Most supplements force your liver to work overtime, but BHB ketones actually generate energy for liver cells! New research shows exogenous ketones deliver ketosis benefits without the liver damage from high-fat diets.
Here's a paradox that might surprise you: while many dietary supplement ingredients force your liver to work overtime, exogenous ketones actually support liver health by generating cellular energy rather than depleting it! This flies in the face of conventional wisdom about supplements and liver burden -- but groundbreaking new research reveals that not all exogenous compounds are created equal when it comes to hepatic metabolism.
About a decade ago, the ketogenic diet gained massive popularity for its potential benefits in weight loss, mental clarity, and various therapeutic applications. By severely restricting carbohydrates to roughly 50 grams per day and dramatically increasing fat intake, keto diets force the body into a metabolic state called ketosis, where it breaks down fat into ketone bodies for energy, providing an alternative to glucose.
Ketones are Great, But is a High-Fat Diet the Healthiest Way to Get Them?
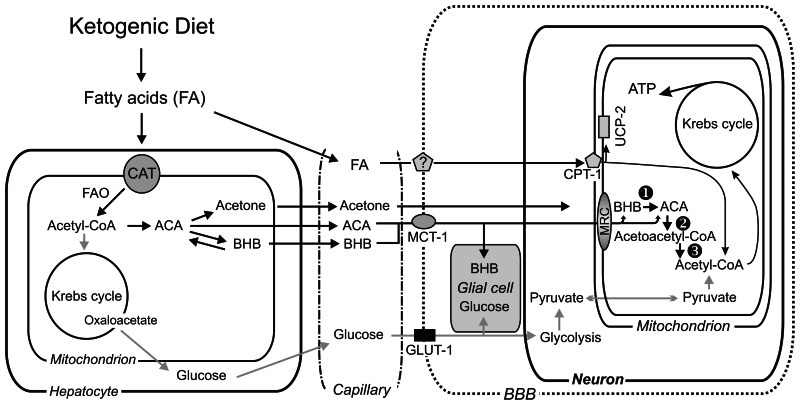
This metabolic shift offers many benefits. Ketone bodies provide an efficient, stable energy source that produces fewer reactive oxygen species than glucose metabolism. They enhance mitochondrial function, reduce inflammation, and provide neuroprotective effects. The positive results stem from a mixture of the ketones themselves and the restriction of excess carbs, but it's become clear that the ketones are providing a great deal of the benefits.
But here's where things get complicated: while high-fat diets effectively generate beneficial ketones, mounting research reveals such diets simultaneously damage the very organ responsible for producing them -- the liver!
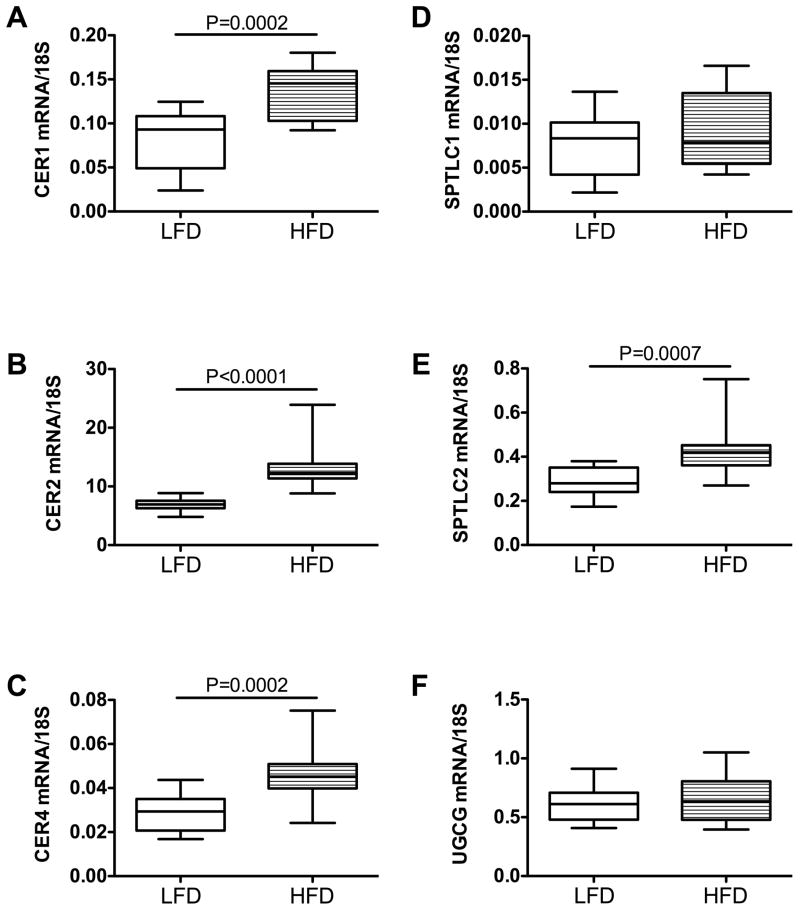
High-fat diets can trigger liver insulin resistance within just three days, increase toxic ceramide production, and overwhelm hepatic processing capacity even when using "healthy" fats. This creates a fundamental dilemma: how do we access the research-backed benefits of ketone metabolism without subjecting our liver to potentially harmful dietary extremes?
Beyond Dietary Extremes: The Exogenous Ketone Advantage
What if you could capture the metabolic benefits of ketosis without adhering to the restrictive and potentially liver-damaging ketogenic diet? This is where exogenous ketone supplementation enters the picture. Rather than forcing your body into ketosis through extreme dietary restriction, you can directly provide ketone bodies -- specifically beta-hydroxybutyrate (BHB) as -- through targeted goBHB supplementation.
This approach offers several advantages. You maintain dietary flexibility while still accessing ketone-mediated benefits. You avoid the potential compliance issues and social challenges that come with strict ketogenic eating. And most importantly for liver health, you're choosing a metabolic fuel that actually supports hepatic function without burdening it.
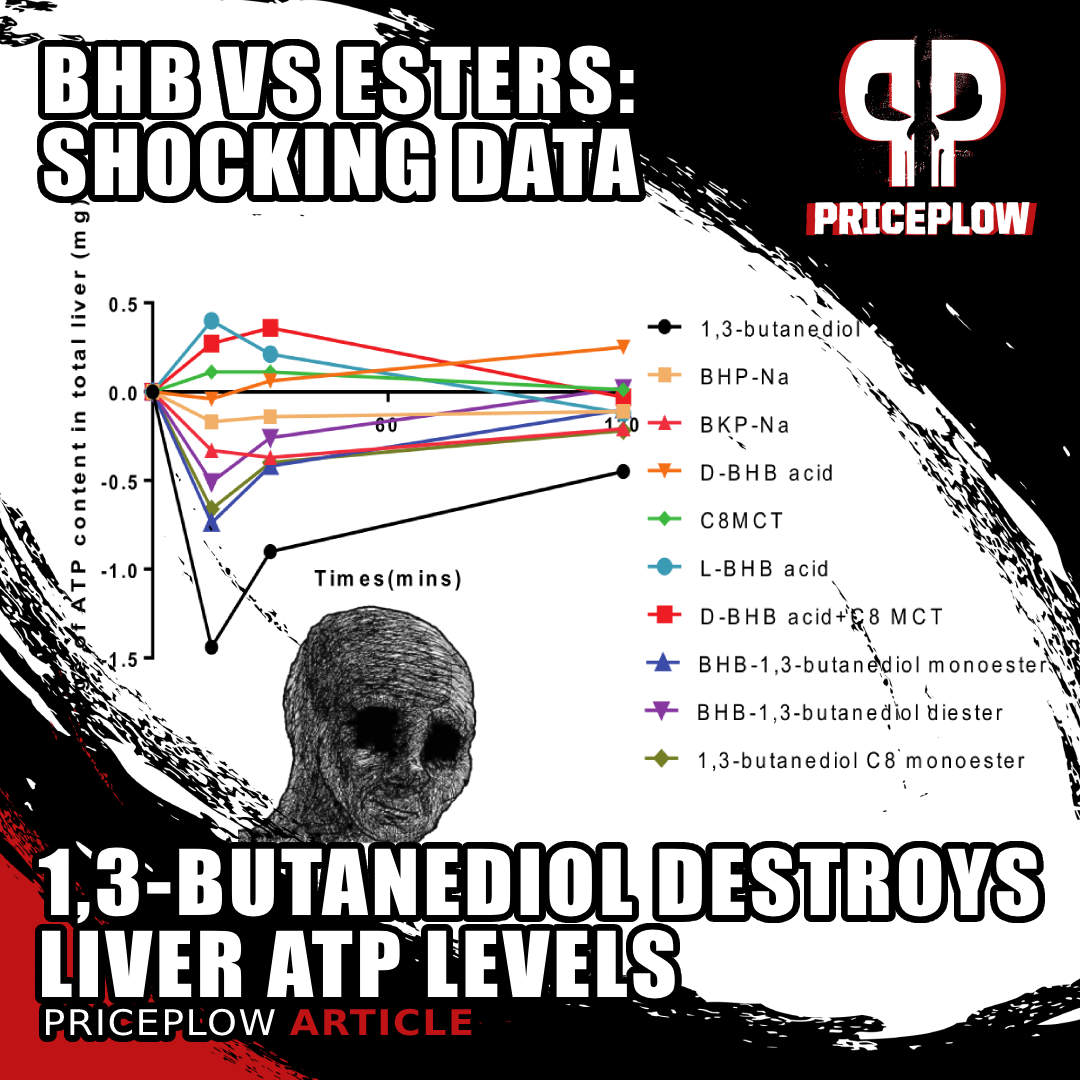
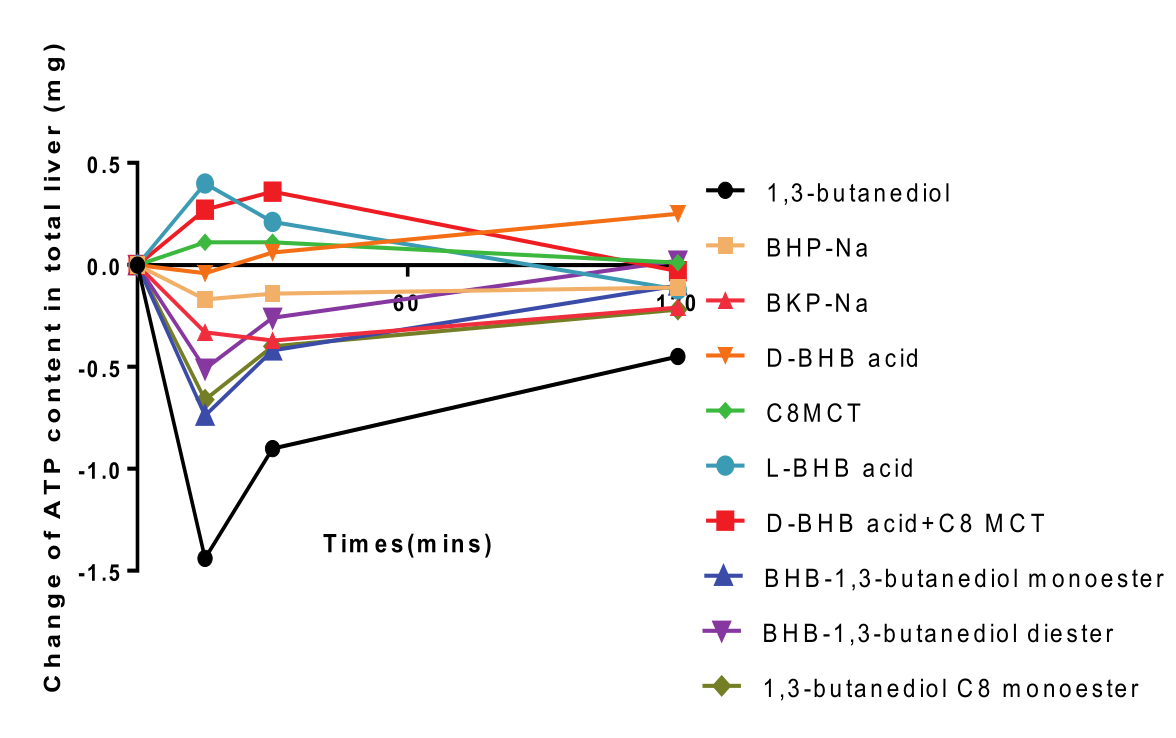
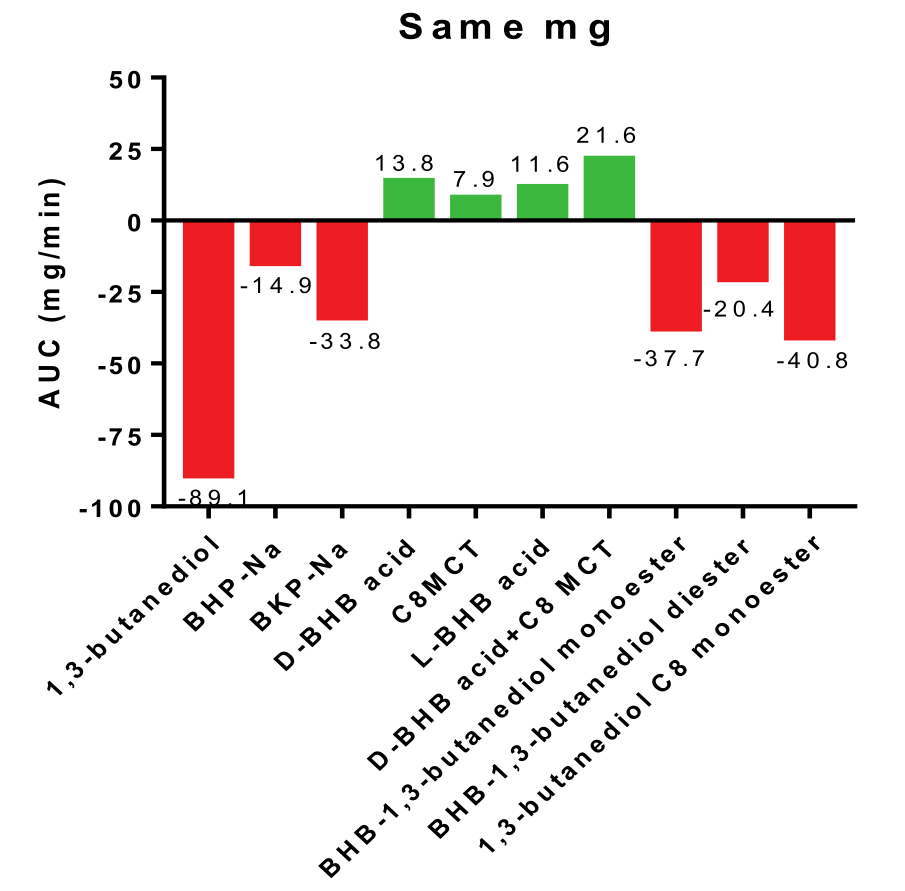
New unpublished preclinical data shows that 1,3-butanediol is a net ATP consumer in the liver, as opposed to free acid BHB and MCT which are ATP (energy) producers.[1] This sheds a whole new light on the BHB vs. Ketone Esters.
Recent internal research from NNB Labs has revealed that BHB free acid is a net producer of ATP in liver tissue, meaning it actually generates cellular energy during its metabolism. This finding turns conventional supplement wisdom on its head. While most exogenous compounds require the liver to expend energy for processing and detoxification, high-quality exogenous ketones like goBHB actually deliver energy to liver cells.
A Smarter Approach to Metabolic Health
The key lies in choosing the right form of exogenous ketones. Not all ketone supplements support liver health equally, and some may actually work against it. The difference between liver-supporting and liver-burdening ketone sources comes down to their specific metabolic processing requirements and energy costs in hepatic tissue.
So instead of viewing supplements as necessary burdens that the liver must process, we have identified compounds that actually support optimal liver function while delivering their intended benefits. This article gets into the details and cites sources on everything described above.
But before we go further, sign up for PricePlow's coverage of Ketone Labs and goBHB for cutting-edge science and industry insights:
Subscribe to PricePlow's Newsletter and Alerts on These Topics
The Liver’s Energy Economy: Why ATP Production Matters
To understand why exogenous ketones can be healthy for the liver, we need to think of the liver as the body's metabolic headquarters -- a bustling energy factory that processes every compound we consume.
You can think of the liver as three things for your body, all in one:
- Chemical production factory
- Sewage processing plant
- Waste storage facility
Unlike other organs that can be selective about what they metabolize, the liver must process everything that enters your system (including things put on your skin), making its energy efficiency absolutely critical for long-term health. It is truly the seat (or foundation) of your body's overall condition.
-
The Liver: Your Body’s Metabolic Processing Plant
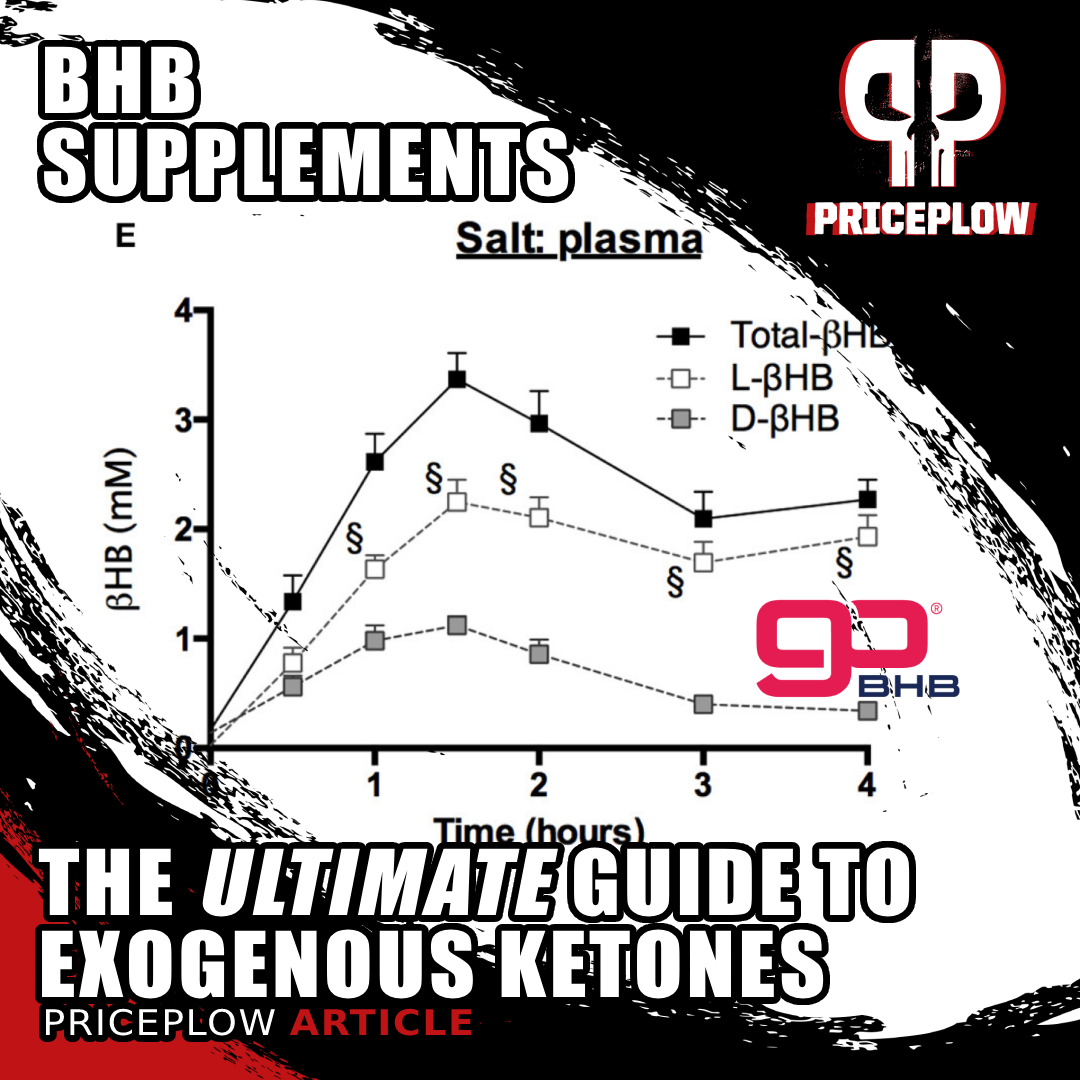
When you consume any exogenous ketone supplement, your liver becomes the primary site where these compounds undergo conversion into bioavailable ketone bodies that can circulate throughout your bloodstream. Each type of ketone source -- whether it's BHB free acid, BHB salts, MCT oil, or alcoholic ketone esters -- carries its own unique "energy cost profile" as it moves through the liver's conversion processes.
This is where things get interesting from a metabolic efficiency standpoint. Some compounds require significant energy investment during their hepatic processing, while others actually generate net energy for liver cells. The difference between an ATP producer and an ATP consumer in the liver can determine whether a supplement supports or burdens hepatic function.
Think of ATP as cellular currency: it's the universal energy that powers every biochemical process in your liver cells. When ATP levels are high, liver cells can efficiently perform detoxification, protein synthesis, glucose regulation, and countless other vital functions. When ATP gets depleted, cellular processes begin to break down, setting the stage for metabolic dysfunction.
-
The Fructose Precedent: How ATP Depletion Damages the Liver
The most well-documented example of how hepatic ATP depletion can cause serious liver damage comes from fructose metabolism research. Unlike glucose, which can be metabolized by cells throughout the body, fructose must be processed primarily in the liver -- and this processing comes with a steep energy cost.
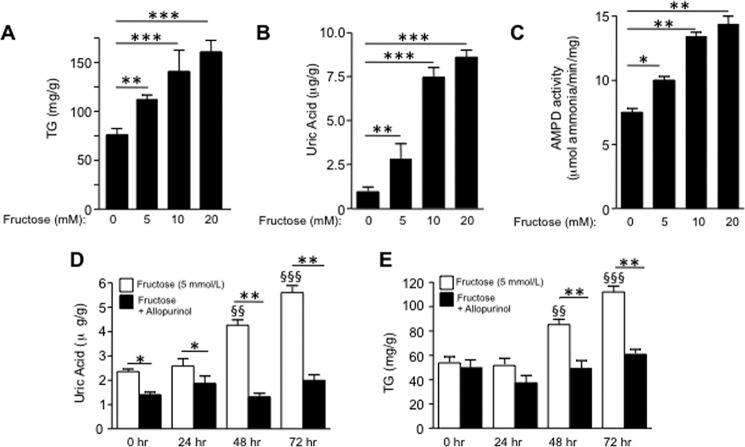
Watch how fructose wreaks havoc on your liver in real-time. Within hours, it spikes triglycerides and uric acid while crushing ATP/ADP ratios -- your liver's energy currency. The allopurinol comparison shows that blocking uric acid production can partially prevent this metabolic disaster, proving the toxic cascade starts with ATP depletion.[2]
When fructose enters liver cells, it bypasses normal glycolytic regulation and gets rapidly phosphorylated, consuming large amounts of ATP in the process.[3] This ATP depletion triggers a cascade of problems: elevated uric acid production, mitochondrial oxidative stress, and inflammatory damage that promotes fatty liver disease.[2]
-
The Universal Principle: ATP Consumers vs. ATP Producers
The fructose example establishes a crucial principle that extends beyond just one problematic sugar: any compound that depletes hepatic ATP reserves can contribute to liver dysfunction through similar mechanisms. The metabolic disruption, oxidative stress, and inflammatory cascade triggered by ATP depletion represent common pathways through which various hepatic stressors damage liver tissue.
This is why the concept of "net hepatic ATP production" becomes so important when evaluating supplements and dietary compounds. Rather than just asking whether something can be metabolized by the liver, we should be asking: Does this compound give energy to liver cells, or does it take energy away?
When we view supplement choices through this lens, a clear strategy emerges: we want to consume compounds that serve as net hepatic ATP producers while avoiding those that function as net ATP consumers. This approach prioritizes liver health at the cellular level, supporting the organ's ability to perform its countless essential functions while minimizing metabolic stress.
Understanding this fundamental principle sets the stage for appreciating why certain exogenous ketone sources represent such a breakthrough in liver-friendly supplementation, and why other ketone sources or high-fat diets, despite producing beneficial ketones, create the opposite problem by overwhelming the liver's processing capacity.
BHB: The Liver’s Preferred Energy Source
Groundbreaking research from NNB Labs has revealed something remarkable: beta-hydroxybutyrate (BHB) free acid actually generates cellular ATP during its metabolism.[1] This discovery fundamentally changes how we should view exogenous ketone supplementation, positioning high-quality BHB as a liver-supportive compound rather than just another supplement that the liver must process.
-
The Direct ATP Production Advantage
When you examine the internal study's results, the contrast between different ketone sources becomes immediately apparent. D-BHB free acid demonstrated a gradual, sustained increase in liver ATP over the 120-minute measurement period.[1] Unlike compounds that require energy-intensive metabolic conversion, BHB requires minimal processing before becoming bioavailable -- it enters liver cells and can be directly utilized for energy production.
Three Steps Instead of Glucose’s Eleven
This efficiency stems from BHB's unique metabolic pathway. While glucose metabolism requires eleven biochemical steps to enter the Krebs cycle, BHB needs only three steps to convert to acetyl-CoA, the fundamental energy molecule that powers cellular respiration. This streamlined pathway means less metabolic overhead with fewer byproducts and more net energy production for liver cells.
If this study[1] is to be confirmed, 1,3-butanediol is what we consider to be straight-up liver poison.
The research also demonstrates that ketone-driven ATP synthesis produces significantly fewer reactive oxygen species (ROS) than glucose-driven metabolism.[5] This reduced ROS production explains much of the antioxidant effect associated with ketone metabolism -- you're getting clean, efficient energy production with minimal oxidative stress as a byproduct.
-
The Synergistic Power of Strategic Combinations
The NNB Labs research revealed another major finding: the combination of D-BHB free acid with C8 MCT produced the highest liver ATP yield of all tested compounds.[1] This synergistic effect suggests that strategic pairing of ketone sources can optimize hepatic energy production beyond what either compound achieves alone.
The mechanism behind this synergy likely involves dual energy pathways: D-BHB provides immediate, direct ATP while C8 MCT rapidly converts to additional ketone bodies, creating both immediate and sustained energy support for liver cells. This represents a sophisticated approach to liver-friendly supplementation that goes beyond simply avoiding hepatic burden.
-
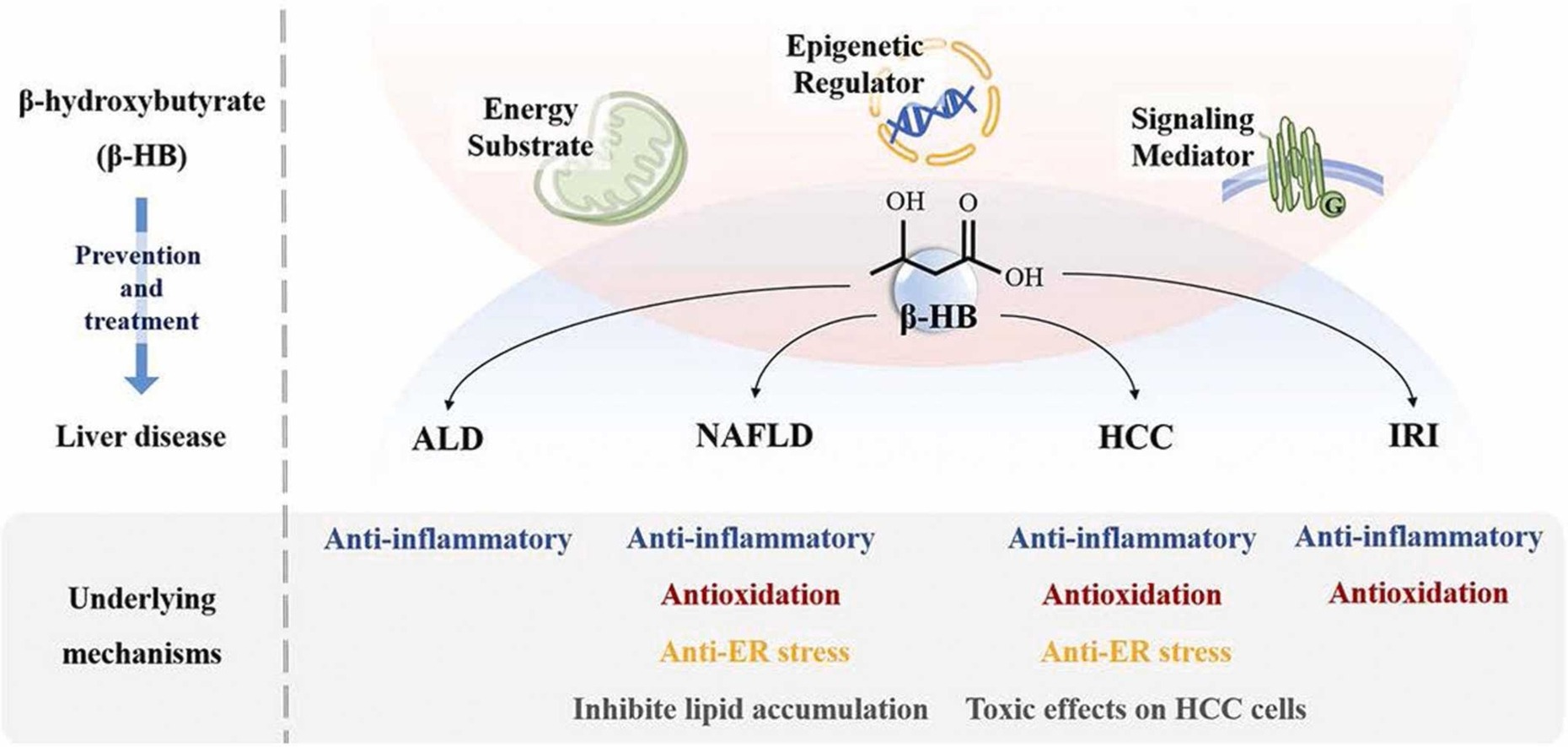
Beyond Energy: BHB’s Additional Liver Health Benefits
BHB isn't just an energy source -- it's a signaling molecule that activates protective genes and blocks inflammatory pathways. By binding to specific receptors like GPCRs and inhibiting harmful proteins like HDAC, it helps your cells function optimally while reducing oxidative damage.[6]
While the ATP production benefits of BHB are impressive, they represent only part of the liver health story.
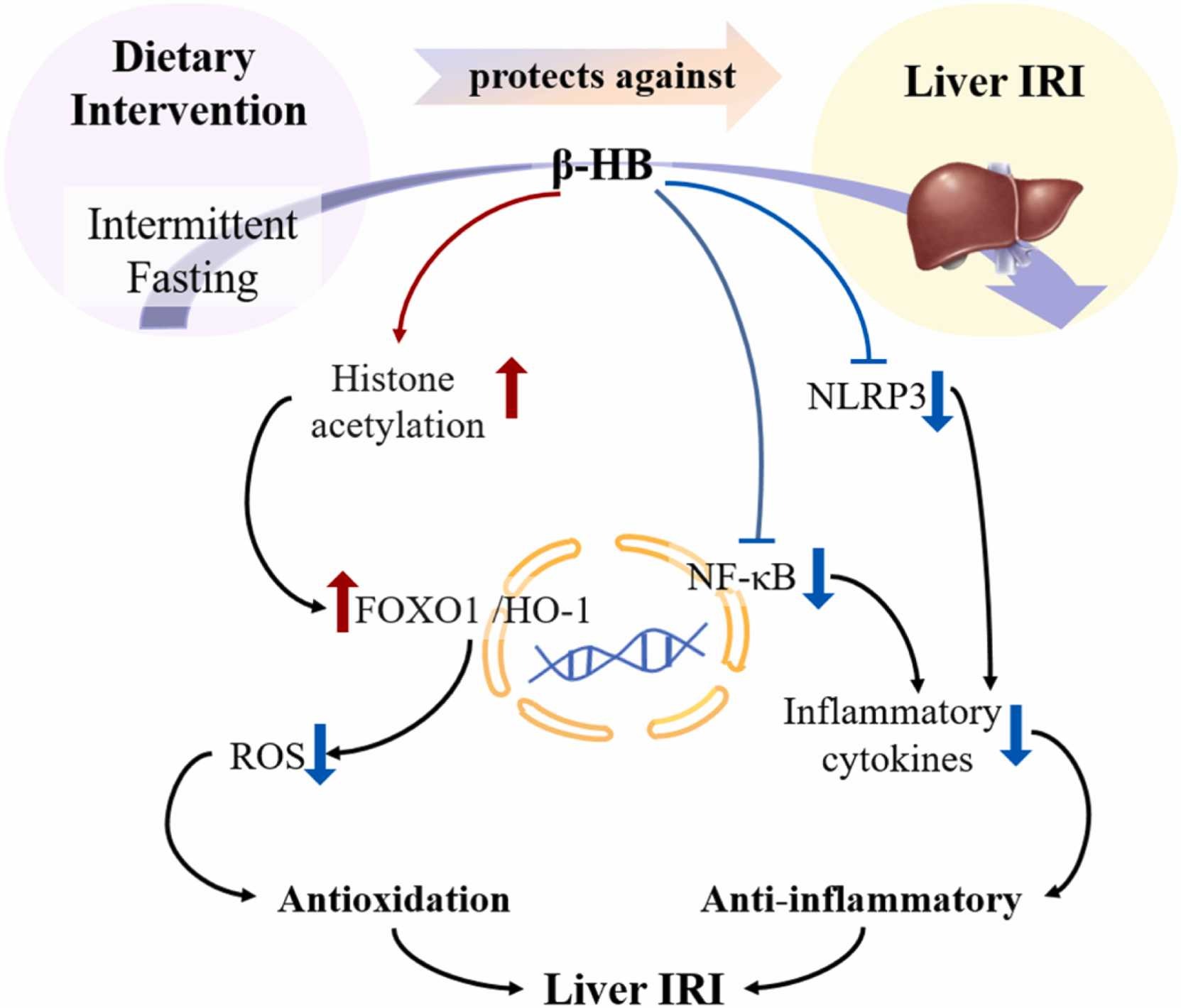
BHB also functions as an endogenous histone deacetylase (HDAC) inhibitor, activating protective genes that enhance the liver's ability to handle metabolic stress and increase production of key antioxidant enzymes like catalase and manganese superoxide dismutase.[7]
BHB also serves as an endogenous inhibitor of the NLRP3 inflammasome, a key inflammatory pathway that plays important roles in liver disease progression.[8] This anti-inflammatory effect helps protect liver tissue from the chronic inflammation that can contribute to metabolic dysfunction and fatty liver disease.
-
A Comprehensive Liver Health Strategy
Recent comprehensive research has identified BHB as "a crucial therapeutic target for diverse liver diseases", including non-alcoholic fatty liver disease, alcoholic liver disease, and hepatocellular carcinoma.[6] The mechanisms include regulation of lipid metabolism, activation of protective signaling pathways, and support for healthy mitochondrial function in hepatocytes.
When your liver processes BHB, it doesn't just create energy -- it activates protective pathways that fight inflammation and oxidative stress. This comprehensive view shows how various ketone sources impact liver health differently, with some supporting cellular function while others may actually burden it.[6]
This positions high-quality exogenous goBHB supplementation as a multidimensional approach to liver health -- providing clean energy, activating protective gene expression, reducing inflammation, and supporting optimal metabolic function. Rather than being just another compound that the liver must process, BHB emerges as an active contributor to hepatic wellness while delivering the benefits of ketone metabolism.
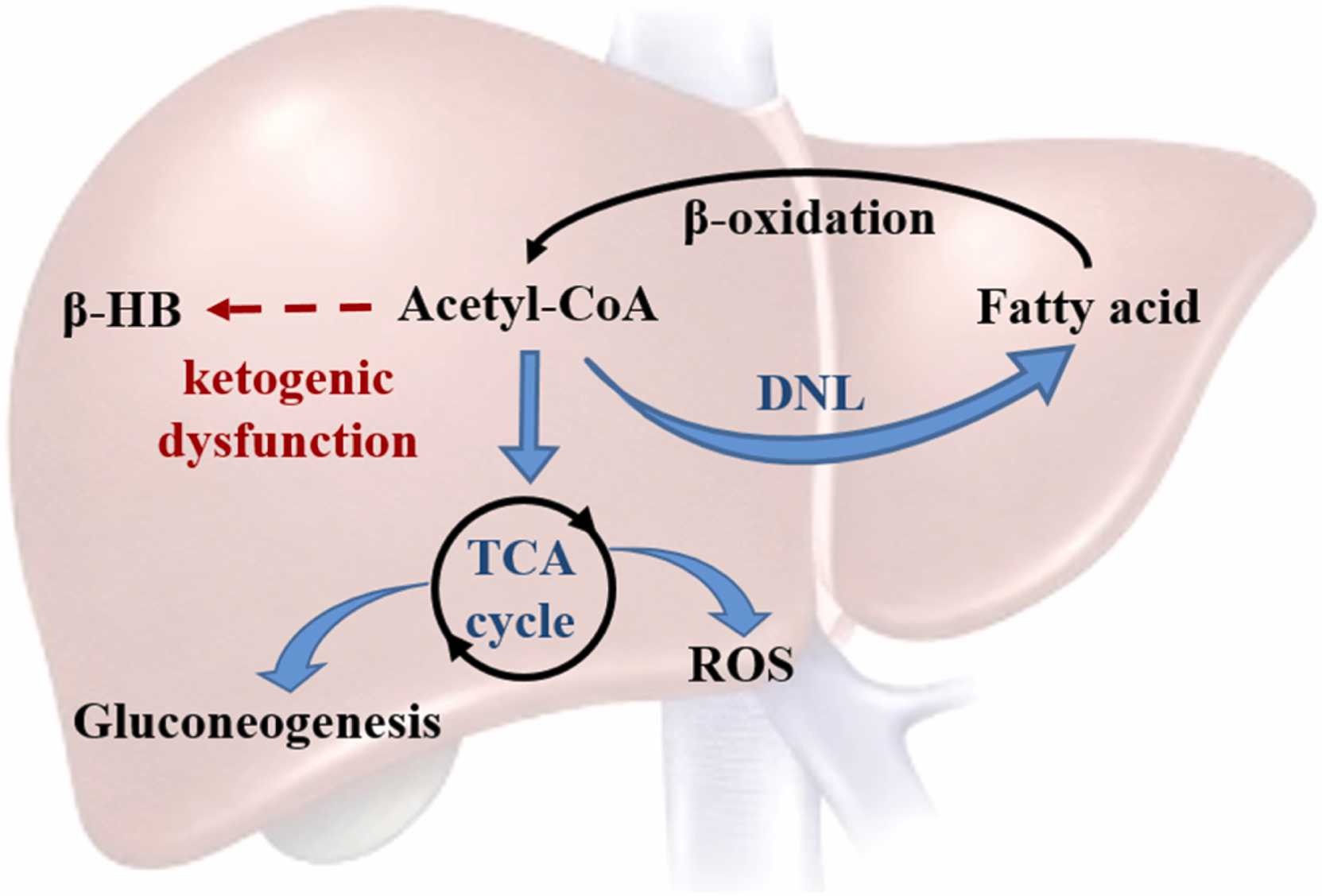
In fatty liver disease, your body's ketone-making machinery breaks down. This creates a vicious cycle where excess acetyl-CoA gets diverted into making more liver fat instead of beneficial ketones, while ramping up harmful glucose production and oxidative stress.[6]
But some may be asking, why is this better or different than going on a high-fat ketogenic diet? That's where the high-fat diet paradox comes into play:
The High-Fat Diet Paradox: When the Solution Creates a New Problem
High-fat diets have earned widespread recognition for their ability to generate beneficial ketone bodies, leading to impressive results in blood sugar levels, mental clarity, and overall metabolic health. However, a growing body of research reveals a troubling paradox: high-fat diets effectively produce endogenous ketones, but they pose significant risks to the liver in the process!
This paradox forces us to confront an uncomfortable truth about extreme dietary approaches: the benefits we seek from ketosis may come at a hidden metabolic cost that undermines long-term liver health. Understanding this trade-off is crucial for developing smarter strategies that capture ketone benefits without compromising hepatic function.
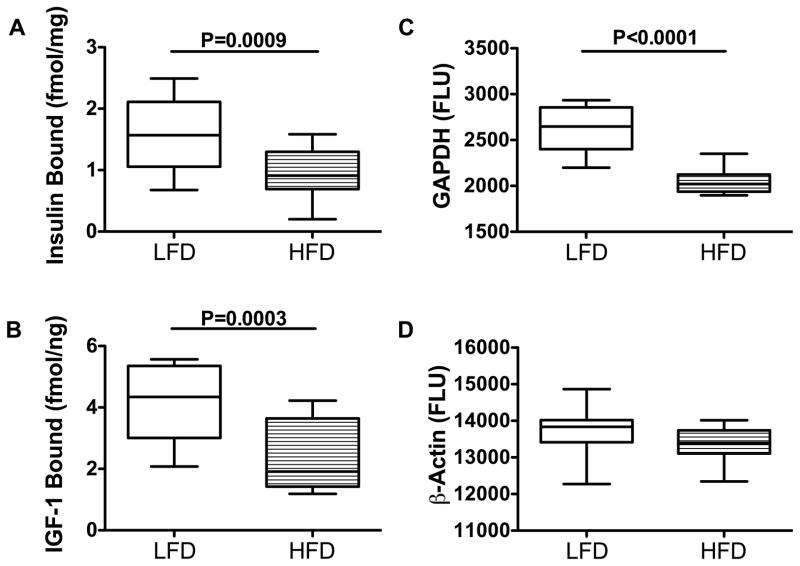
Within weeks of high-fat feeding, your liver stops responding properly to insulin. These rat studies show reduced insulin binding and impaired IGF-1 signaling -- early warning signs that metabolic dysfunction is taking hold.[9]
-
The Timeline of High-Fat Diet Damage: Liver First, Everything Else Follows
Decades of research has revealed that high-fat diets damage the liver before affecting any other organ system.[10] This sequential pattern of metabolic dysfunction provides critical insights into how dietary fat excess initiates a cascade of health problems.
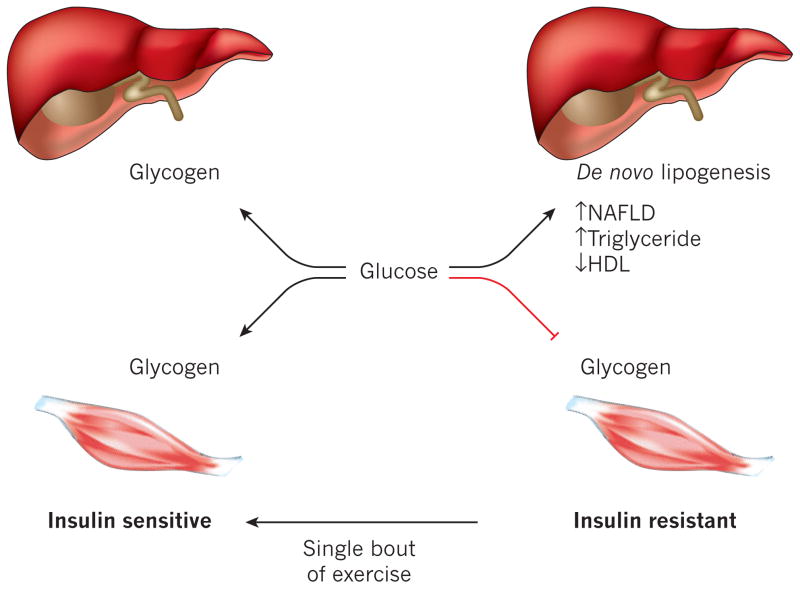
Within just three days of high-fat feeding, liver insulin resistance develops, while muscle tissue remains completely unaffected.[10] This finding demolishes the assumption that muscle and liver respond equally to dietary changes. Instead, the liver bears the initial brunt of metabolic stress from excessive fat intake.
Only after three weeks of high-fat feeding does muscle insulin resistance appear, accompanied by significant glucose intolerance and widespread metabolic dysfunction.[10] This timeline suggests that liver damage acts as the triggering event that eventually spreads metabolic dysfunction throughout the body.
When your muscles become insulin resistant, they can't store glucose as glycogen properly. This forces all that extra glucose to your liver, where it gets converted into fat through de novo lipogenesis -- but remarkably, a single bout of exercise can reverse these defects![11]
The mechanism behind this progression becomes clear when we examine what happens during those critical first three days: the liver becomes overwhelmed by the sheer volume of fat it must process, leading to impaired insulin signaling that disrupts normal glucose metabolism. This hepatic insulin resistance then creates an "oversupply of energy substrate" to other tissues, eventually causing them to develop their own insulin resistance in a protective response to metabolic overload.
-
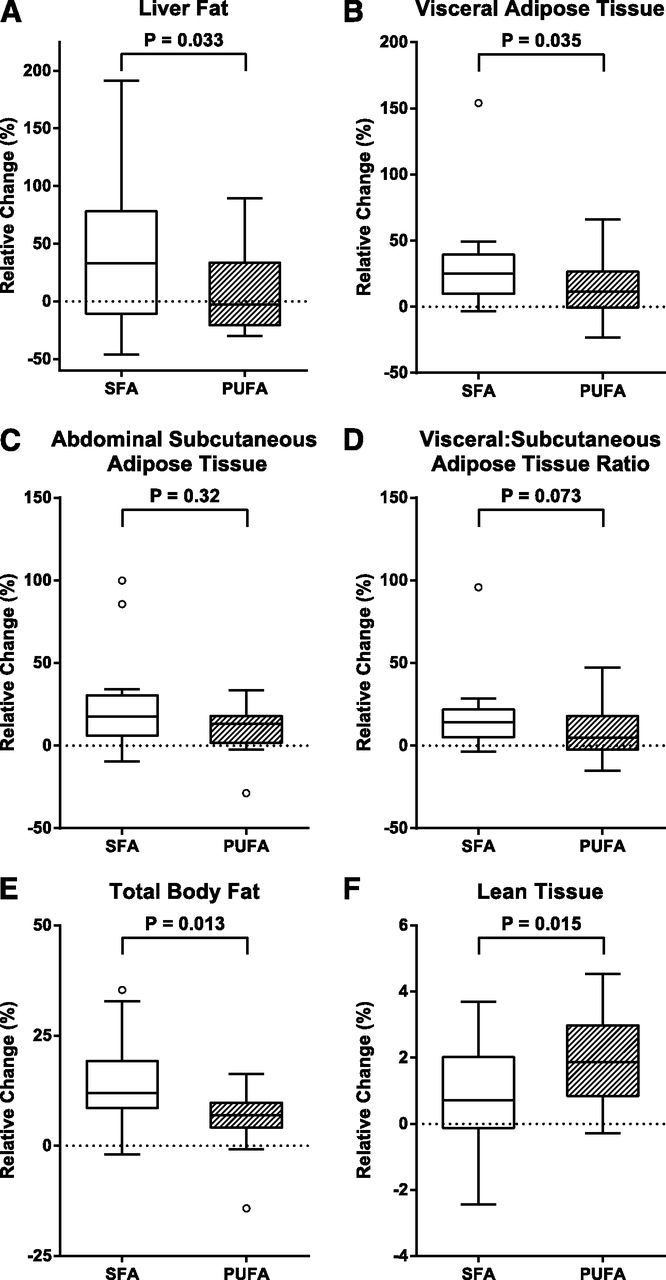
Human Evidence: Saturated Fat Dramatically Increases Liver Fat
Just seven weeks of eating saturated fat muffins significantly increased liver fat compared to polyunsaturated fats. This human study shows why fat quality matters -- your liver processes different fats very differently, with saturated fats causing more metabolic stress.[12]
While animal studies provide mechanistic insights, human research confirms that these concerns translate directly to real-world dietary patterns. The landmark LIPOGAIN study provided the first controlled evidence of how different dietary fats affect liver fat accumulation in healthy humans.
When healthy, normal-weight individuals were overfed muffins high in saturated fat (palm oil) versus polyunsaturated fat (sunflower oil) for seven weeks, the saturated fat group showed markedly increased liver fat compared to the polyunsaturated fat group.[12] Even more concerning, saturated fat caused a twofold larger increase in dangerous visceral fat compared to polyunsaturated fats.
The study revealed that liver fat accumulation directly correlated with changes in plasma saturated fatty acids and inversely correlated with polyunsaturated fatty acids.[12] This establishes a clear dose-response relationship: the more saturated fat consumed, the more fat accumulates in the liver.
Importantly, this occurred in healthy, young individuals with normal baseline liver fat content. The fact that even short-term saturated fat overfeeding produced measurable liver fat accumulation in metabolically healthy people suggests that longer-term high-fat diets could cause significant hepatic damage in real-world populations.
-
The Toxic Ceramide Connection: How High-Fat Diets Poison Liver Cells
Digging deeper, the mechanism by which high-fat diets damage liver tissue involves the production of toxic lipid metabolites called ceramides. High-fat diet feeding increases hepatic expression of pro-ceramide genes and serum ceramide levels.[9]
Chronic high-fat feeding cranks up genes that produce ceramides -- toxic lipids that poison liver cells. These harmful compounds directly impair insulin signaling and promote cell death, creating a downward spiral of liver dysfunction.[9]
Ceramides function as cellular toxins that directly impair liver function through multiple pathways:
- Ceramides activate proteins that negatively regulate insulin signaling, creating a state where liver cells become resistant to insulin's metabolic instructions.[9] This insulin resistance disrupts normal glucose and fat metabolism, leading to further lipid accumulation.
- Ceramides promote cellular apoptosis and senescence, literally killing liver cells and reducing the organ's functional capacity over time.[9] Lab studies demonstrate that ceramide exposure significantly reduces liver cell viability, mitochondrial function, and cellular ATP production.
The liver becomes trapped in a vicious negative feedback loop: high-fat intake increases ceramide production, ceramides damage liver cells and impair insulin signaling, damaged insulin signaling promotes further fat accumulation, and increased fat accumulation generates more toxic ceramides.
If there's one thing we've learned through our decades of nutritional research, it's that we must avoid negative feedback loops like this.
-
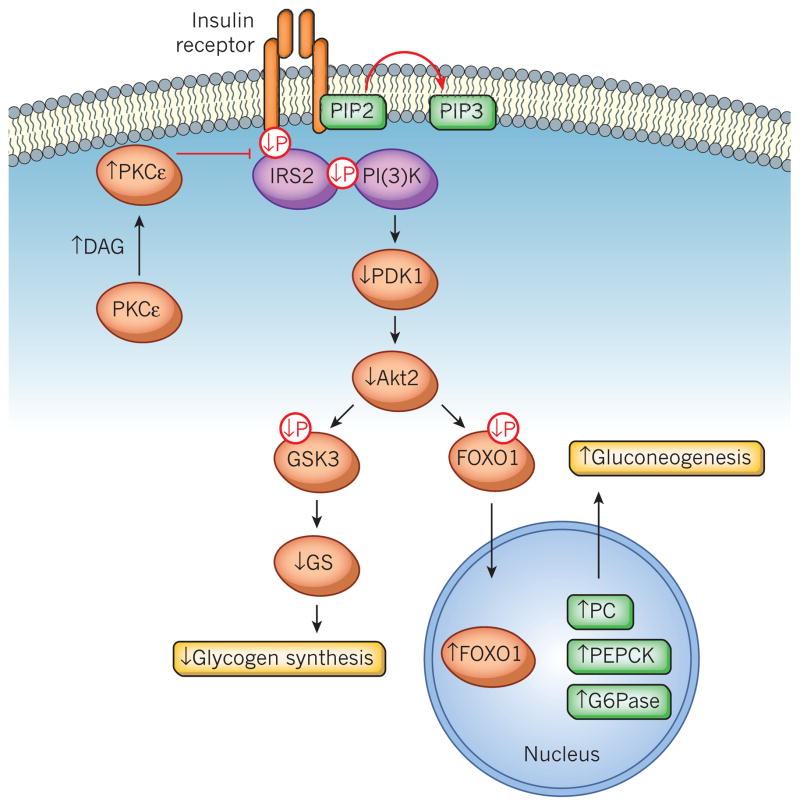
The Diacylglycerol Disaster: PKCε Activation and Metabolic Collapse
Diacylglycerol (DAG) accumulation from high-fat diets activates PKCε, which then sabotages insulin signaling at multiple points. This molecular roadblock prevents insulin from doing its job -- shutting down glucose production when you don't need it.[11]
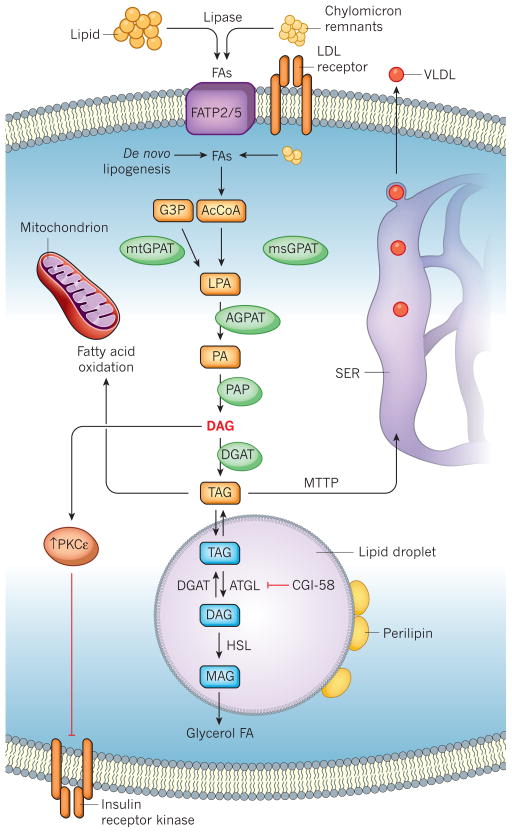
Beyond ceramides, high-fat diets trigger another dangerous pathway through diacylglycerol accumulation. Excess hepatic diacylglycerol activates protein kinase Cε (PKCε), which directly inhibits insulin receptor signaling.[11] This is one of the most well-established mechanisms linking liver fat to metabolic dysfunction.
This process activation blocks insulin's ability to suppress glucose production, leading to inappropriately high blood glucose levels even when insulin levels are elevated.[11] The liver essentially becomes "blind" to insulin's signals, continuing to pump out glucose regardless of the body's actual needs.
It turns out that hepatic diacylglycerol content is the best predictor of hepatic insulin resistance in obese humans, far outperforming inflammatory markers or other lipid species as risk indicators.[11] This establishes diacylglycerol accumulation as a primary driver of metabolic dysfunction rather than just a side effect.
-
Consider the Fat Soluble Passengers in the Fat
The above research doesn't even include another major issue: fats often come with harmful fat-soluble toxins (such as heavy metals, alcohols, and aldehydes) that are difficult to process and excrete. These often need to be stored in the liver fat until it can catch up, which may never happen. You can't just urinate out excess fat soluble molecules, after all -- so they get stowed away until later, greatly contributing to fat storage.
Point being, "calories" and "energy" aren't the only things stuffed away into liver fat.
-
Multiple Mechanisms Converge: A Perfect Storm for Liver Damage
Fatty liver happens when your liver gets more fat than it can process. Like a backed-up highway, excess fatty acids from diet and fat tissue overwhelm your liver's ability to burn or export them, leading to dangerous accumulation.[11]
High-fat diets don't damage the liver through a single pathway... they create a perfect storm of interconnected mechanisms that compound each other's effects:
- Mitochondrial dysfunction occurs as high-fat diets impair the liver's cellular powerhouses, reducing ATP production and increasing oxidative stress.[13] This energy deficit makes liver cells less capable of handling metabolic stress.
- Endoplasmic reticulum stress develops as liver cells struggle to process the massive influx of dietary fats, triggering inflammatory pathways and cellular damage.[13]
- Autophagy disruption impairs the liver's ability to clean up damaged cellular components, allowing toxic materials to accumulate and cause further harm.[13]
- Chronic inflammation emerges as damaged liver cells release inflammatory signals, creating a sustained inflammatory environment that perpetuates cellular damage and insulin resistance.[13]
These mechanisms work synergistically, too: ceramide production increases oxidative stress, oxidative stress impairs mitochondrial function, mitochondrial dysfunction reduces cellular energy, energy depletion impairs detoxification processes, and compromised detoxification allows more toxic metabolites to accumulate.
-
The Composition Problem: Not All Fats Are Equal, But Volume Matters
While dietary fat composition does influence liver health outcomes, the research reveals that total fat volume poses risks regardless of the specific fat types consumed. Even monounsaturated fats, traditionally considered "healthy", can trigger hepatic steatosis when consumed in high quantities.[13] This challenges the assumption that simply choosing "good" fats eliminates the risks of high-fat dietary patterns.
Point being, the liver has a finite capacity for fat processing, regardless of fat quality.
During liver stress or injury, BHB acts as a cellular shield by boosting antioxidant defenses and calming inflammatory responses. It achieves this through histone modifications and by blocking inflammatory triggers like NF-κB and NLRP3.[6]
So the challenge becomes clear: how do we access the metabolic, cognitive, and therapeutic benefits of ketone bodies without subjecting the liver to potentially harmful fat processing demands? Traditional approaches have forced an all-or-nothing choice between ketone benefits and liver health.
Thankfully, there's a better way.
Beyond Dietary Extremes: The Exogenous Ketone Solution
The solution to this paradox lies not in abandoning ketone metabolism entirely, but in recognizing that the therapeutic benefits of ketones can be separated from the metabolic stress of processing excessive dietary fat. Exogenous ketone supplementation offers an excellent escape from the high-fat diet dilemma.
By providing ketone bodies directly through supplementation, we can access their benefits -- including enhanced cellular energy, reduced inflammation, improved mitochondrial function, and neuroprotective effects -- while maintaining dietary flexibility and supporting rather than challenging liver function.
The goal becomes accessing the benefits of ketones through the most liver-friendly pathway possible, rather than forcing the liver to process massive amounts of dietary fat to generate them endogenously.
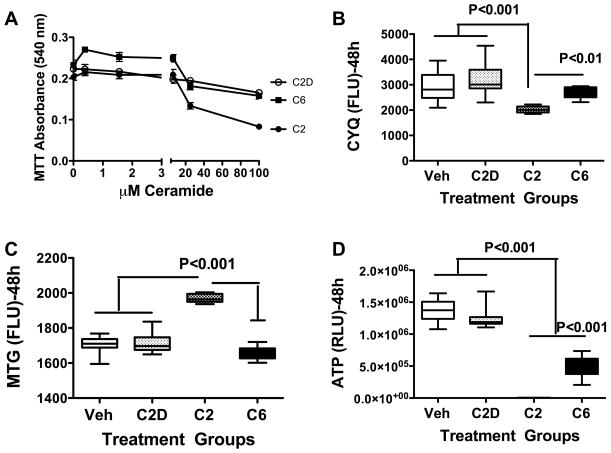
When you expose liver cells to ceramides in the lab, their mitochondria -- the cellular powerhouses -- start failing. ATP production plummets while oxidative damage markers spike, showing how these toxic lipids directly sabotage cellular energy production.[9]
Strategic exogenous ketone supplementation allows us to maintain metabolic flexibility while providing targeted support to liver cells through compounds that actually generate hepatic ATP rather than consuming it. This is a fundamental shift from viewing supplements as metabolic burdens to recognizing certain compounds as active contributors to organ health.
The research is clear: high-fat diets create real risks for liver health through multiple interconnected mechanisms. Rather than accepting these risks as the necessary price for ketone benefits, we can choose a smarter approach that supports both metabolic health and liver function simultaneously.
Let's talk about some of the potential applications and dosing strategies, and then get into one major pitfall in the ketone world that we must avoid.
Practical Applications: Implementing Liver-Healthy Ketone Supplementation
The research establishing BHB as a liver-supportive compound opens up exciting possibilities for practical implementation. However, not all ketone sources deliver equal benefits, and successful use requires understanding both the science behind different forms and how to incorporate them into a comprehensive health strategy.
Choosing the Right Ketone Source
The choice between ketone sources can make the difference between supporting and burdening liver health. Free acid BHB emerges as the clear winner for liver support, offering several key advantages over alternatives.[1]
Exogenous BHB is now for everyone—from athletes needing endurance to those boosting brain function. Offering clean, lasting energy, BHB is proving versatile and backed by research.
- Free acid BHB provides immediate bioavailability without requiring dissociation from mineral salts, leading to faster absorption and more efficient liver ATP production. Its neutral taste profile makes it ideal for beverage applications, and it avoids the mineral loading that can become problematic with higher doses of salt forms.
- BHB salts (sodium, magnesium, calcium, or potassium BHB) offer the advantage of providing essential electrolytes alongside ketones, which can be beneficial for those following low-carb diets or during exercise.
However, ketone salts are limited by gastrointestinal tolerance and can elevate blood ketones only in the range of 0.5-1.5 mM due to the high mineral load.[14] For liver health specifically, the salt forms still provide positive ATP generation, though less efficiently than free acid.
- Ketone esters should be avoided entirely for liver health applications.
Research has documented that 1,3-butanediol produces serious side effects including hepatotoxicity, metabolic acidosis, and even physical dependence.[15] Its metabolism shares similarities with ethanol processing, which may explain why some ketone ester products are marketed as alcohol alternatives and why dependency issues have been reported.
Additionally, the NNB Labs research revealed that 1,3-butanediol-based esters function as massive ATP consumers, depleting 89.1 mg/min of liver ATP![1]
This is discussed in heavy detail in our article, 1,3-Butanediol and Ketone Esters vs Free Acid BHB: Severe Impacts on Liver ATP.
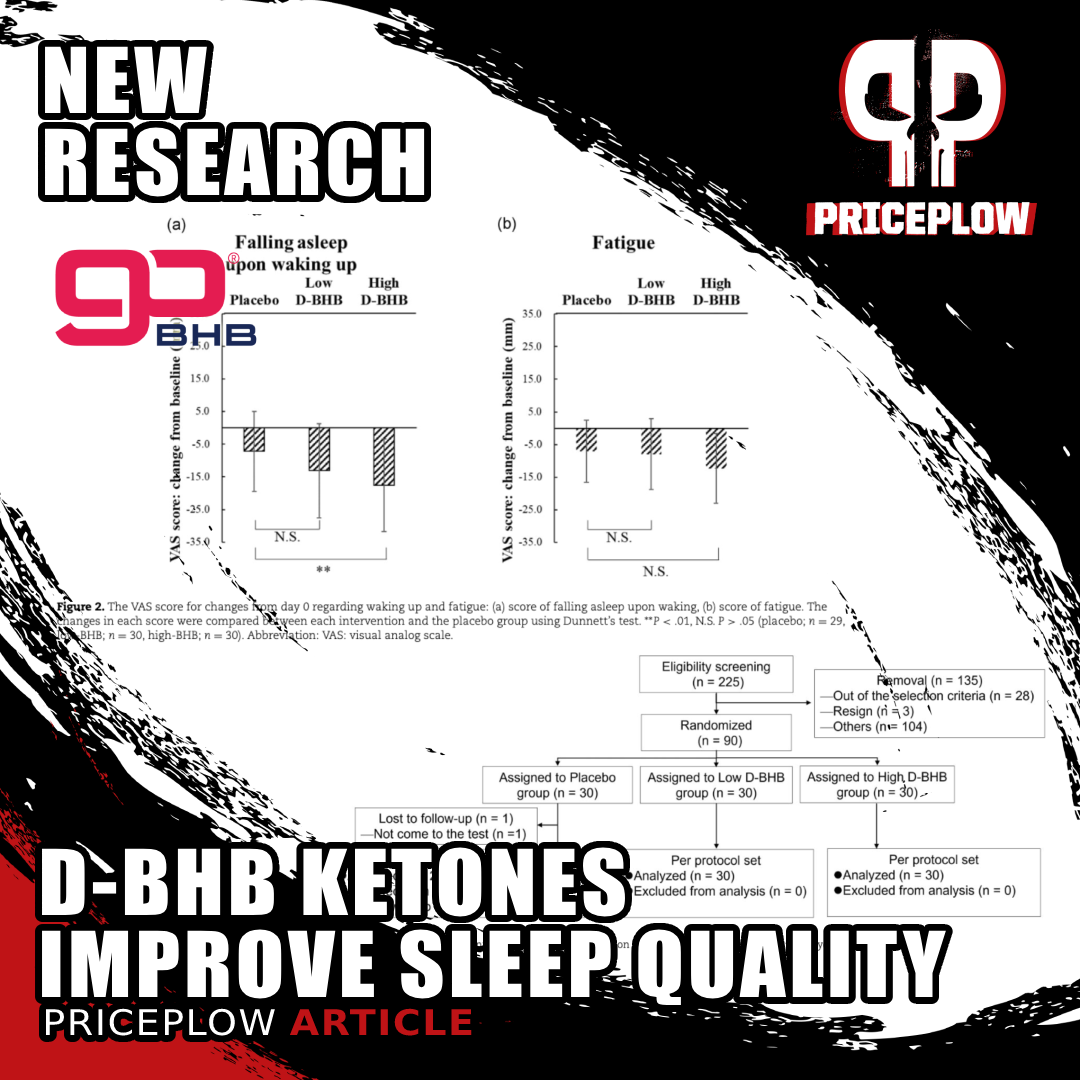
New research shows BHB ketones can significantly improve sleep quality! Study found 1.5-2.9g of D-BHB taken before bed enhanced multiple sleep parameters including easier falling asleep and feeling more refreshed upon waking.[16]
The liver ATP research demonstrates that the combination of D-BHB free acid with C8 MCT produced the highest liver ATP yield of all tested compounds, suggesting that strategic pairing can optimize hepatic energy production beyond what either compound achieves alone.[1]
The bottom line is clear: when choosing between ketone sources, the difference isn't just about effectiveness -- it's about supporting versus burdening your body's most vital organ. The data strongly favors goBHB (in its several forms) as the liver-friendly choice for anyone serious about long-term metabolic health.
Dosing and Applications
Recent clinical research has revealed that effective BHB dosing for health benefits starts much lower than one would expect. A human trial has shown significant sleep quality improvements with doses as low as 1.5g and 2.9g of D-BHB.[16]
For general liver support and metabolic benefits, effective dosing ranges from 1.5g to 5g of D-BHB per serving:
- 1.5-2.9g: Sleep quality improvement, gentle metabolic support
- 3-5g: More pronounced energy and cognitive benefits
- 5g+: Maximum metabolic effects, likely measurable ketosis
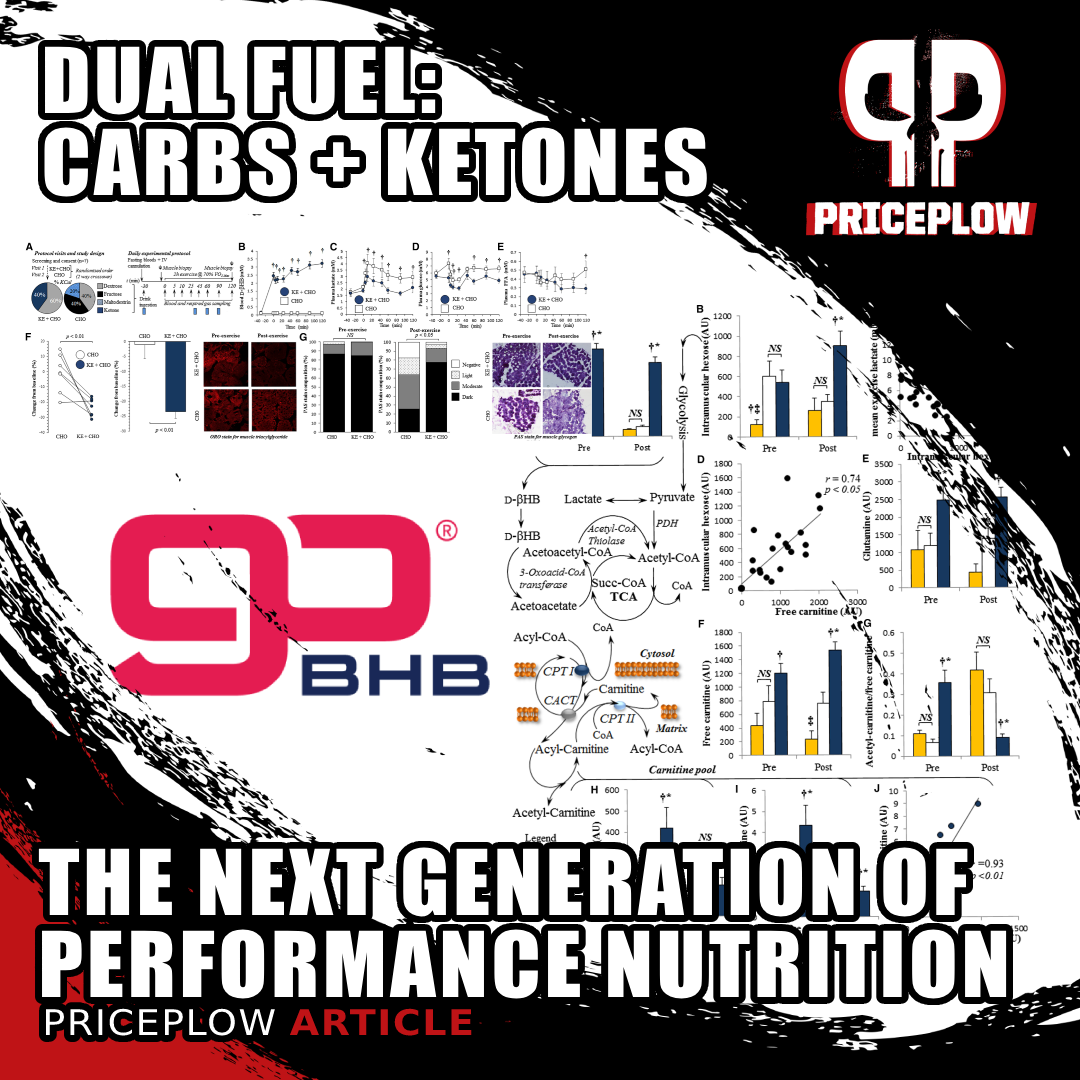
Fuel your workouts with the power of "dual fuel", combining goBHB ketones and carbs for optimal performance.
For cutting-edge applications, consider the innovative "dual fuel" pre-workout approach that combines ketones with carbohydrates for enhanced performance. This is described in our article, DUAL FUEL: Combining Ketones and Carbs for Rocket Performance.
For other applications, such as using BHB for head injury prevention and support, we would go to 10 grams per day or even higher.
The Balanced Approach: Beyond Dietary Extremes
The beauty of liver-supportive ketone supplementation lies in its compatibility with normal, healthy eating patterns. Unlike extreme ketogenic diets that require dramatic macronutrient restriction, strategic BHB supplementation allows access to ketone benefits while maintaining dietary flexibility and supporting liver function.[6]
Rather than forcing metabolic dependence on a single fuel source, you can maintain metabolic flexibility by combining moderate and appropriately-timed dietary carbohydrate intake with strategic ketone supplementation. This approach preserves your cells' ability to efficiently utilize both glucose and ketones for energy, supporting long-term metabolic health better than dietary extremes.
For comprehensive guidance on ketone supplementation, including detailed implementation strategies, timing protocols, and product selection: BHB Supplements: The Ultimate Guide to Exogenous Ketones.
Conclusion: A Supplement That Flips the Liver Question on Its Head
The groundbreaking research on BHB and liver ATP production represents more than just another supplement study - it fundamentally challenges how we think about metabolic health and liver support. While most exogenous compounds force the liver to work overtime, high-quality BHB actually delivers energy to hepatic cells, creating a paradigm shift from liver burden to liver support.[1]
This discovery resolves the fundamental paradox we explored: while high-fat diets effectively generate beneficial ketones, they simultaneously damage the liver through multiple mechanisms. goBHB supplementation offers an elegant escape from this dilemma, allowing you to access ketone benefits without subjecting your liver to the documented risks of dietary extremes.
Rather than forcing your body into ketosis through severe carbohydrate restriction that triggers hepatic insulin resistance within days, goBHB supplementation allows you to maintain dietary flexibility while supporting one of your body's most vital organs. The liver receives energy rather than expending it, inflammation decreases through NLRP3 inhibition, and cellular protection increases through enhanced antioxidant enzyme production.[6]
New research suggests ketones may provide crucial brain protection in contact sports. goBHB supplementation offers an alternative energy source when glucose metabolism is impaired after impact. Could this be the next frontier in athlete brain safety?
The implications extend far beyond ketone supplementation itself. We should evaluate all supplements and dietary interventions through the lens of cellular energy economics - asking not just what benefits they provide, but whether they support or tax the organs responsible for processing them. BHB emerges as a rare compound that delivers its benefits while simultaneously strengthening the metabolic foundation that supports long-term health.
For those seeking to optimize metabolic health while supporting liver function, the evidence points toward a balanced approach: maintain a nutritious, reasonable diet while strategically incorporating liver-friendly exogenous ketones. This is smart supplementation at its finest: delivering targeted benefits while actively supporting the body's most important metabolic processing center.




Comments and Discussion (Powered by the PricePlow Forum)