New research suggests ketones may provide crucial brain protection in contact sports. goBHB supplementation offers an alternative energy source when glucose metabolism is impaired after impact. Could this be the next frontier in athlete brain safety?
Every season, athletes across contact sports face an inherent risk that comes with competition - traumatic brain injury (TBI). The scale of this challenge is staggering - according to the CDC, TBI accounts for approximately 2.87 million emergency department visits annually, with the numbers increasing by 54% in recent years.[1] And these figures likely underestimate the true scope, as they don't capture the many athletes who receive care outside of emergency rooms or through team medical staff.
From youth soccer fields to professional football stadiums, the potential for concussions and subconcussive impacts looms over athletes of both genders as well as their parents, coaches, and medical staff. The impact extends far beyond the acute injury - it's estimated that 5.3 million individuals in the United States live with TBI-related disabilities.[1] While protective equipment continues to evolve, the reality is that we need better solutions for protecting our athletes' brains, both before and after injury occurs.
A Safe Energy Alternative For The Brain Exists: goBHB®
What if there was a way to better prepare the brain for these inevitable impacts? What if we could provide backup fuel for neurons during their moment of crisis? The emerging science of ketone body metabolism may hold the key to a revolutionary advance in brain protection for contact sport athletes.
For decades, we've known that the brain can run on two primary fuel sources - glucose and ketones. Most athletes are glucose-dependent, but glucose metabolism can become impaired during trauma. However, ketones provide an alternative energy pathway that could help maintain brain function when it matters most. Recent research has revealed that supplementing with exogenous ketones may help support the brain's energy needs during both acute injury and recovery.
The Case for Ketones in Contact Sports
In this article, we'll explore the growing case for ketone supplementation in contact sports, examining the science behind how these molecules could be a game-changer for protecting athletes' brains. We'll break down the research showing why glucose metabolism falters after head impacts, how ketones can provide crucial backup energy, and why every athletic trainer should consider having ketone supplements in their medical kit.
We even go further to recommend supplemental ketones before and during all sporting events, but especially those at risk for TBI. This isn't just about football, either -- both men's and women's lacrosse, soccer, wrestling, and combat sports should be considered as well.
The stakes couldn't be higher - we're talking about protecting our athletes' most vital organ. Let's dive into the science and see why ketones may represent the next frontier in brain protection for contact sports.
Before heading in, sign up for our Ketone Labs news alerts below so that you don't miss out on new research -- Ketone Labs sells goBHB® ketones, available in both BHB (beta-hydroxybutyrate) salts and BHB free acid, which we'll detail further on down:
Subscribe to PricePlow's Newsletter and Alerts on These Topics
Understanding Brain Energy Crisis in TBI
When the brain experiences trauma, it sets off an immediate cascade of events that creates a severe metabolic crisis. This energy emergency in injured brain tissue occurs in two distinct phases:[2]
- an initial surge in energy demand followed by
- a prolonged depression in energy metabolism.
The Initial Energy Crisis
The moment of impact triggers a massive release of neurotransmitters, particularly glutamate, along with a flood of potassium out of neurons and calcium rushing in.[3] This ionic disruption forces neurons to work overtime, frantically pumping ions to restore their delicate balance. To meet this sudden energy demand, neurons must work overtime as their sodium-potassium pumps try to restore ionic balance, leading to a sharp increase in energy demands.[4]
To meet this sudden energy demand, the injured brain immediately increases its glucose metabolism in what's known as "hyperglycolysis".[5] However, this elevated glucose consumption can persist for days in TBI patients, depleting precious energy reserves.[5,6]
The Glucose Problem
Here's where the situation becomes particularly problematic: Just when the brain most desperately needs efficient energy production, its ability to properly metabolize glucose becomes impaired. The trauma initiates a complex series of events that essentially "breaks" normal glucose metabolism:
- The injury triggers excessive production of reactive oxygen and nitrogen species, leading to oxidative stress.[7]
- This oxidative damage activates an enzyme called PARP (poly-ADP ribose polymerase) which depletes critical NAD+ stores in cells.[8]
- The loss of NAD+ cripples the cells' ability to process glucose through glycolysis, as a key enzyme in this pathway (GAPDH) requires NAD+ to function.[9]
- Additionally, trauma appears to inhibit the pyruvate dehydrogenase complex, further blocking glucose's entry into the energy-producing TCA cycle.[10]
The end result is a devastating energy deficit - at the exact moment cells need more energy to repair and survive, their primary fuel source (glucose) cannot be efficiently utilized! This metabolic crisis contributes significantly to cellular dysfunction and death after TBI.[11]
What do you do when glucose metabolism is impaired?
This rather dire scenario sets up our next critical question - if glucose metabolism is compromised, could an alternative fuel source help rescue these struggling brain cells?
The answer lies in ketones, which can bypass many of the metabolic roadblocks that TBI creates for glucose metabolism.
Ketones: The Brain’s Emergency Backup Generator
Following from our understanding of how glucose metabolism fails after TBI, the brain requires an alternative energy source to maintain cellular function and survival. Much like a hospital relies on backup generators during a power outage, the brain has evolved to use ketones as an alternative energy source during metabolic emergencies.
Many of us understand ketones in the context of fasting and ketogenic diets. But well beyond weight loss and improved blood sugar control, research has now clearly demonstrated enhanced cognition with these keto diets,[12,13] hinting to us that there are neurological benefits to having ketones around.
goBHB® Exogenous Ketones: Take 30 minutes before activity and utilize them throughout
Thankfully, we now have access to exogenous ketone supplements that can provide these neuroprotective benefits without requiring dramatic dietary changes. Rather than waiting days or weeks to achieve ketosis through diet, athletes can supplement with goBHB® and achieve elevated ketone levels within 30 minutes.[14]
goBHB: Using the predominant ketone (BHB) in its optimal form
Of the ketone bodies produced by the body, beta-hydroxybutyrate (BHB) is the most abundant and physiologically relevant.[15] This is why goBHB, which provides supplemental BHB in its optimal form, is such an important innovation. When we discuss "ketones" in the context of metabolism and neuroprotection, we're primarily referring to BHB, as it's the predominant ketone body utilized by the brain for energy.[16]
Think of it as having an emergency fuel reserve ready to deploy at a moment's notice. Just as hospitals maintain backup generators for power outages, athletes can now have ketones readily available to support their brains if glucose metabolism becomes impaired after impact. This represents a potential paradigm shift in how we approach brain protection in contact sports - providing an alternative energy source that's immediately available when it's needed most.
They can also be taken immediately after impact
Supplements with goBHB® ketones can be taken immediately after an impact, but preferably 30 minutes before practices and competitions (as well as during and at halftime), making them available at all times.
This availability enables an alternative energy source that covers for the lost glucose processing described above, and is explained in detail next:
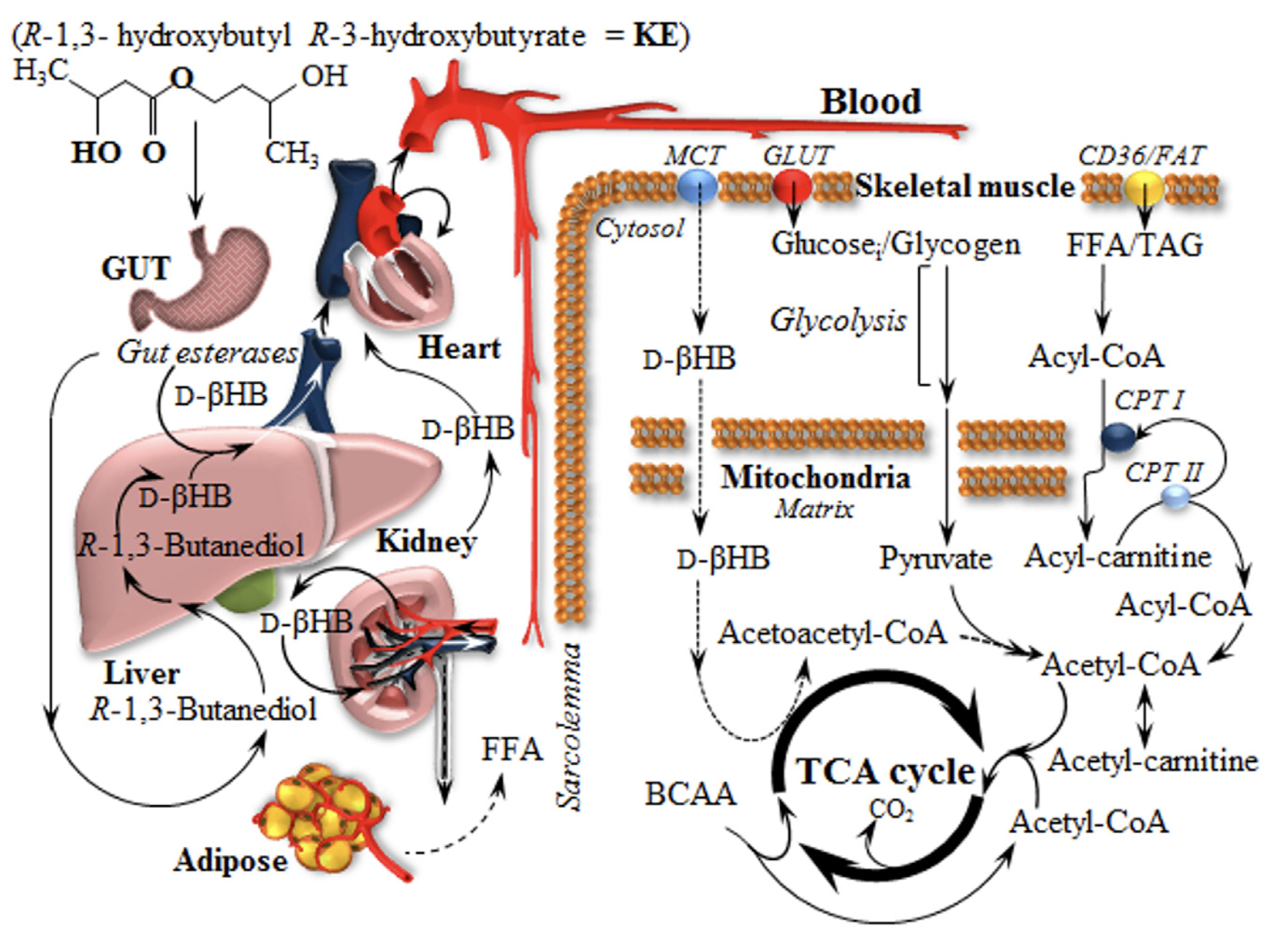
Ketones as a Solution: How and Why BHB Works Better
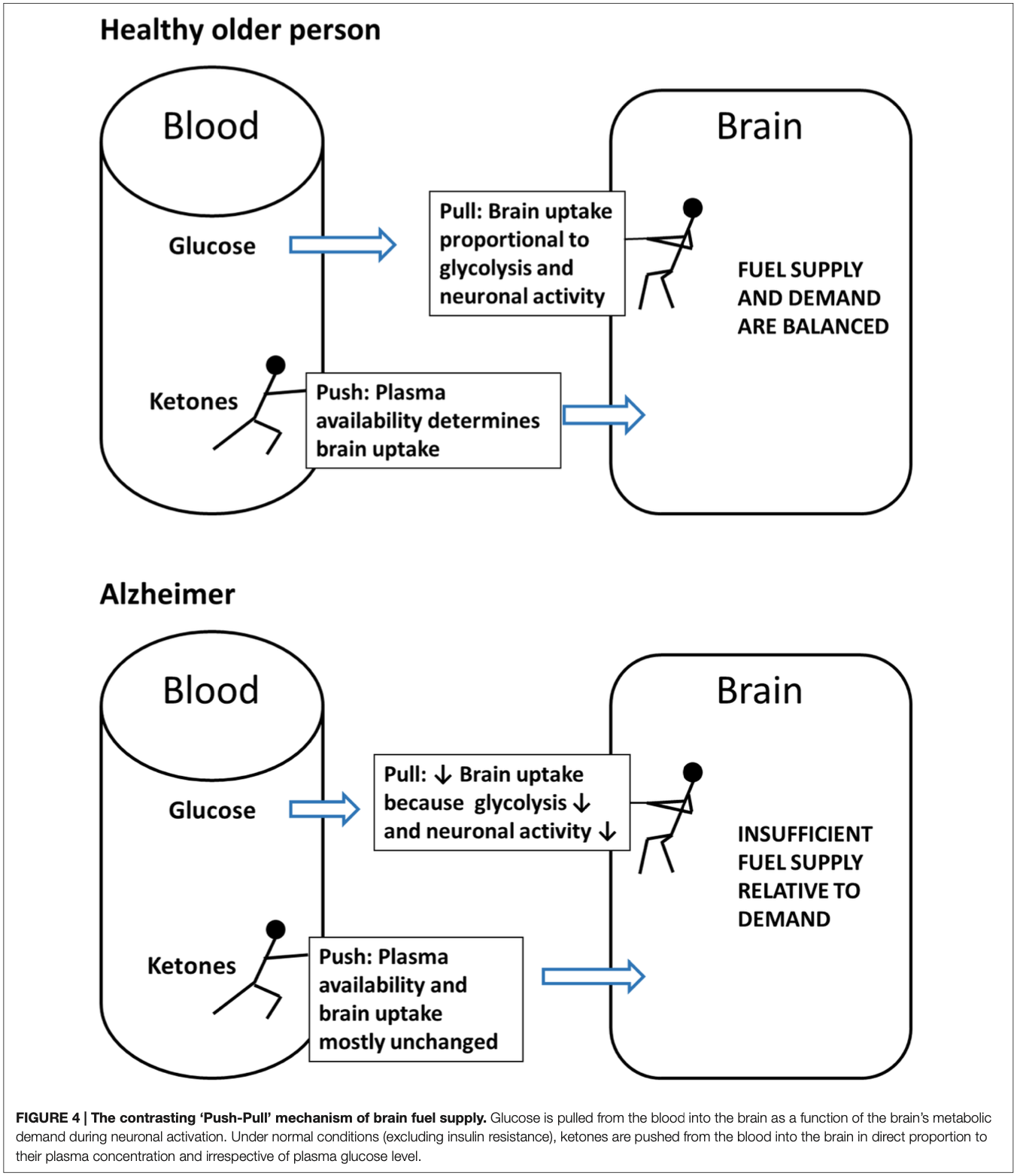
The 'Push-Pull' diagram illustrates how the brain sources its energy. Glucose is 'pulled' into the brain based on its metabolic demand, while ketones are 'pushed' into the brain proportionally to their plasma concentration, regardless of glucose availability. This mechanism emphasizes the reliability of ketones as a brain fuel during energy crises, such as those caused by traumatic injuries or metabolic deficits.[17]
The beauty in this scenario is that ketones can bypass several of the metabolic roadblocks created by a TBI event. While glucose requires 10 enzymatic steps to enter the energy-producing TCA cycle, beta-hydroxybutyrate (BHB) can be converted to energy in just 3 steps.[18] This metabolic efficiency becomes critically important when normal glucose processing is impaired.
Improved oxygen utilization
Ketones also demonstrate remarkable efficiency in oxygen utilization. During TBI, oxygen delivery to brain tissue can become compromised due to reduced cerebral blood flow and mitochondrial dysfunction.[18] In this oxygen-limited environment, ketones create a distinct advantage - ketones generate much more energy (ATP) per molecule of oxygen consumed compared to glucose.[19] This improved oxygen efficiency means that even in conditions of reduced oxygen availability, ketones can help maintain better energy production in injured brain tissue.
Even more significantly, ketones don't require the pyruvate dehydrogenase complex to enter the cellular energy production pathway. This is relevant because TBI appears to inhibit this complex through various mechanisms, including oxidative damage.[10] However, BHB doesn't require this complex at all - it has its own direct route into the cellular energy production pathway. By circumventing this damaged machinery, ketones can provide a crucial alternative pathway for energy production when glucose metabolism is compromised.
More ATP, less oxidative stress, and greater utilization after injury
Studies examining the fate of ketones in injured brain tissue have revealed another fascinating advantage: ketone metabolism actually increases the potential for ATP production by widening the substrate ratio between key components of the cellular energy production system.[20] This means that ketones can potentially produce more energy per unit than glucose[21] - a critical benefit when every bit of energy counts for cellular survival.
This graph demonstrates the effects of β-Hydroxybutyrate (βHB) supplementation on brain ATP levels following a controlled cortical impact, a model for traumatic brain injury (TBI). The data reveal an 8.5-fold increase in βHB uptake and over a 10-fold rise in cerebral ATP production within 3 hours post-injury, underscoring βHB's potential to restore cellular energy and support brain recovery.[22]
Furthermore, ketones appear to do more than just provide energy -- they are neuroprotective. When brain tissue is injured, it experiences a surge in damaging free radicals in the form or Reactive Oxygen Species (ROS). BHB not only provides clean-burning energy but also helps reduce this oxidative damage,[23] which contributes to glucose metabolic dysfunction in the first place.[18] This creates a potentially virtuous cycle where ketones not only provide immediate energy support but may help protect and restore normal metabolic function over time. It's like having both a backup generator and a surge protector for your brain cells.
Perhaps most compelling is that the brain's ability to take up and utilize ketones actually increases after injury, particularly when glucose metabolism is impaired.[22] This suggests that the injured brain may be naturally attempting to shift toward ketone metabolism as an alternative energy source - if only we make them available at the right time.
This understanding of ketones as a metabolic "bypass" for damaged glucose metabolism pathways has profound implications for how we approach brain protection in contact and combat sports. This is crucial since most athletes rely primarily on glucose metabolism and lack sufficient naturally-occurring ketones to aid in post-impact recovery. If we could ensure athletes have elevated ketone levels before and during competition, we might be able to provide their brains with an immediately available alternative fuel source in the critical moments after impact.
Exogenous Ketones with goBHB®: No waiting for ketone generation
This is where exogenous ketone supplementation with goBHB® becomes extremely valuable. Rather than waiting for the body to produce ketones naturally - which can take days of strict dieting - supplemental BHB can provide immediate support when the brain needs it most. Think of it as having an emergency fuel reserve ready to deploy at a moment's notice - and it can be in every athlete's sports drink and every team doctor's kit.
Beyond Energy: BHB’s Broader Neuroprotective Effects
While providing crucial energy is important, BHB's protective effects on the brain extend far beyond just being an alternative fuel source. Several other key mechanisms make BHB valuable for protecting athletes' brains during contact sports.
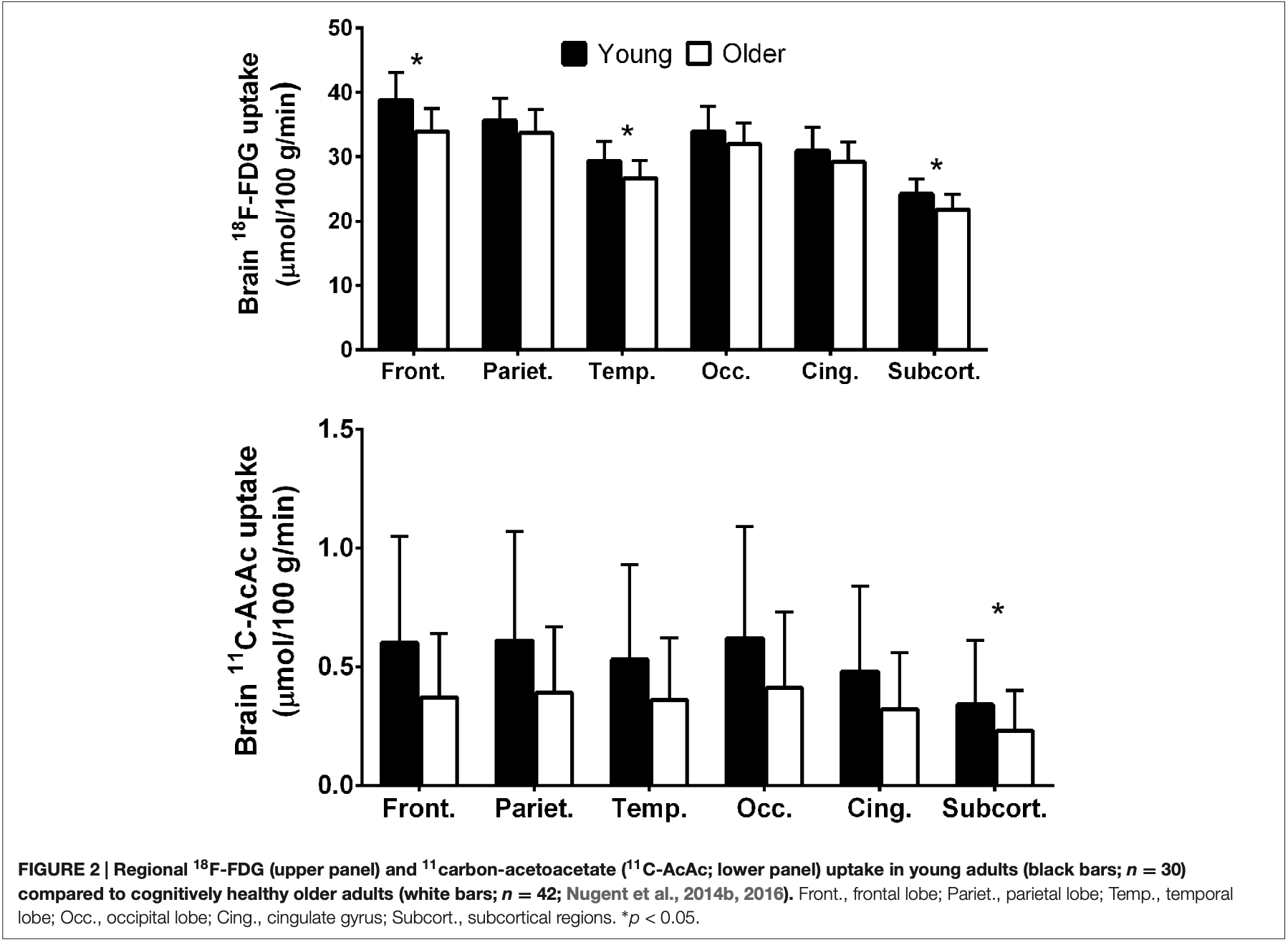
This chart compares glucose and ketone uptake in various brain regions across young and older adults. The findings show a marked decline in glucose uptake in older adults, particularly in the frontal and parietal regions, while ketone uptake remains consistent. This stability in ketone metabolism highlights their critical role as an alternative energy source for the aging brain.[17]
-
Reduce the inflammatory cascade
One of BHB's most powerful effects is its ability to reduce the inflammatory cascade that occurs after head impacts. When the brain experiences trauma, it triggers an inflammatory response that, while initially protective, can spiral out of control and cause additional damage. BHB helps regulate this response by inhibiting a key inflammatory complex called NLRP3.[24] This helps maintain a balanced inflammatory response rather than an excessive one that could cause further harm.
-
Increased BDNF Levels
BHB also acts as a powerful signaling molecule, helping to activate the brain's own protective pathways. Research shows that ketones can stimulate the production of brain-derived neurotrophic factor (BDNF), a protein that supports the survival of existing neurons and encourages the growth of new ones.[24] This becomes particularly important when brain cells are under stress from impact forces.
-
Support the brain’s structural integrity
Perhaps most importantly for contact sport athletes, BHB appears to help maintain the brain's structural integrity. Studies have shown that ketone supplementation can help preserve the blood-brain barrier - the crucial gateway that controls what enters and exits brain tissue.[26] When this barrier is compromised by impact, it can lead to increased swelling and inflammation, but BHB helps maintain its integrity.
For athletes in contact sports, having BHB available before and after competition could provide a crucial layer of protection. Think of it as putting your brain in a protective metabolic state that's better prepared to handle impacts. The combination of enhanced energy availability, reduced inflammation, and strengthened cellular protection makes goBHB® a very powerful tool for brain health in contact sports.
-
Supporting Evidence from Ketogenic Research
The neuroprotective potential of ketones is also supported by extensive research into the ketogenic diet across various neurological conditions. We're not endorsing a keto diet for contact sports athletes, but the effects are worth understanding.
For instance, studies have shown that elevated ketone levels can improve outcomes in mild cognitive impairment, seizure disorders, and more severe neurodegenerative conditions.[12,13]
Gary Millet of Ketone Labs / goBHB joins the PricePlow Podcast for Episode #138 to talk about the future of BHB research and exciting new applications to come.
What's interesting for contact sport applications is how ketones appear to be neuroprotective even in acute settings. Studies of the ketogenic diet in animal models of traumatic brain injury have shown reduced contusion volume and improved cognitive outcomes.[27] While these studies used dietary interventions rather than supplementation, they provide additional mechanistic support for ketones' ability to protect neural tissue.
Even in cases of more severe brain trauma, ketogenic interventions have shown promise in reducing secondary injury and improving recovery outcomes.[25] This suggests that having elevated ketone levels - whether through diet or supplementation - may provide neurological benefits across a spectrum of brain injuries, from mild impacts to more serious trauma.
While more research is always needed, these findings from ketogenic diet research help validate the potential of exogenous ketone supplementation for athletes in contact sports. By providing the same neuroprotective molecules in a more practical and immediate form, BHB supplements may offer similar benefits without requiring dramatic dietary changes.
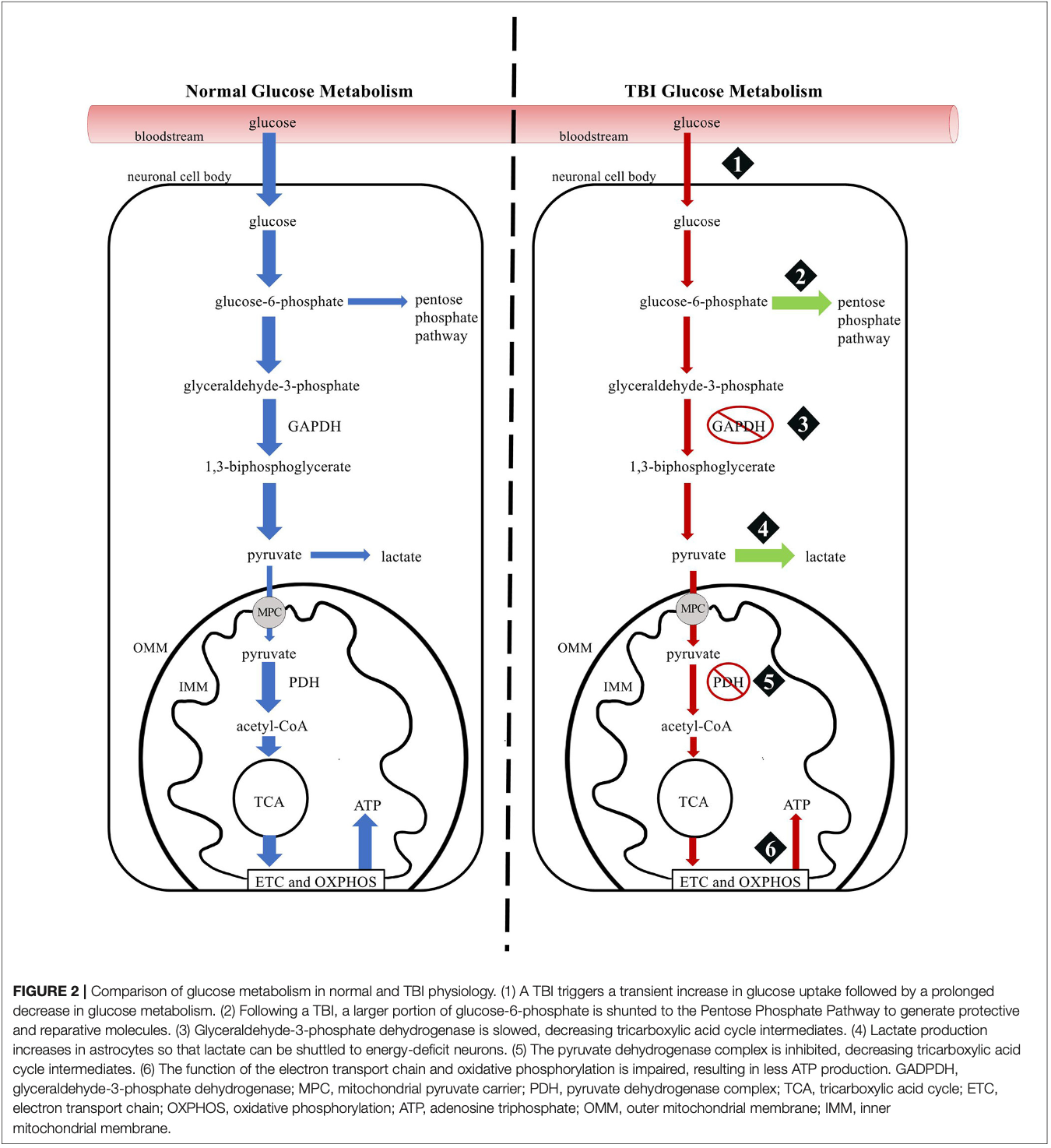
This comparison highlights how ketones bypass impaired glucose metabolism in traumatic brain injuries. While glucose metabolism becomes inefficient due to cellular damage, ketones act as an alternative energy source, fueling brain recovery by enhancing ATP production and reducing oxidative stress. This unique metabolic shift demonstrates the therapeutic potential of ketone supplementation for brain injuries.[25]
Additional Physical Athletic Benefits
Beyond brain protection, BHB supplementation offers several compelling performance benefits for athletes. Research shows that ketones can serve as an alternative fuel source during exercise, potentially improving endurance and recovery.[28] This is valuable for athletes looking to maximize both their cognitive and physical performance.
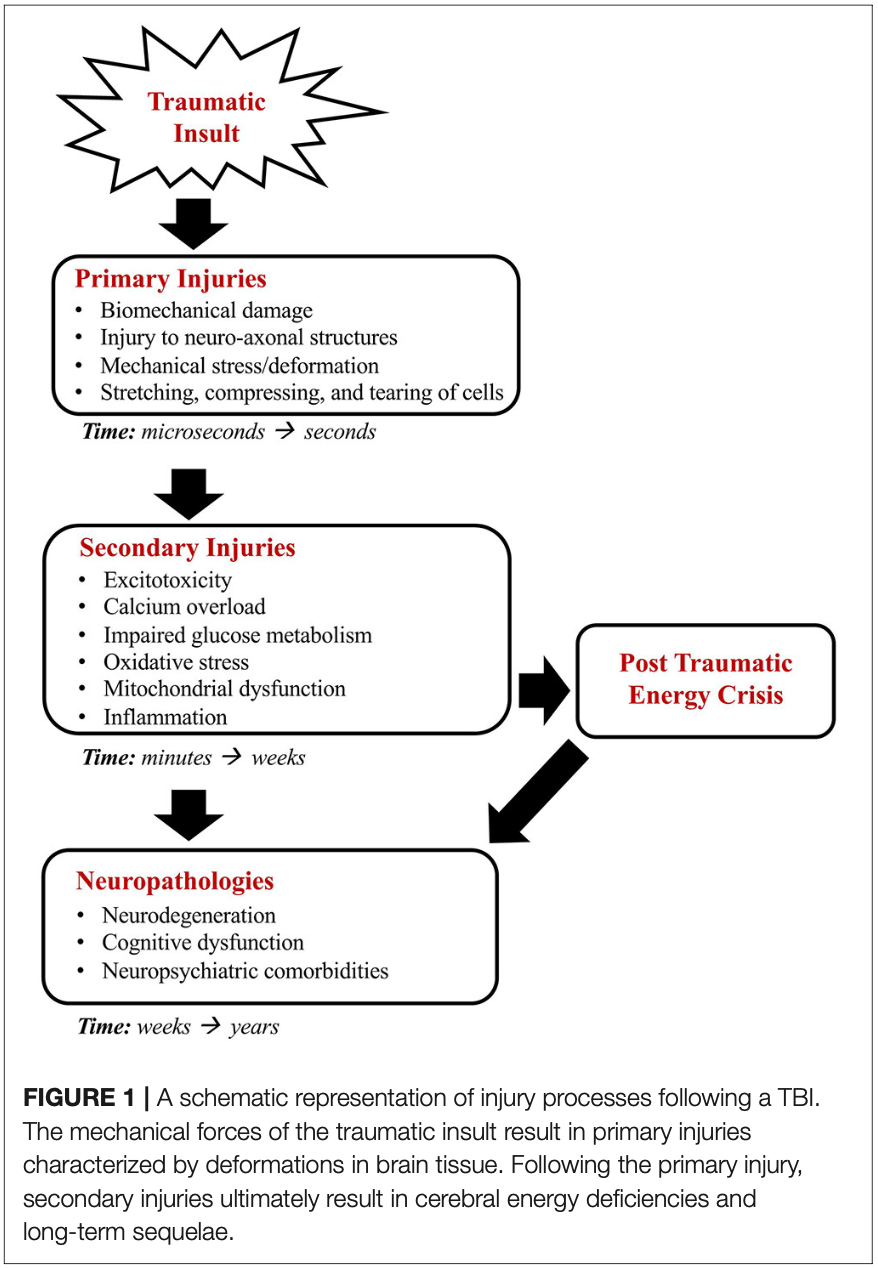
A detailed breakdown of primary and secondary injury mechanisms following traumatic brain injury. The chart highlights the immediate mechanical damage (primary injury) and the delayed cascade of metabolic dysfunction, oxidative stress, inflammation, and neuronal damage (secondary injury). This timeline underscores the importance of interventions, like ketone supplementation, to address energy deficits and reduce long-term damage.[25]
-
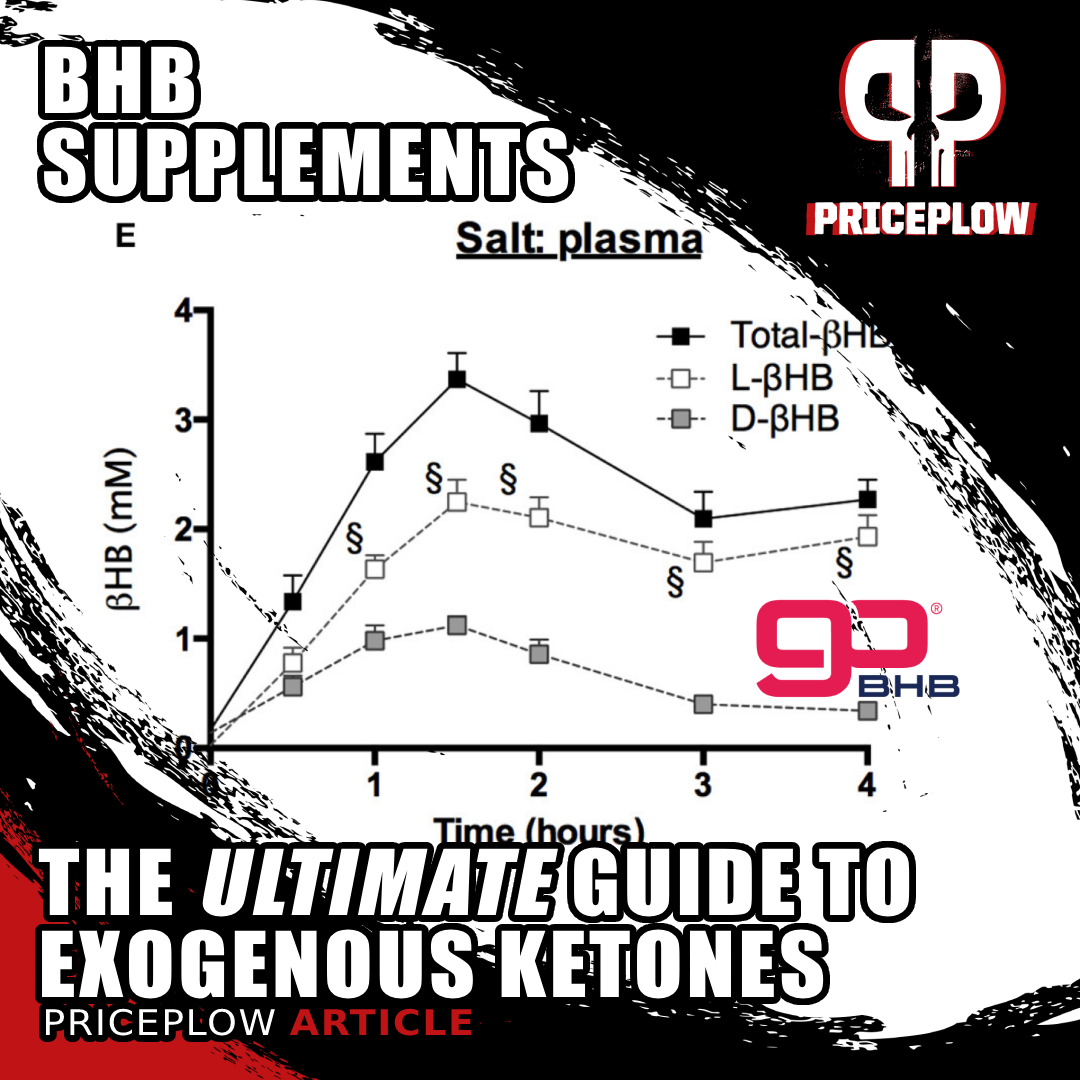
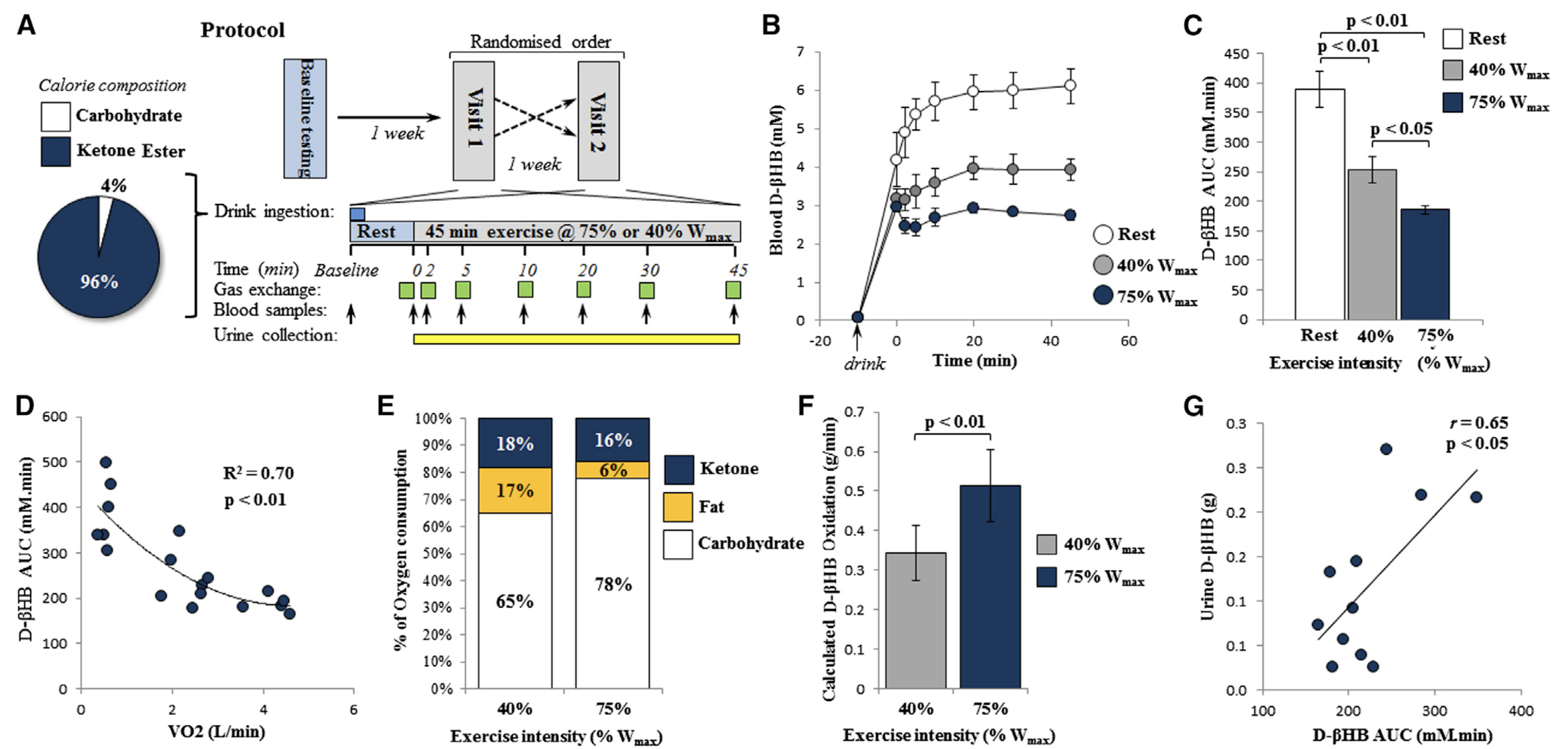
Glycogen sparing
One of the most significant athletic advantages of ketone supplementation is its ability to preserve precious glycogen stores. When athletes consume BHB along with carbohydrates, their bodies can utilize ketones for lower-intensity efforts, effectively "saving" glucose for when it's needed most - during high-intensity bursts of activity.[28] This metabolic flexibility allows athletes to maintain higher performance levels throughout competition, as their primary fuel sources are strategically preserved.
-
Reduced Exercise-Induced Fatigue
Ketone supplementation can also significantly reduce lactate production during exercise.[28] This reduction in lactate accumulation can help delay the onset of fatigue, allowing athletes to maintain higher performance levels for longer periods. Competitors supplementing with ketones often report improved endurance and reduced perception of effort during training and competition.
-
Enhanced Recovery Through Inflammation and Oxidative Stress Reduction
The reduction in inflammation and oxidative stress reported above isn't only for the brain.
BHB can decrease the production of inflammatory markers and free radicals that typically surge after intense physical activity.[23,29] This anti-inflammatory effect may help athletes recover more quickly between training sessions or competitions, potentially reducing muscle soreness and improving overall adaptation to training.
These graphs demonstrate how exercise intensity influences blood ketone levels and metabolism. Higher intensity exercise reduces circulating ketones faster, emphasizing their role as an oxidative fuel source during physical exertion. The data highlights ketones' unique ability to support endurance by sparing glycogen and reducing plasma lactate levels, which is beneficial for athletes and individuals recovering from energy deficits.[28]
We cover the above studies in greater detail in our article, "DUAL FUEL: Combining Ketones and Carbs for Rocket Performance". They're not fully in the scope of this article, so let's keep moving, but they're benefits athletes should be aware of.
The Evidence
While protecting athletes' brains during competition has long been the domain of equipment manufacturers and rule changes, emerging research suggests we may have overlooked a powerful metabolic approach to neuroprotection. A growing body of evidence - from animal studies to early human research - indicates that ketone supplementation could provide crucial support for the brain during and after impact events.
Of course, realize that obtaining human research will always be a major challenge - researchers cannot ethically conduct double-blinded, placebo-controlled research to injure and monitor human subjects. But with a combination of animal research and observational study, we can learn quite a bit.
Preclinical Research
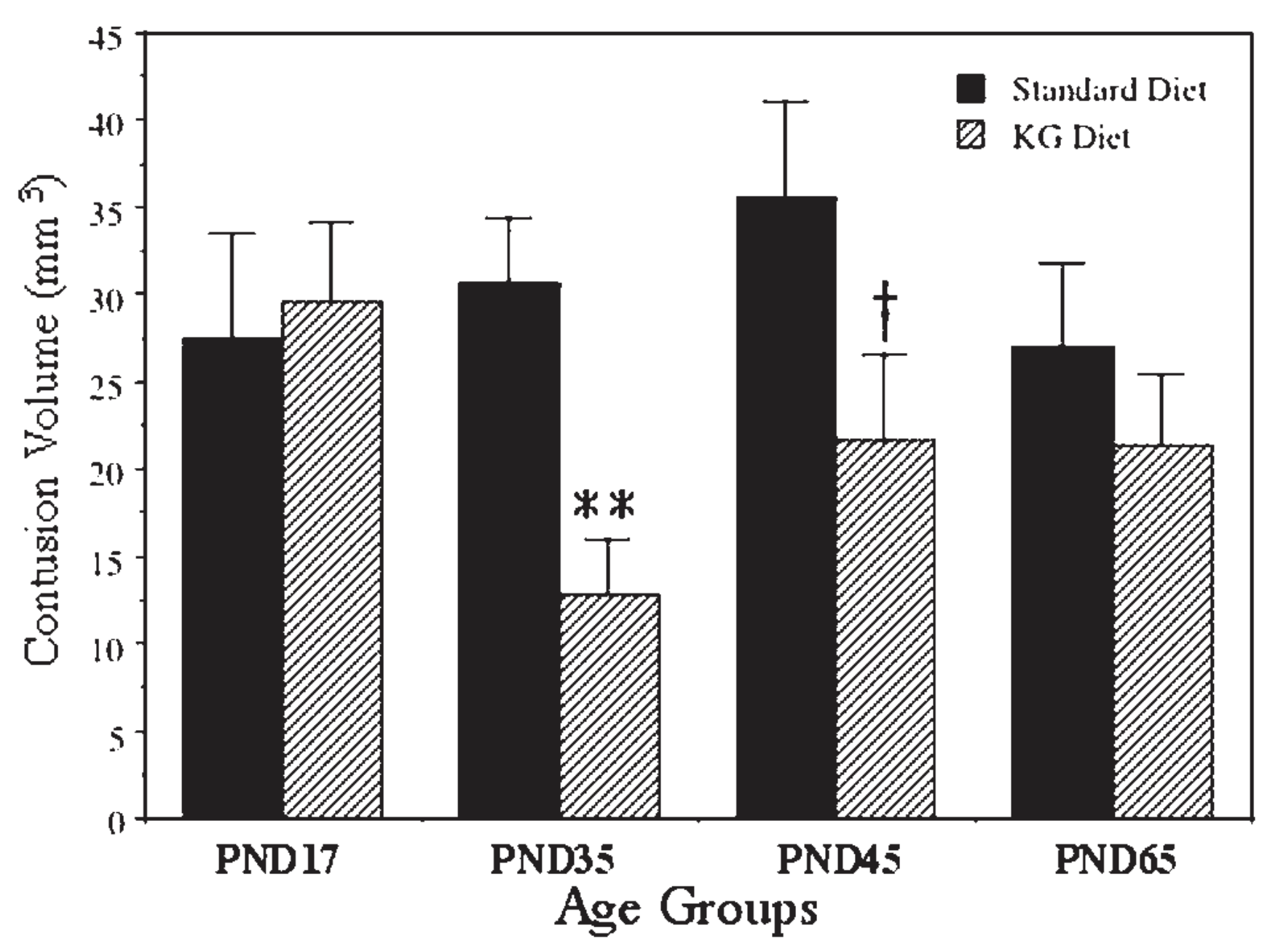
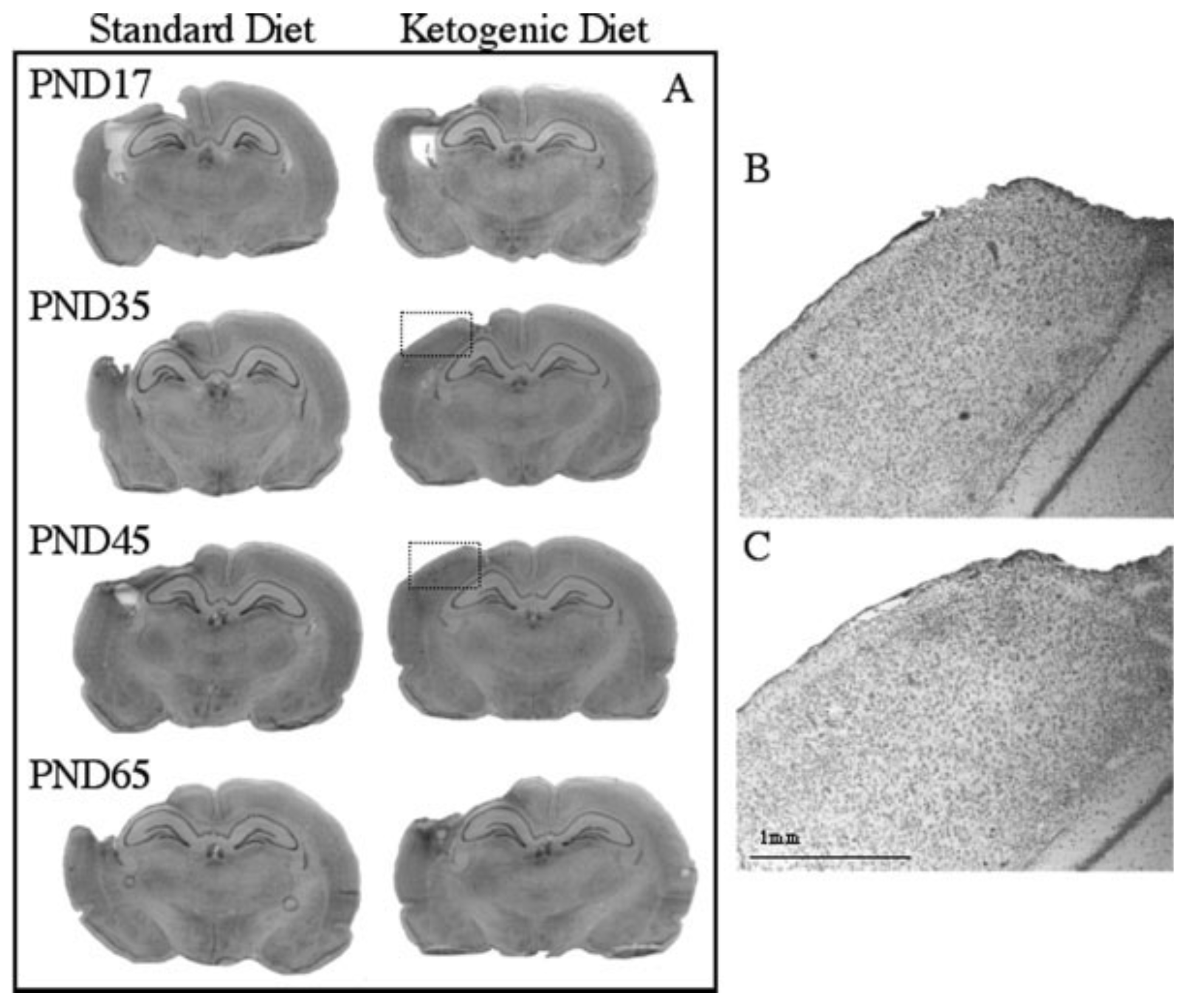
The chart illustrates how a ketogenic diet significantly reduces cortical contusion volume in rats after traumatic brain injury. The protective effects are most pronounced in younger rats (postnatal day 35 and 45), showcasing the age-dependent neuroprotective benefits of ketone metabolism. This finding suggests a greater therapeutic potential for ketone supplementation in younger populations with traumatic brain injuries.[27]
Some of the most compelling evidence for ketone supplementation comes from animal studies examining traumatic brain injury (TBI). These controlled experiments have revealed that ketones don't just serve as an alternative fuel source - they appear to actively protect brain tissue and preserve cognitive function when administered around the time of injury.
-
Improvements from fasting
In a landmark study, researchers found that fasting animals for 24 hours after experimental brain injury - which naturally elevates ketone levels - resulted in significantly improved tissue preservation and cognitive outcomes compared to normally-fed animals.[30] This protection was linked specifically to elevated ketone levels rather than reduced glucose, as artificially lowering glucose with insulin actually worsened outcomes.
-
Greater outcomes when given D-BHB
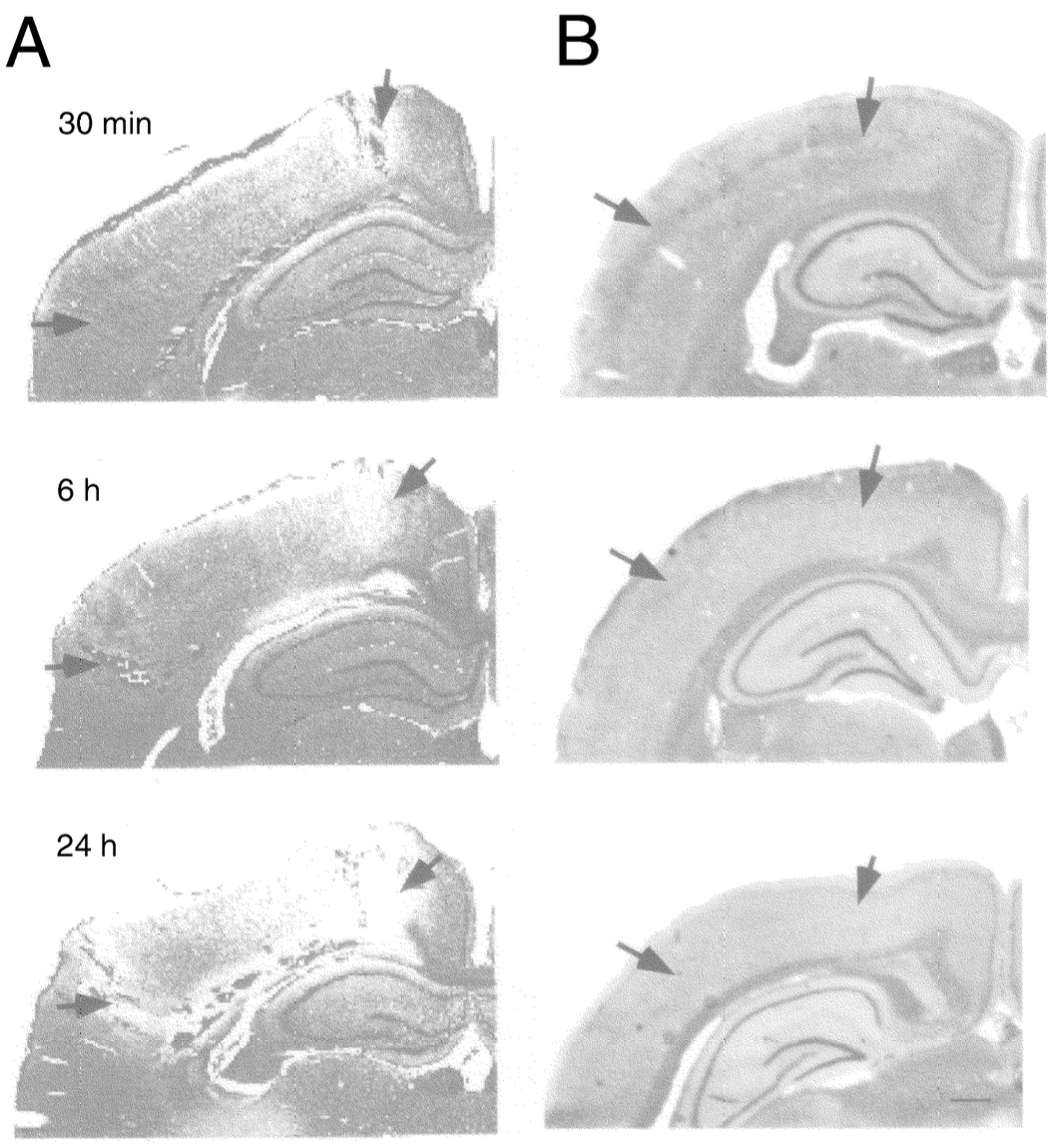
These microscopic images reveal the progression of brain tissue damage following traumatic brain injury (TBI). The images compare fluid percussion injuries, which show minimal degeneration, with controlled cortical impact injuries, where marked degeneration becomes evident 24 hours post-injury. The stark differences highlight the varying severity of brain damage and the critical need for interventions that protect against neuronal loss.[4]
The direct administration of beta-hydroxybutyrate (BHB) has shown similarly promising results. When researchers provided BHB (specifically D-BHB) through mini-pumps immediately after experimental brain injury, they observed significant preservation of brain tissue.[30] Importantly, this protection appeared to have a "sweet spot" - lower doses (0.83 mmol/kg/day) proved more effective than higher doses (1.66 mmol/kg/day), suggesting that careful dosing will be critical for clinical applications.
-
Better effects in younger subjects
The protective effects of ketones appear particularly robust in younger subjects. Studies comparing different age groups found that adolescent animals showed greater neuroprotection from ketone administration than adult animals.[27] This age-dependent response may be particularly relevant for youth sports, where developing brains could potentially benefit most from metabolic protection.
-
Also works well with mild impacts
Perhaps most relevant to contact sports, ketones appear to provide protection even with milder impacts. Research has shown that ketone supplementation between consecutive mild impacts can help preserve cognitive function.[18] This suggests potential benefit not just for diagnosed concussions, but also for the cumulative effects of sub-concussive impacts that athletes experience throughout a season.
Mechanistic Details from Animal Research
The mechanisms align with what was discussed in in the introductory TBI information a few sections above:
-
Improved Oxidative Metabolism and Energy Production
Histological sections reveal the stark differences between standard-fed and ketogenic-fed rats after brain injury. Ketogenic-fed rats exhibit better neuronal preservation and significantly fewer degenerating cells in the cortex and hippocampus. These results highlight the ketogenic diet's ability to mitigate cellular damage and promote recovery in the injured brain.[27]
Recall that when brain tissue is injured, it experiences a significant metabolic crisis - the tissue's ability to process glucose becomes impaired, even as its energy needs skyrocket.[5] Introducing ketones can help address this crisis, thanks to them requiring just 3 steps to make energy as opposed to 10 with glucose.[18] This metabolic efficiency becomes critically important when normal glucose processing is impaired.
-
Better Oxygen Utilization During Crisis
During TBI, oxygen delivery to brain tissue can become compromised due to reduced cerebral blood flow and mitochondrial dysfunction.[18] In this oxygen-limited environment, ketones generate more energy (ATP) per molecule of oxygen consumed compared to glucose.[30] This improved oxygen efficiency means that even in conditions of reduced oxygen availability, ketones can help maintain better energy production in injured brain tissue.
-
Enhanced Uptake After Injury
Additionally, the brain can take up and utilize more ketones after injury, especially when glucose metabolism is impaired,[18] as discussed in the introduction.
-
Protection Against Secondary Damage
Beyond just providing energy, animal studies have revealed that ketones help protect against the cascade of secondary damage that follows the initial injury. They reduce the production of harmful reactive oxygen species, help maintain proper calcium balance within cells, and support the brain's natural antioxidant systems.[30]
These mechanistic insights from animal studies have provided a strong foundation for understanding how ketone supplementation might protect athletes' brains during contact sports. The combination of enhanced energy availability, improved oxygen utilization, and protection against secondary damage makes a compelling case for their potential use in both preventing and treating sports-related brain injuries.
Early Human Studies
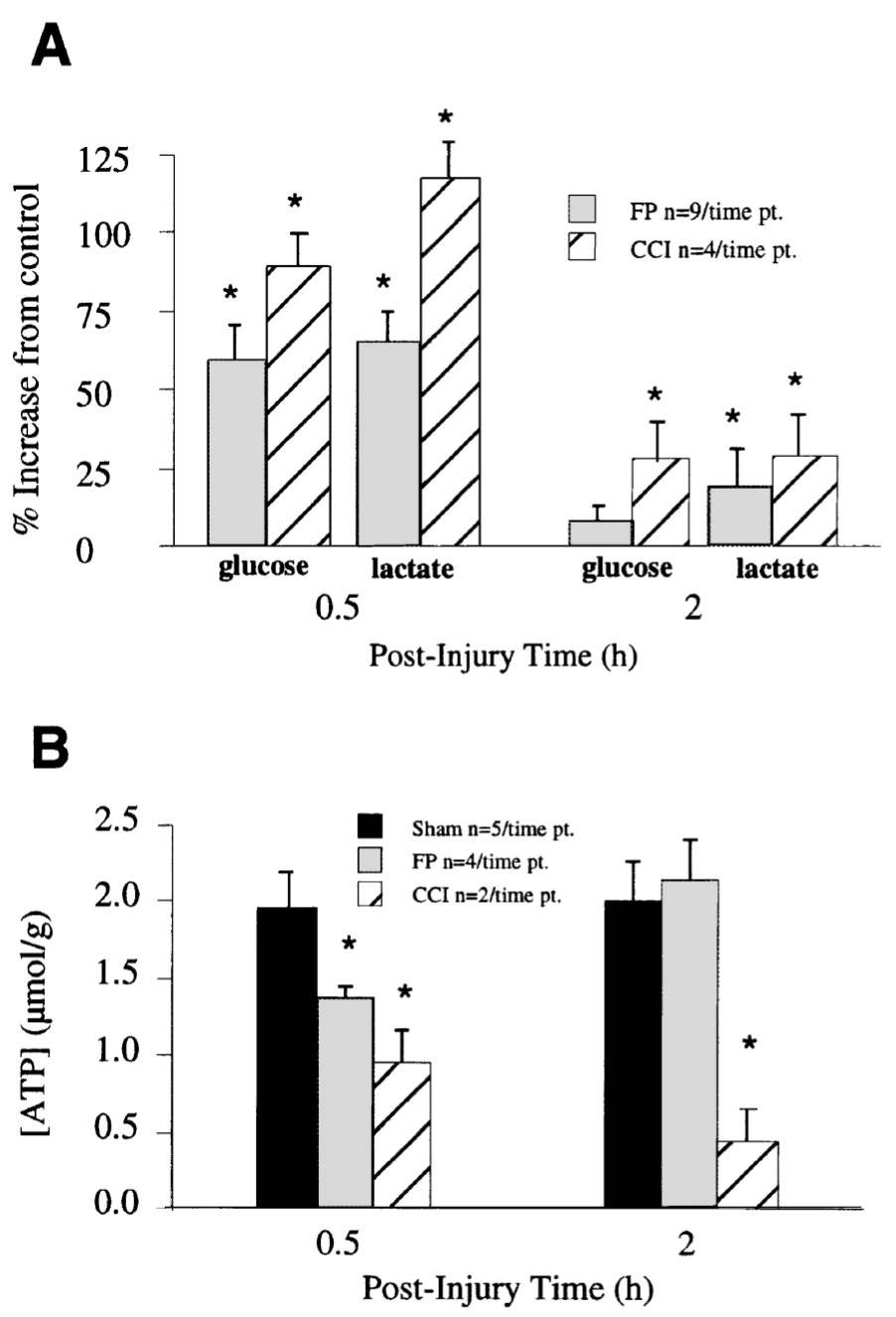
This graph depicts changes in ATP content and glucose utilization following two types of brain injuries: reversible (fluid percussion) and irreversible (controlled cortical impact). While glucose utilization spikes immediately post-injury for both types, ATP levels recover only in reversible cases. Irreversible injuries show sustained ATP depletion, emphasizing the importance of energy restoration in severe trauma scenarios.[4]
Obtaining definitive human research in this area presents unique challenges - researchers cannot ethically conduct double-blinded, placebo-controlled trials to injure and monitor human subjects. However, through a combination of animal research and observational study, we're beginning to understand how ketones might protect the human brain during contact sports.
Clinical studies have shown that fasting-induced ketosis increases the brain's ability to take up and utilize ketones, even in the absence of injury.[31] This foundational work suggests that elevating ketone levels before competition could provide immediately available alternative fuel for the brain.
Some encouraging early evidence comes from clinical studies using microdialysis to sample brain tissue chemistry after injury. These studies have demonstrated that the injured human brain can effectively take up and metabolize ketones when they're available.[32]
However, we still need well-designed clinical trials specifically examining ketone supplementation in athletes. Several trials are currently registered to investigate the effects of exogenous ketones on recovery from sports-related concussions, but results are still pending.
Anecdotal feedback from Ketone Labs
Ketone Labs, the company behind goBHB®, stated the following:
"We have had two kids take goBHB® over the last 2 months after getting concussions and the results were very dramatic -- big time improvement."-- Ketone Labs
While this is anecdotal, given the safety of BHB[33] -- a molecule generated naturally within the body when glucose is limited -- we see no reason why goBHB® supplements shouldn't be tried after a TBI. It's literally the first thing we would reach for.
Practical Applications
The evidence supporting ketone supplementation for brain protection in contact sports, as well as their ultra low-risk nature, presents a compelling case for athletic programs to consider implementing goBHB® supplementation protocols. Let's explore how teams and athletes can practically incorporate this protective strategy.
Recommendations for Athletic Programs
Athletic programs have a responsibility to protect their athletes' brains using the best available methods. While proper technique, rules, and protective equipment remain paramount, supplemental BHB offers an additional layer of metabolic protection that's both safe and potentially game-changing.
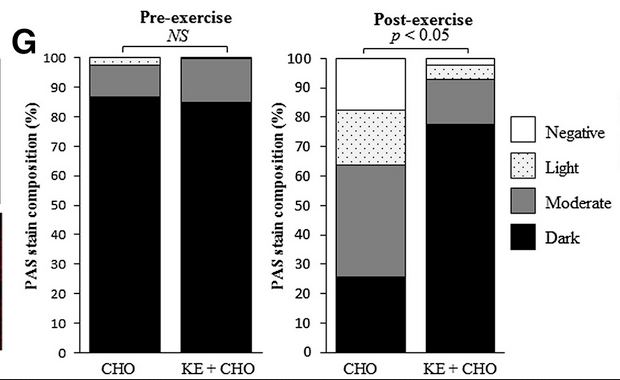
Endurance athletes who consumed a mixture of exogenous ketones and carbohydrates retained far more muscle glycogen after an intensive exercise test.[17]
The beauty of goBHB® supplementation is its dual benefit - not only does it provide potential neuroprotection, but it also delivers performance advantages through enhanced energy availability and reduced fatigue.[28] This creates a "win-win" scenario where athletes can gain both immediate performance benefits and longer-term brain protection.
Consider making BHB part of your standard game-day protocol, similar to how electrolyte drinks are provided. The cost-benefit analysis strongly favors this approach - the potential protective benefits far outweigh the minimal risks, especially given BHB's established safety profile.[33]
Implementation Strategies
For optimal protection and performance benefits, we recommend the following supplementation strategy:
- Pre-Competition (30-60 minutes before): Take 5g of BHB to establish baseline ketone levels in the blood.[14]
- During Competition: For longer events or games with breaks (like halftime), consume additional 2-3g doses to maintain elevated ketone levels.
- Post-Competition: Another 5g dose can support recovery and provide continued protection during the vulnerable post-impact period.[18]
Remember, brain injuries occur on a spectrum - you don't need a diagnosed concussion to benefit from ketone supplementation. Every impact, however minor, can potentially trigger metabolic disruption in brain tissue.[2] Having ketones available as an alternative fuel source provides insurance against these metabolic disturbances.
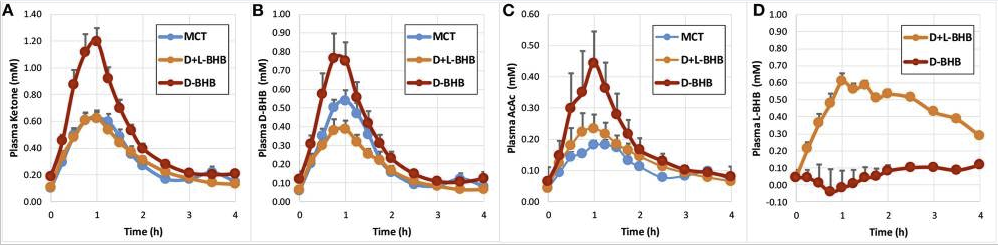
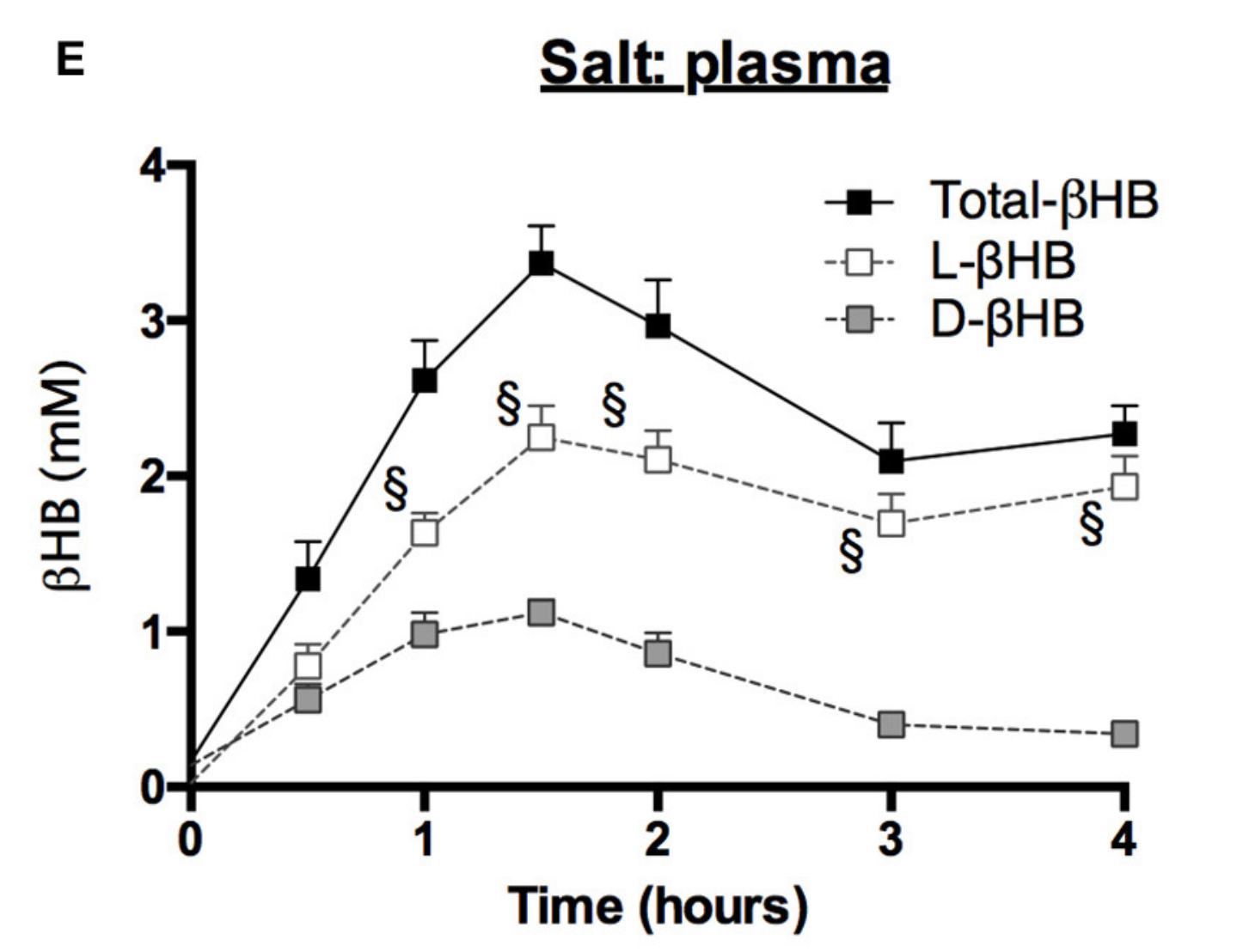
Blood ketone kinetics following gram-matched oral doses of D-BHB, D+L-BHB, and MCT in 15 fasted participants at rest. (A) Plasma ketone, (B) D-BHB, (C) AcAc, and (D) L-BHB levels over 4 h. Values are means + SEM.[34]
Forms of Exogenous Ketones
For practical supplementation in sports, we recommend focusing on two primary forms of goBHB®:
BHB Salts: These combine BHB with essential minerals like sodium and magnesium. They're ideal for pre-game supplementation as they provide both ketones and electrolytes. Available in powder form, they're easy to mix into pre-game drinks.
Free Acid BHB: This pure form of BHB provides rapid ketone availability without additional minerals. It's particularly effective in ready-to-drink formulations and can be ideal for during-game supplementation.
D-BHB and L-BHB
BHB comes in two different isomers -- molecules with the same molecular formula and structure, but different orientation. These are known as L-BHB and D-BHB (R-BHB is also sometimes called D-BHB). Consider them "left-handed" and "right-handed". D/L-BHB is a mix of these two.
While both D-BHB and D/L-BHB mixtures can be effective, research suggests that pure D-BHB may produce higher blood ketone levels per gram consumed.[34] However, this may simply be due to the measurement methods used, as many studies aren't properly measuring L-BHB, and those that do show incredible increases in total BHB levels.[14]
Newer research indicates that D/L-BHB mixtures may offer unique benefits through complementary mechanisms, and L-BHB may have the most cognitive benefits, although that's still subject to ongoing research, which is covered in our article, "Entering the Flow State with L-BHB: Next Generation Nootropic".
So at this time, we're inclined to stick with D/L-BHB formulations, to get the broadest range of benefits from ketones.
Safety Considerations
One of the most compelling aspects of BHB supplementation is its strong safety profile. Both BHB salts and free acid BHB have achieved Generally Recognized as Safe (GRAS) status from the FDA.[36] This means they've been thoroughly evaluated and deemed safe for regular consumption.
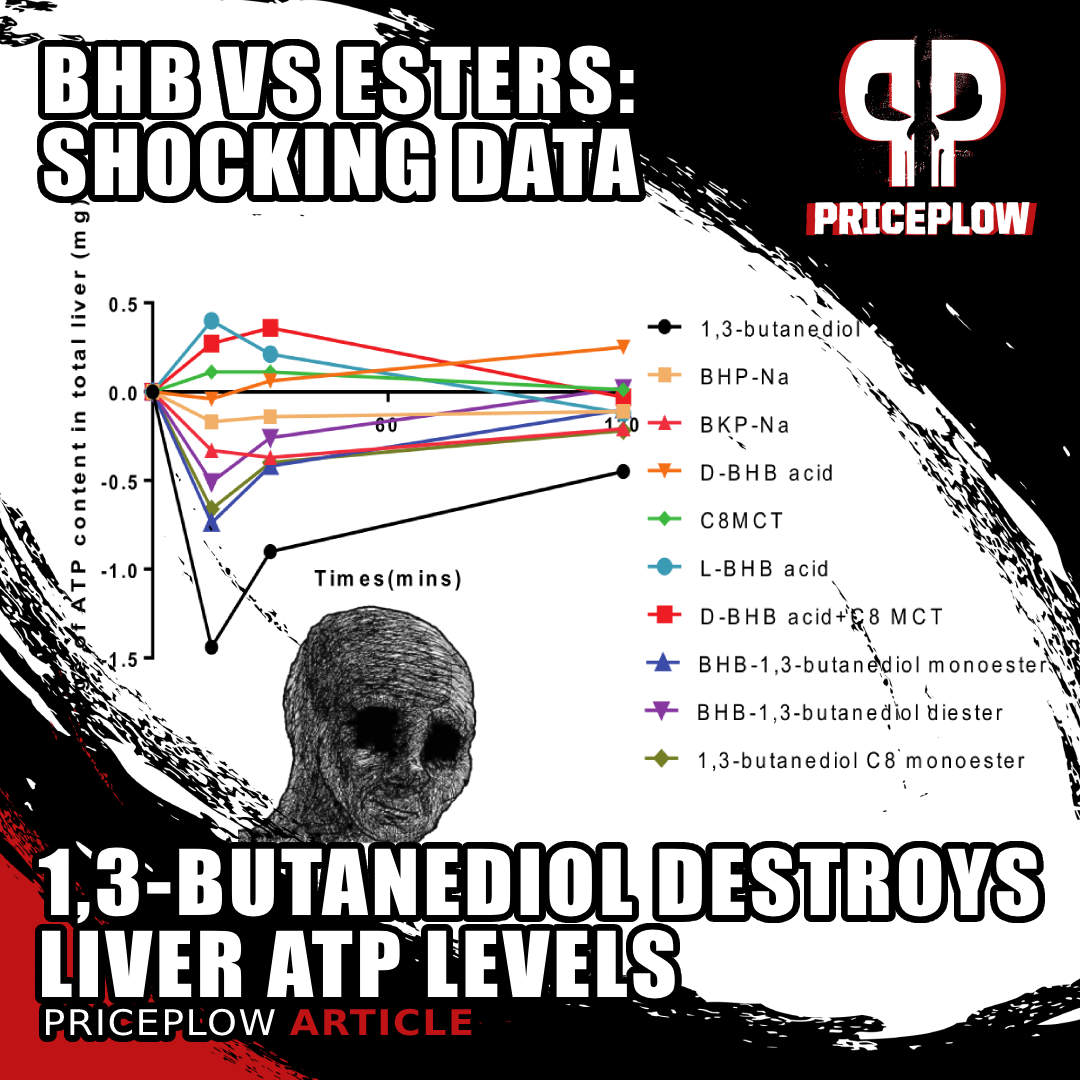
New unpublished preclinical data shows that 1,3-butanediol is a net ATP consumer in the liver, as opposed to free acid BHB and MCT which are ATP (energy) producers.[7] This sheds a whole new light on the BHB vs. Ketone Esters.
Key safety considerations include:
- Start with lower doses to assess individual tolerance
- Monitor hydration status when using BHB salts due to their mineral content
- Ensure proper electrolyte balance by maintaining adequate potassium intake when supplementing with sodium BHB
- Avoid ketone esters, which can have adverse effects on liver function and may not be as safe as BHB salts or free acid forms
On the note of ketone esters, we urge extreme caution, since the most popular forms have ATP-depleting, alcoholic effects. For more details, read our article titled "1,3-Butanediol and Ketone Esters vs Free Acid BHB: Severe Impacts on Liver ATP". Not all ketones work the same, and it's best to stick with the same BHB molecule that's generated within the body naturally.
Future Directions
The promising preliminary evidence for ketone supplementation in contact sports creates an exciting pathway for future research that can be done in parallel to improvements to rules and wearable gear. However, studying traumatic brain injury prevention presents ethical challenges since we can't intentionally subject humans to head impacts. Nevertheless, several promising research directions could help validate and optimize ketone supplementation protocols.
Observational Studies and Registry Data
One ethical approach would be to establish voluntary registry studies of athletic programs that choose to implement ketone supplementation protocols. These could include:
- Multi-team comparative analysis tracking concussion rates, recovery times, and long-term outcomes between programs using ketone supplementation versus traditional approaches.
- Biomarker studies examining blood and cognitive markers in athletes who opt to use ketones versus those who don't, particularly after diagnosed concussions.
- Long-term neurological health tracking of retired athletes who used ketone supplementation during their careers compared to matched controls.
Exogenous BHB is now for everyone—from athletes needing endurance to those boosting brain function. Offering clean, lasting energy, BHB is proving versatile and backed by research.
Preclinical Research Opportunities
While human studies face ethical constraints, several critical questions could be addressed through animal models:
- Comparative efficacy studies between different forms of BHB (D-BHB vs L-BHB vs racemic mixtures) in standardized TBI models.[25]
- Investigation of optimal timing and dosing protocols, including pre-loading strategies versus post-injury administration.[18]
- Examination of potential synergistic effects between ketones and other neuroprotective compounds currently being studied for TBI.[37]
Technological Innovation Needs
Several technological advances could dramatically improve our understanding:
- Advanced neuroimaging techniques to better visualize acute metabolic changes in the brain following impact
- Improved biomarker detection methods for early identification of subtle brain injuries
Clinical Trial Opportunities
While we can't induce TBI in humans, several clinical trial designs could help validate ketone supplementation:
- Randomized controlled trials examining prophylactic ketone supplementation in high-risk sports, with primary outcomes focusing on recovery metrics when injuries naturally occur
- Studies comparing different forms of ketone delivery (salts vs. free acid) for palatability, compliance, and effectiveness
- Investigation of potential benefits in post-concussion syndrome treatment, where the injury has already occurred
The diagram outlines the metabolic pathway of ketone ester supplements. After ingestion, ketone esters are hydrolyzed in the gut, releasing β-hydroxybutyrate (BHB) and 1,3-butanediol. BHB enters circulation to fuel muscles and the brain, while 1,3-butanediol is converted in the liver into additional BHB. This efficient pathway provides a clean, sustainable energy source, making it ideal for use in brain recovery and endurance performance.[28]
Integration with Existing Protocols
Research should also examine how ketone supplementation can be optimally integrated with:
- Current concussion protocols and return-to-play guidelines
- Existing nutritional strategies for athletes
- Standard medical treatments for diagnosed concussions
Economic Impact Studies
Understanding the potential economic benefits could help drive adoption:
- Cost-benefit analyses of preventative ketone supplementation versus traditional post-injury care
- Impact on insurance costs for athletic programs
- Economic modeling of reduced recovery times and improved long-term outcomes
A low-risk, high-reward addition to current protocols
The field of ketone supplementation for brain protection in contact sports is still in its early stages. This is one of those times where many of us in the know are ahead of the curve, and given the safety of these ingredients,[33] we see no risk in moving forward. However, it will take years before highly-validated research exists -- and we're not interested in waiting around for data before providing quality nutritional support for young athletic brains.
While ethical considerations create certain research limitations, numerous opportunities exist to build our understanding through carefully designed studies. As technology advances and our ability to detect and measure subtle brain changes improves, we'll be better positioned to validate and optimize these promising protocols.
Conclusion: A Call to Action for Sports Medicine Professionals
Fuel your workouts with the power of "dual fuel", combining goBHB ketones and carbs for optimal performance.
As the evidence mounts for ketone supplementation's potential role in protecting athletes' brains, sports medicine professionals face an incredible, brain-saving opportunity. While protective equipment and rule changes remain essential, we now have a metabolic approach that could provide an additional layer of defense for our athletes' most vital organ.
The mechanistic data strongly supports their use, and there's virtually no downside to implementation, given their safety profile and ability to provide more energy that's not in the form of glucose. Just as we wouldn't send athletes onto the field without proper electrolyte balance, perhaps it's time to consider ketone supplementation as part of our standard protocols.[20]
This is especially true given the "dual fuel" possibilities that ketones provide alongside traditional carbohydrate-based nutrition strategies. Ketones are an addition, not a replacement, so athletes can maintain their existing nutrition protocols while adding ketones as a supplementary fuel source, potentially improving both performance and protection.[28]
When it comes to selecting the right form of ketone supplementation, the research currently points towards a combination of both D-BHB and L-BHB. While D-BHB has traditionally been favored for its metabolic effects, emerging evidence suggests that L-BHB may provide enhanced neuroprotective benefits. This balanced approach, available through goBHB® supplementation, offers a comprehensive solution for athletes looking to support both performance and brain health.
Flow State in a bottle?! With the new L-BHB free acid ingredients from Ketone Labs, we're starting to believe it. Understand how this energy-providing ketone isomer may work better for nootropic (cognitive) applications!
Looking ahead, we believe ketone supplementation could become a standard component of contact sport protocols, much like how creatine supplementation evolved from a performance enhancer to a recognized neuroprotective agent. The science supporting ketones' role in maintaining brain energy metabolism during crisis, reducing inflammation, and supporting mitochondrial function makes a compelling case for their inclusion in any comprehensive brain protection strategy.[18]
For sports medicine professionals interested in implementing ketone supplementation protocols, we encourage exploring the growing body of research and product information available through PricePlow's extensive coverage of Ketone Labs' goBHB® products and research. The future of brain protection in contact sports may well depend on our willingness to embrace metabolic solutions alongside traditional physical protection strategies.




Comments and Discussion (Powered by the PricePlow Forum)