoSlim's ability to increase adiponectin levels is exciting!
Adiponectin also improves liver function, which probably helps explain the last thing we want to highlight about this study.
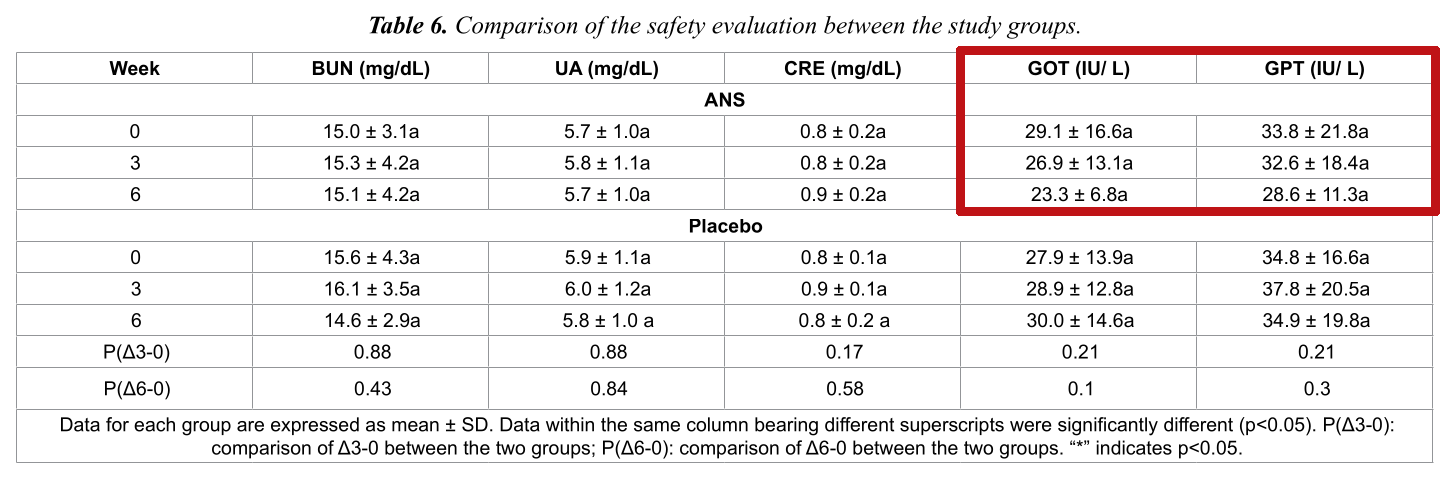
Supplementation with Astragalus + Notoginseng Extract (InnoSlim) improved liver function, as reflected by reduced levels of key liver enzymes.[5]
Glutamic oxaloacetic transaminase (GOT) and serum glutamic pyruvic transaminase (GPT) are liver enzymes. In the US, they're more commonly referred to as alanine transaminase (ALT) and aspartate transaminase (AST).[35]
These are cytosolic enzymes, meaning that under ordinary circumstances, they're enclosed in liver cells. When the liver is damaged, the enzymes leak into the bloodstream. Meaning that elevated blood-enzyme levels are an indication of ongoing liver damage.[35]
Taking the astragalus + notoginseng extract reduced subjects' GOT and GPT levels by about 20% and 15%, respectively.[5]
Since InnoSlim is non-stimulatory, the doors are opened to a multitude of incredible weight loss applications.
The reason this matters is that liver health is a key factor in metabolic health. There's actually a bi-directional relationship between them: liver damage can lead to diabetes and vice-versa.[36] The most famous example of this is probably non-alcoholic fatty liver disease (NAFLD), which is causally associated with metabolic syndrome and diabetes.[37]
Researchers noted no adverse effects from astragalus + notogenseng supplementation.[5]
Granted, this study was conducted with a pretty small sample size – 12 participants. It's definitely a limitation that's important to make note of.
Moreover, study participants' average BMI was about 28, which is considered nearly obese. As a whole, at the outset of the study period, the group showed signs of metabolic derangement. While this is the most relevant group to study when it comes to anti-diabetic supplements, we wonder whether the results could be replicated in healthy people.
All in all, it's a great demonstration of the potential of ANS supplementation.
And the best part of this study?
The ANS (astragalus + notoginseng) extract used was actually InnoSlim by NuLiv Science.
So we have some hard clinical data backing the efficacy of the exact ANS formulation we're writing about. In the supplement industry, that's a pretty big deal – randomized controlled trials, even small ones, are very expensive. Supplement manufacturers really have to go the extra mile to get one done on their product.
Plus, there's no hiding in an RCT. The manufacturers who run these types of trials are simply more highly-respected, not only because of the higher-quality data achieved, but because it's well-known how much time, cost, and business risk is involved. It's encouraging to see that NuLiv Science is confident enough in their work to do this.
-
Huang, Liu, Lin et al., 2021 – Preliminary clinical trial with human arm
Above, we wanted to discuss the human randomized controlled trial first,[5] since it's most relevant to consumers and is the natural headliner.
That study[5] was actually motivated, in part, by a preliminary clinical trial conducted a year earlier by many of the same researchers.[6] Although there's significant overlap between the results of both studies, the preliminary research is still definitely worth discussing.
InnoSlimⓇ is also GRAS, or Generally Recognized as Safe by the FDA, as determined by a panel of experts.
Performed in 2021, the study was conducted in three parts: in vitro, in animals, and with humans.[6] This multidimensional approach to proof-of-concept is common in pilot studies.
In some ways, as a matter of fact, the human portion of this trial was even better than the subsequent 2022 study covered above. For one thing, the sample size was significantly larger, with 21 subjects successfully completing the study.
-
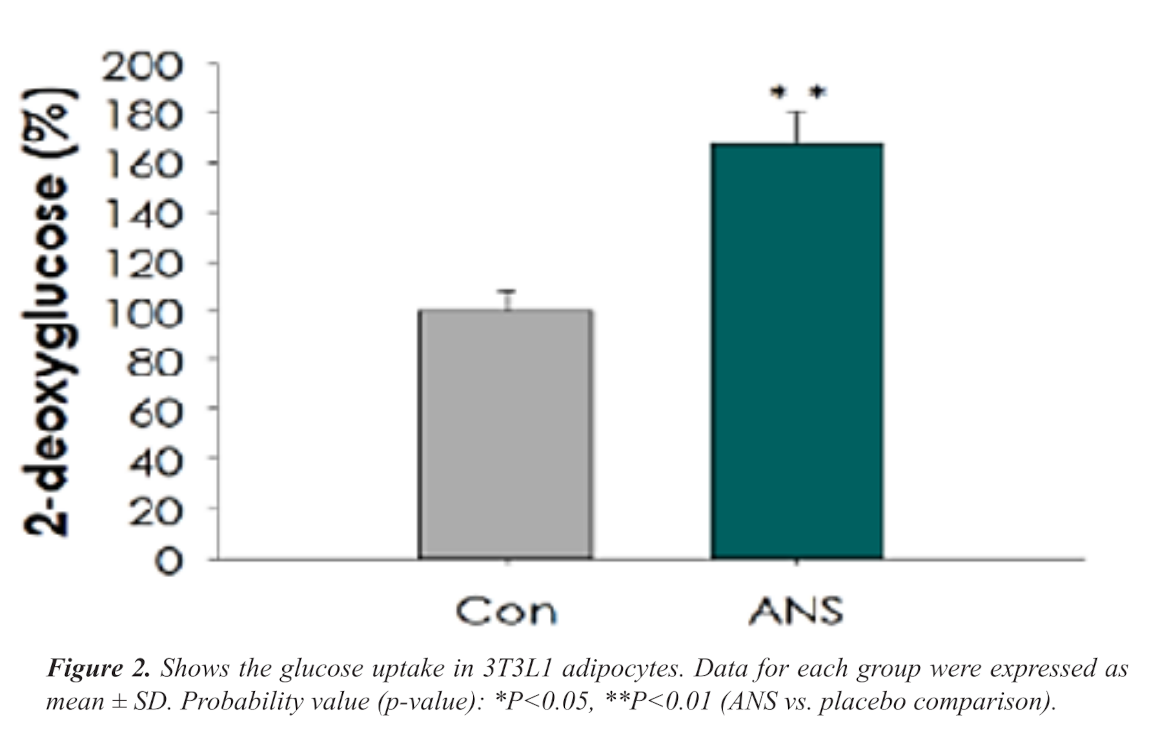
In vitro experiment – cultured fat cells treated with InnoSlim
Since InnoSlim was designed to affect body composition, it makes sense that the researchers would start by studying its effect on fat cells. The technical term for fat cell is adipocyte.
For this experiment, the researchers cultivated their own adipocytes, starting with a pre-adipocytes cell line derived from mice.[6] Following a standard process, the researchers cultured the pre-adipocytes, allowing them to differentiate into mature adipocytes.
Once mature, they were divided into two groups. One was treated with chemicals that induce cellular insulin resistance in order to create a cellular model of the whole-body insulin resistance you'd see in metabolic syndrome or type 2 diabetes. The second group served as the control and was treated with pure DMSO, the solvent used for administering the chemicals.
The insulin-resistant adipocytes were divided into two groups: one was treated with InnoSlim dissolved in DMSO, while the other group got pure DMSO with no InnoSlim. This latter group served as the control for InnoSlim application.
Just to reiterate, there were four distinct groups of adipocytes in the experiment:
- Insulin resistance + InnoSlim group
- Insulin resistance + DMSO group
- DMSO + InnoSlim group
- DMSO + DMSO group
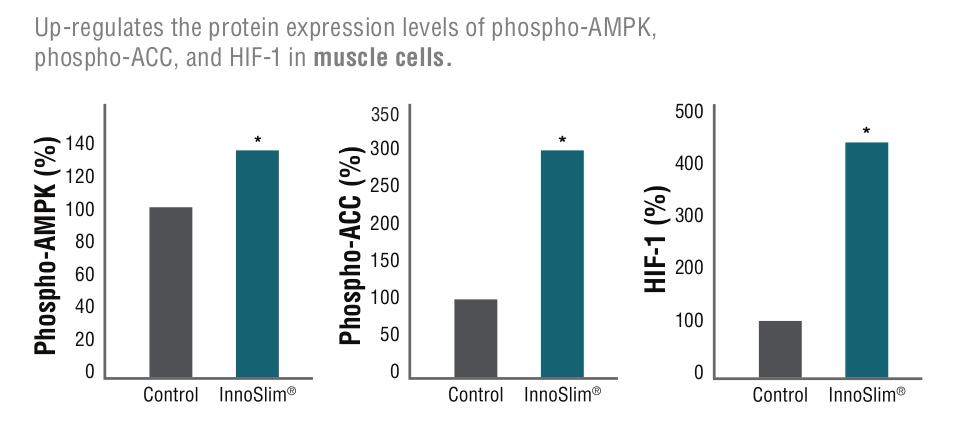
Increased AMPK leads to more greater requirements
The researchers found that, on average, adipocytes treated with InnoSlim had a much higher rate of glucose uptake (68% higher!) than adipocytes that got pure DMSO, thanks to InnoSlim's upregulation of adiponectin and AMPK.[6]
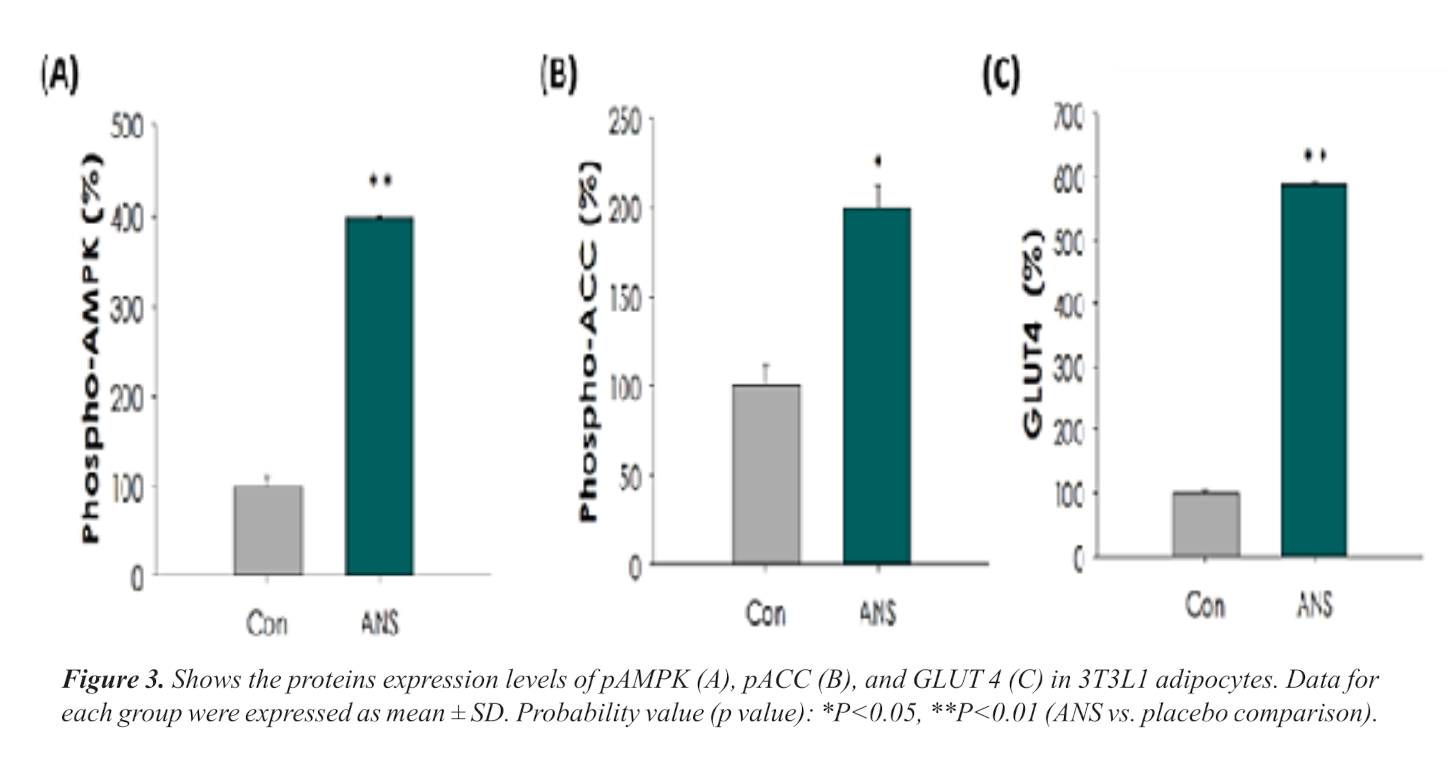
Phosphorylated AMPK levels and glucose transporter 4 (GLUT4) expression was much higher in adipocytes treated with InnoSlim.[6]
That might sound like a bad thing, since glucose uptake by fat cells can increase the addition of new body fat. But bear in mind that glucose uptake is much higher – 2 to 5 times – in isolated adipocytes, compared to in vivo adipocytes.[38]
In other words, the fat cells of real living organisms respond a little differently to glucose, which is partly why the animals in the study lost significant amounts of body fat while supplementing with InnoSlim.[6]
And remember, the systemic metabolic damage caused by metabolic syndrome and diabetes is fundamentally driven by inappropriately high levels of blood glucose. We really want to get that glucose under control, and pretty much any kind of glucose disposal is better than letting it just sit in your blood vessels damaging vascular tissue while your pancreas burns itself out producing too much insulin in response to the glucose.
What we see with the increase of AMPK -- which we sometimes refer to as the "we need energy now" enzyme -- is that the cells are increasing their energy requirements. In vitro, their way of doing this is to take in more glucose that's been made available to them.
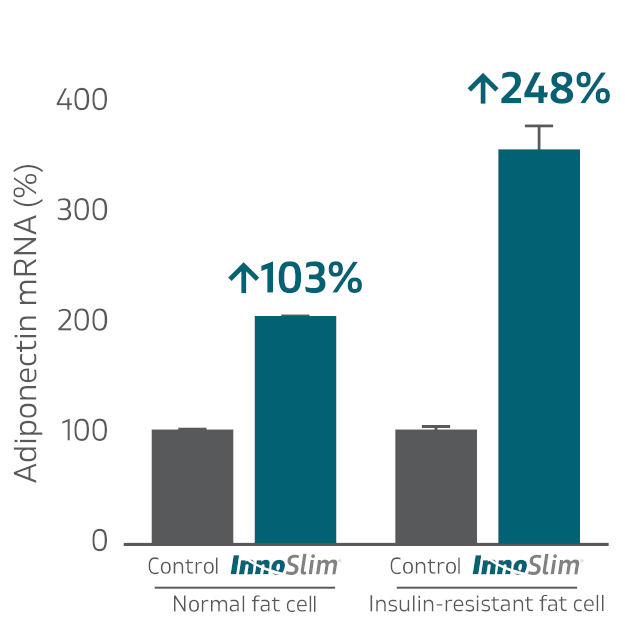
Adiponectin increases in both normal and insulin resistant cells
Concentrations of adiponectin within normal and insulin resistant adipocytes, as measured by mRNA assay.[6]
The results of the in vitro experiment are also very interesting when you look at the adiponectin levels between the different groups of adipocytes. In the insulin resistant adipocytes, treatment with InnoSlim increased adiponectin by a whopping 248%, which illustrates how InnoSlim helps reverse the metabolic dysfunction associated with metabolic syndrome and type 2 diabetes.
But even in the normal adipocytes, which had not been chemically engineered to be insulin resistant, InnoSlim increased adiponectin by over 100%.[6]
Huge potential for healthy human subjects
This suggests that the answer to one of the major questions raised by the study we discussed earlier – namely, "can InnoSlim improve metabolic function in healthy subjects?" – might be yes. It could be the case that InnoSlim is useful as a treatment for helping prevent diabetes onset in genetically susceptible individuals.
The researchers also noted that cells treated with InnoSlim had much higher levels of phosphorylated (activated) AMPK, which, as you'll recall from our earlier discussion, is the natural result of adiponectin upregulation.[6]
Acetyl coenzyme A carboxylase phosphorylation (ACC-P)
We talked a bit about fatty acids, but we've yet to mention one of the body's key factors in metabolizing them – acetyl coenzyme A carboxylase (ACC).This enzyme regulates the formation of fatty acids, controlled via responses from insulin, glucagon, and epinephrine.[39] It's important because it's involved in the first step of fatty acid synthesis.
As you would imagine, ACC is quite active when there's a surplus of calories available, storing this excess energy as body fat. While this is the body's natural response, there seems to be a way to influence it in an advantageous manner.
Images on this page provided courtesy NuLiv Science. This is the first page of their original Fact Sheet published in 2019
Acetyl coenzyme A carboxylase phosphorylation (ACC-P) is an incredibly important limiting factor in all of this. ACC is switched off by phosphorylation, which makes it easier for the body to store fat.[39] Inhibiting ACC-P reduces lipogenesis,[40] putting the body in more of a "fat-burning", as opposed to "fat-storing", state.
We won't get into the role of ACC yet, but it's interesting to note that glucose transporter 4 (GLUT4) was upregulated in the InnoSlim-treated adipocytes. GLUT4 is responsible for actually moving glucose into cells, and GLUT4 under-expression has been identified as a major risk factor for metabolic dysfunction and type 2 diabetes.[41]
Glucose transporter 4 (GLUT4)
GLUT4 is a transporter protein that, unlike the previous two proteins/enzymes, has a much more streamlined responsibility. GLUT4 is in charge of glucose uptake,[11] shuttling glucose from the blood (where it's toxic when overabundant) into areas of the body that need it. Although there are a number of other transporters similar to GLUT4, this particular protein transporter is most involved with both muscular and fatty tissue.[11]
It's easy to see that GLUT4 has a very significant relationship with insulin, moving and acting more efficiently when insulin response is high. Lacking enough GLUT4 in either type of tissue can be dangerous, with issues such as insulin resistance entering the fold.[11]
All in all, GLUT4 works to ensure glucose homeostasis, which is imperative for a healthy, well-running metabolism![11]
Increasing 2-DG (2-deoxyglucose) - An energy restriction mimetic
Finally, let's take a look at what InnoSlim did to cellular concentrations of 2-deoxyglucose (2-DG).
The subject of 2-DG is slightly confusing. 2-DG is a glucose analogue in which one hydroxyl group has been replaced by a hydrogen ion, which renders the molecule incapable of being metabolized by the normal process of glycolysis.[42] Because 2-DG production is closely related to the action of insulin, 2-DG was used as a measure of insulin sensitivity for a long time. Only recently has it been identified as a potential anti-diabetic drug.[42]
2-DG is not a source of energy for cells, and is not metabolized in the same way as glucose. Instead, it's taken up by cells and competitively inhibits the metabolism of glucose, leading to a decrease in energy production. In other words, it restricts cellular energy production. 2-DG has thus been described as belonging to the category of energy restriction mimetics (ERMAs),[43] a class of compounds that imitate the effects of caloric restriction at the cellular level.[44]
You can think of ERMAs not just as a diet pill, but almost like a diet-in-a-pill. Theoretically, an ERMA of sufficient efficacy could cause people to lose weight without requiring them to actually restrict food intake.
Research shows users can experience reduced glucose absorption in the intestine, reduced fat accumulation and inflammation in fat cells, reduced insulin resistance, and overall weight loss. This is the right ingredient for the right time.
The proposed cellular mechanism for this is simple: Since 2-DG restricts cellular energy production, when applied to cells, it causes them to starve to death.[42-44]
However, the science on 2-DG is far from settled. There's at least one peer-reviewed study that argues pretty convincingly that energy restriction can't be the mechanism behind 2-DG's ability to induce cellular catabolism.[45]
The bottom line is that although nobody really knows how it works, 2-DG appears to have significant anti-obesity effects. Animals fed an obesogenic diet treated with 2-DG show significantly lower levels of inflammation and gain much less weight than control animals.[42,43]
-
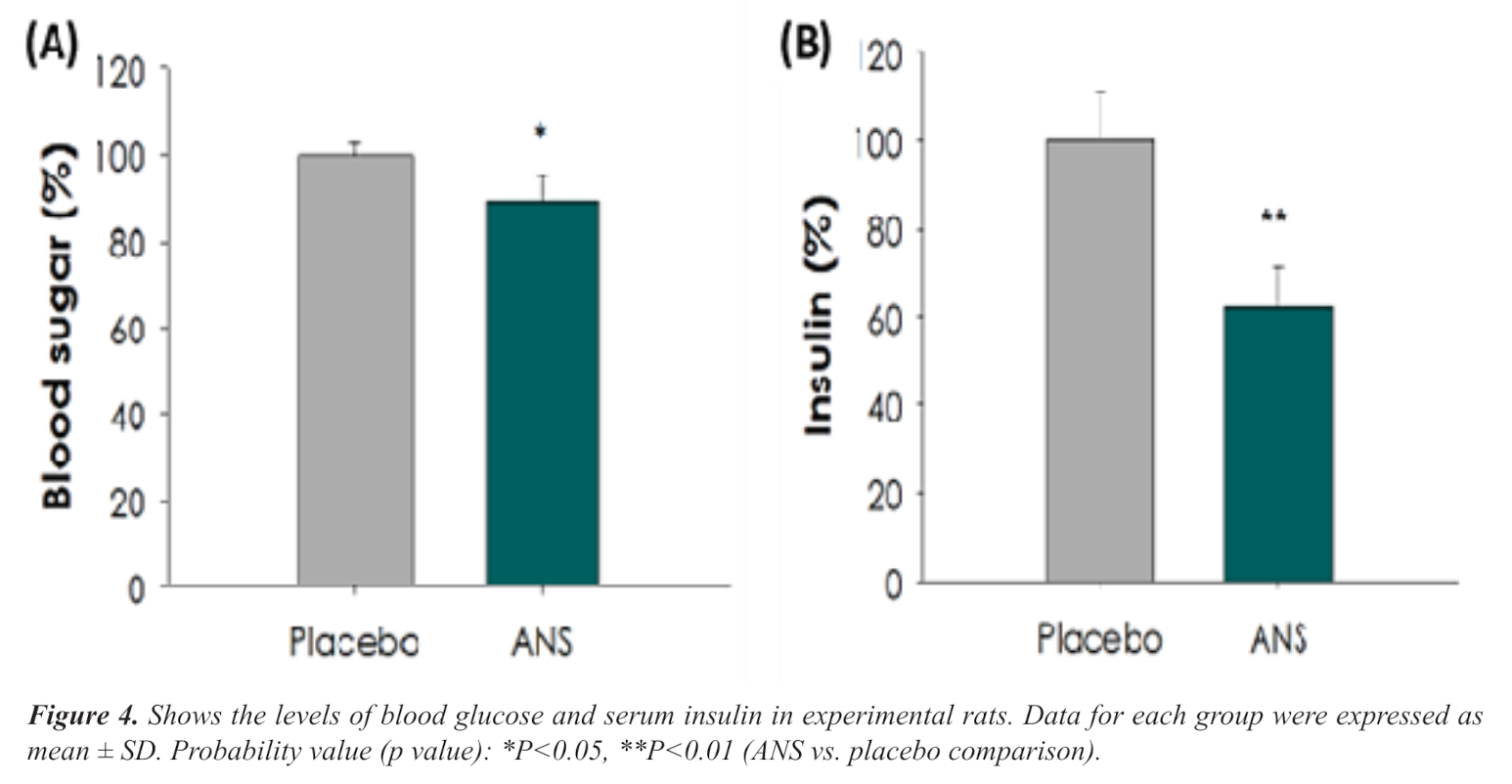
Animal experiment – oral glucose tolerance test (OGTT) in Sprague-Dawley rats
The animal experiment was much more straightforward than the in vitro experiment. For this part of the study, researchers procured 16 male Sprague-Dawley rats and verified with a baseline oral glucose tolerance test (OGTT) that there were no significant metabolic differences between them.
If you're not familiar with the OGTT, it's a pretty simple concept, and used often in human clinical practice. The subject is given a significant dose of glucose and then has their blood drawn at regular intervals to monitor changes in glucose and insulin levels. It's a reliable way to assess metabolic health.
After the initial OGTT, the rats were assigned to either a placebo or InnoSlim group. Each group got its prescribed treatment 12 hours before another OGTT, the idea being to see whether InnoSlim would change the results.
Pre-treatment with InnoSlim significantly reduced average glucose and insulin AUC following an oral glucose tolerance test (OGTT).[6]
AUC (area under the curve) is a metric used in pharmacokinetics to measure the total effect of a drug or substance over time.[46] The math nerds here probably remember that you get the AUC by taking the integral of a mathematical function (the output, in this case, being the blood concentration of whatever you're studying) with respect to time.
We can see from the results that there was about an 11% reduction in glucose area under the curve (AUC), and a whopping 38% reduction in insulin AUC.
A reduction of 38% in the total amount of insulin action during the OGTT is huge. That alone can potentially make the difference between hyperinsulinemia and normal insulin function. And remember, unlike the in vitro experiment, the rats were not treated to induce insulin resistance beforehand. These were normal, metabolically healthy animals that showed an impressive improvement.
So again, we see that InnoSlim is not necessarily just for people with existing metabolic dysfunction. Theoretically, we might be able to use this as a prophylactic against metabolic syndrome and diabetes.
-
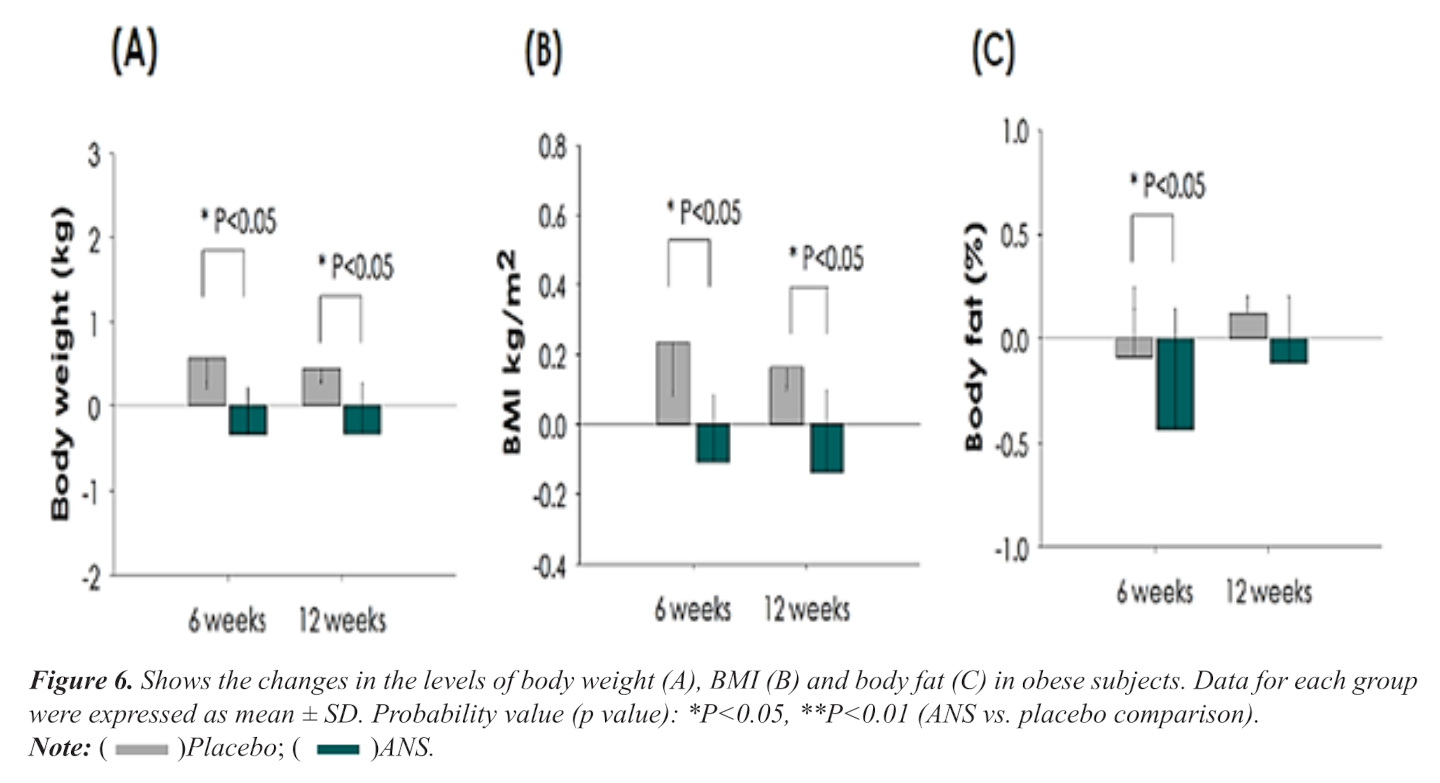
Human clinical trial – 2 phase, 12 week crossover study
That brings us to the 2021 human portion of the experiment.[6]
The design was similar to the 2022 crossover study we discussed earlier[5] – subjects served as their own controls by completing an active phase and a placebo phase, separated by a washout period.
Each of the two study phases lasted 12 weeks with a 4 week washout period. Blood samples were taken every 6 weeks.
During the InnoSlim phase of the experiment, obese subjects saw significant reductions in body weight, BMI, and body fat percentage.[6]
Similar improvements to cholesterol and triglycerides were noted in this study as to the 2022 study,[6] albeit the effect size was a bit smaller.
The really interesting thing about this study is that clear reductions in body weight, body mass index (BMI), and body fat percentage were observed in subjects who took InnoSlim![6]
-
These two studies[5,6] were not here when we first wrote about InnoSlim on this page in 2019. We were already confident in the ingredient, but this data puts it over the top, especially given the endpoints of weight loss combined with the correction of metabolic biomarkers that we actually care about (insulin, triglycerides, HDL, and more).
For many, these two studies are all you need to see. For others, especially ingredient formulators, there's more digging to be done. What's going on under the hood?
Ginsenoside Research
The studies we just discussed are particularly interesting because they were conducted on InnoSlim specifically.

What are the differences in these NuLiv Science ingredients that use similar plants? In another article, we dive into the Astragalosides and Ginsenosides inside, and break down the different constituents of four of NuLiv Science's major sports nutrition ingredients
InnoSlim consists of many different bioactive constituents – it's a combination of extracts, after all. But there's one class of molecules that seems to be disproportionately responsible for the health benefits of the ginseng part of InnoSlim, and that's the ginsenosides, steroid glycosides and triterpene saponins that occur naturally in the ginseng plant.[47]
As NuLiv Science brought InnoSlim to market, the formulators were guided by key research on the benefits of isolated ginsenosides. We'll take a quick look at some of this research, as it can help us understand the significance of the studies we just discussed.
Upregulate adiponectin, AMPK and ACC-P
A 2013 study found that when cultured liver cells were exposed to a ginsenoside concentration of 0.1 micrograms/mL in a 24-hour saturation period, mRNA levels of adiponectin increased by 203%.[48] Furthermore, effects on insulin-resistant cells were even more pronounced. In these cells, adiponectin activity increased by 348%.[48]
By increasing ginsenoside dosing from 0.001 micrograms/mL to 1 microgram/mL, scientists saw that AMPK activity increased from 300% to 400%.[48]
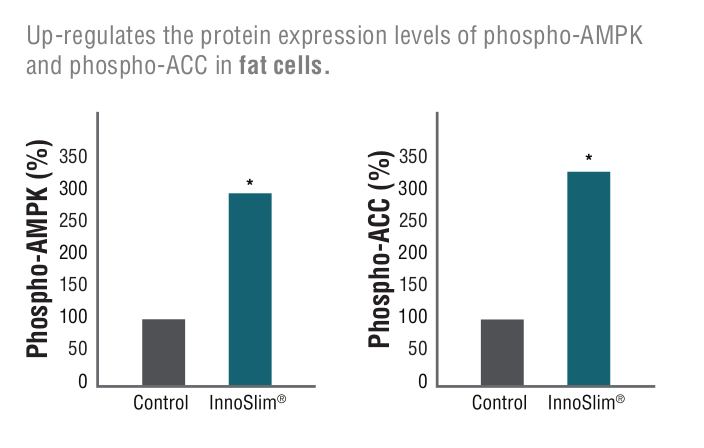
AMPK upregulation in fat cells means the capability for more energy and fatty acid oxidation where it matters most![48]
Finally, ACC-P expression increased from 200% to 350% of baseline.[48]
This stimulation bodes well for metabolic health. As this study was specifically concerned with liver cells, such increases in AMPK and ACC-P can increase fatty acid oxidation while suppressing hepatic glycogenesis and lipogenesis.[48]
Help reduce glucose absorption
The effects of InnoSlim are arguably most prominent when discussing glucose absorption.
After all, how the body reacts, responds, and deals with glucose sets the table for how well it's functioning as a whole. Handling glucose in efficient ways, such as through insulin sensitivity, is a major component of keeping things like fat gain and liver damage to a minimum.
To understand how InnoSlim can help us efficiently dispose of ingested glucose, it behooves us to take a look at the research showing ginsenosides' effects on glucose absorption.
Sodium-dependent glucose cotransporter 1 (SGLT1)
The first opportunity for glucose to enter the bloodstream is in the digestive tract. And while we ultimately want glucose to reach cells and fuel them, we don't want this to happen too fast. High elevations in blood glucose levels after meals can increase the risk of diabetes.[31]
SGLT1 operates in a similar fashion to GLUT4, however, it does have some slight differences. First, it primarily works within the digestive tract to transport both glucose and galactose, a sugar native to dairy products.[49] Second, and perhaps most importantly, SGLT1 is sodium-dependent, meaning it relies on the presence of salt to conduct its work.
That being said, SGLT1's involvement with blood sugar aligns it closely with GLUT4 in terms of effects. Not only is SGLT1 a part of the first step of converting sugars into energy, but more SGLT1 activity has been linked to better insulin response and energy balance.[49]
This makes intestinal SGLT1, which are the body's first-available glucose transporters, extremely important. Reducing glucose absorption by inhibiting SGLT1 can help maintain regular blood sugar levels, ultimately helping keep metabolic syndrome at bay.
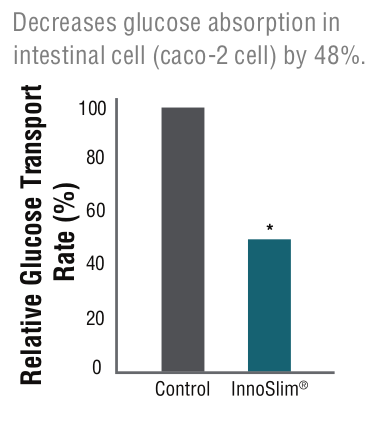
Research shows that InnoSlim causes the small intestine to absorb less glucose into the bloodstream,[50] helping prevent more glycemic issues in the first place
In a 2007 in vitro study published in the Journal of Agricultural and Food Chemistry, researchers tested the effects of InnoSlim on glucose uptake in human Caco-2 cells. They treated cellular systems with multiple concentrations of the ingredient (0.01 micrograms per milliliter (mcg/ml), 0.10mcg/ml, and 1.00mcg/ml), comparing the rate of glucose transport in each model with a control group.[50]
Using the 0.10mcg/ml as the primary measuring model, they found that InnoSlim reduced Caco-2 glucose absorption by 42%.[50]
Diving deeper, the researchers found that the ingredient accomplishes this by inhibiting SGLT1 mRNA protein expression, with the 0.10mcg/ml concentration downregulating transporter activity by 25%. They also observed a dose-dependent effect, too — higher concentrations yielded larger reductions in absorption and SGLT1 activity.[50]
HIF-1
While it may not be involved directly with metabolic processes, hypoxia-inducible factor-1 (HIF-1) surely has a substantial indirect role. Essentially, this factor maintains cellular homeostasis, specifically when instances of hypoxia (low oxygen) or low energy are of concern.[51]
HIF-1 increases the expression of vascular endothelial growth factor (VEGF), a protein that causes new blood vessels to grow. The growth of new blood vessels, called vascularization, is necessary for fat cell proliferation – after all, new fat cells can't survive without an adequate supply of blood.
The glucose that does make it through the intestines has a better chance of going where we want it to go - into the muscle cells![52]
For this reason, inhibiting HIF-1 can prevent weight gain.[53]
And as it turns out, ginsenosides inhibit HIF-1. A study from 2020 found that inhibiting HIF-1 through application of a ginsenoside solution prevented cellular proliferation in vitro.[54]
TNF-⍺ and PAI-1
Finally, these last three cofactors and enzymes all share similar relationships as far as InnoSlim is concerned, especially in terms of body fat.
Tumor necrosis factor-alpha (TNF-⍺) is an inflammatory cytokine that tends to be overexpressed in cases of metabolic syndrome. Because it's mainly held in adipose tissue, increased levels of fat tend to increase the amount of TNF-⍺ present. Increased TNF-⍺ raises a person's risk for insulin resistance, obesity, and other markers of metabolic syndrome.[55] Fortunately, ginseng extracts have been shown to decrease TNF-⍺ production.[56]
Plasminogen activator inhibitor-1 (PAI-1), a biomarker in the fibrolysis system, has displayed a positive correlation to visceral body fat, poor insulin response, and inflammation.[57,58]
Your body produces PAI-1 in response to TNF-⍺, and ginsenosides don't just decrease TNF-⍺ expression – they can also stop the the production of PAI-1.[59]
InnoSlimⓇ is also GRAS, or Generally Recognized as Safe by the FDA, as determined by a panel of experts.
In other words, ginsenosides both decrease the production of the inflammatory cytokine TNF-⍺, and help limit the damage it causes.
Glucose transporter 4 (GLUT4)
Other research has shown that ginsenosides can increase muscular glucose uptake rate by over 100%,[52] effectively doubling the speed at which muscular cells can absorb the sugar. Considering this same study found increased GLUT4 activity as well,[52] we can deduce that this muscle-based glucose transporter was upregulated due to this novel formula!
Upregulation of GLUT4 also promotes more glucose uptake in adipocytes – which sounds like a bad thing, but this can actually help regulate blood glucose activity in fat cells, which thus maintains stable blood sugar levels.[60]
If you're interested in more underlying research, you can also read our article titled Astragalosides and Ginsenosides: Differentiating NuLiv Science's Ingredients.
Innoslim Supplements: Weight Loss Aids with InnoSlim Inside
Given its potent fat-burning, insulin sensitivity-boosting effects, InnoSlim is an extremely attractive ingredient for weight-management products. Its non-stimulatory nature makes it even more versatile, capable of being added to any formula. Thus, InnoSlim can fit neatly into fat-burners (both stimulant-based and stimulant-free), glucose disposal agents (GDAs), carnitine supplements, and other products.
Here are some of our favorite products that put InnoSlim to use:

If your goal is fat loss, InnoSlim-powered Glaxon Thermal is a great addition to your supplement stack!
- Glaxon Thermal: A non-stimulant weight management aid in a flavored powder drink mix. In Thermal, InnoSlim works alongside other ingredients to activate fatty acid oxidation and increase energy expenditure, yet without caffeine. Beware, however, it does contain GBB, an ingredient known to increase sweat production.
- Alpha Lion Apex Burn: A stimulant-based fat burning drink mix that includes InnoSlim alongside a timed-release blend of caffeine and other thermogenic ingredients for a smooth lift of energy and metabolism.
- Healthgevity Ignite: A powerhouse metabolic-enhancing formula marketed towards healthcare practitioners who are on the front lines of the obesity epidemic. It includes a dual dose of the potent glucose disposal agent, berberine (and its more powerful metabolite, dihydroberberine). This is a stimulant-free, capsule-based product.
Of course, this list isn't all-inclusive. Because of its various capabilities, it's likely you'll find InnoSlim in other formulas, too. Below is a list of articles on the PricePlow Blog covering InnoSlim:
All InnoSlim Articles on PricePlow
Conclusion – InnoSlim Is More Than a Metabolic-Booster
Fat burners and weight-loss aids receive quite a lot of attention in supplements as consumers search for the best ways to support healthy body weight and body composition. And let's face it, whether you're a bodybuilder looking to lean-out for a competition or a weekend warrior that wants to get in better shape, many of us have tried dropping a few pounds of body fat at some point.

As a part of a healthy diet that assists with the same hormones, proteins, and enzymes, InnoSlimⓇ can have a major impact and we hope to see it in more supplements.
A healthier body weight, balanced body composition, and optimal metabolic health have comprehensive effects that extend past "shape" — these things put us in a better position to fight inflammation, optimize immune function, and support longevity. In other words, weight management lends itself more to overall health than some may think.
Optimizing your diet and training regimen are two of the best ways to pursue these endeavors and improve your health. Once these are taken care of, you can then look into other areas for additional gains —from sleep hygiene to stress management, and, of course, metabolic health. InnoSlim from NuLiv Science looks at the latter, activating mechanisms in the body to improve glucose uptake and blood sugar levels, increase energy expenditure, regulate appetite, and support weight management.
InnoSlim's capabilities make it an excellent ingredient to include in a weight-focused regimen, yet its relevance doesn't stop there. Influencing the metabolism on multiple fronts allows it to support overall health, too. This makes NuLiv Science's InnoSlim a powerful ingredient, one that we hope to see in even more formulas across sports supplements.







Comments and Discussion (Powered by the PricePlow Forum)