Beta Hydroxybutyrate (BHB) is a ketone body that your cells can use for energy, especially when glucose is unavailable. They've gained recognition from discussions of the ketogenic diet, and you can think of ketones as the fourth macronutrient, after protein, fat, and carbohydrates.
Exogenous BHB is now for everyone—from athletes needing endurance to those boosting brain function. Offering clean, lasting energy, BHB is proving versatile and backed by research.
When the body is deprived of dietary carbohydrates, it enters a state of ketosis, in which the body burns fat (both dietary and stored body fat) to produce highly energetic molecules called ketones. In this state, the body readily utilizes ketones as its primary energy source -- they serve as a powerful alternative to glucose. A diet that aims to create ketones and maintain this state for a prolonged period is generally called a ketogenic diet, shortened to "keto diet".[1]
Compared to the standard American diet (SAD), research has demonstrated several potential health benefits from ketogenic dieting, especially in metabolically distressed individuals. These benefits include weight loss,[2-13] better glycemic control,[5,6,10-14] improved metabolic and lipid biomarkers,[7-9] reduced liver disease,[10] enhanced cognition,[15,16] better appetite,[17] sleep,[18] and even improvements in skin quality.[19]
However, not everyone can (or wants to) adhere to the high-fat, low-carbohydrate, moderate-protein diet traditionally used to produce ketones and maintain the state of ketosis. So, can we achieve some of the benefits of ketones without strictly following a ketogenic diet?
Ketones For Everyone, Not Just Keto Dieters
While your cells can produce BHB on their own during a period of carbohydrate restriction, thanks to modern scientific advancements, we can now take ketones exogenously as dietary supplements. There's an interesting history behind this discovery, and if you'd like to learn more, check out Episode #131 of the PricePlow Podcast with Rob Rogers of Ketone Labs, where we hear the story of how BHB supplements were brought to market.
Seeing the benefits that dieters attain when switching from a SAD diet to a keto diet, the main question faced is, "Are the benefits coming from the ketones, or from the reduction of glucose and insulin?" The answer is a bit of both, but for healthy individuals and athletes who occasionally enjoy entering a state of ketosis, it's primarily the former -- exogenous BHB supplementation comes with several benefits.
Can we get those BHB benefits without drastically changing our diets? Absolutely.
In this article, we detail the benefits of exogenous ketone supplementation, focusing specifically on BHB salts and BHB free acids, which are marketed as goBHB by Ketone Labs. We also discuss some of the differences among the various ketone supplements available on the market, as well as some of the pitfalls to watch out for.
Benefits of BHB Supplementation
Before beginning, let us clarify that this article primarily addresses exogenous BHB supplements. The keto diet studies cited in the introduction are valuable, but we're more interested in supplementation without significant dietary changes.
So what can exogenous BHB do for us? Let's take a look:
Preventing blood sugar swings
Anyone who's experimented with a continuous glucose monitor (CGM) can probably tell you that drops in blood sugar often correlate with feelings of nervousness or anxiety. Many individuals using CGMs have reported that BHB supplementation can substantially reduce those periods, often referred to as the "blood sugar rollercoaster".
This is supported by multiple animal studies indicating that BHB supplementation can help decrease the severity of anxious behavior.[20,21] Research on both humans and animals has consistently shown that exogenous BHB lowers blood sugar levels,[22-27] stabilizing blood sugar fluctuations.
Supports Brain Health, Fights Anxiety
We should start by discussing BHB's most pronounced and arguably important effects, which occur in the brain. Under "normal" conditions (i.e., the mixed-macro feeding pattern of the Standard American Diet), the brain is highly sensitive to fluctuations in blood glucose levels, as neurons depend on glucose for energy.
-
Benefits for Brain Health
One preclinical study in mice showed that BHB actually prevented the onset of neurodegenerative illness in the animals. More specifically, the study was carried out in 3xTgAD mice, which are bred for a predisposition to developing amyloid and tau proteins, which can aggregate and form neurotoxic plaques.[20]
In the study, one group of plaque-disposed mice was fed a carbohydrate-predominant diet, while the other group raised its serum BHB levels through ketone consumption. Throughout the entire study period, the ketone group performed significantly better on a battery of cognitive tests than the carbohydrate group.[20]
According to the authors of the study, the most likely explanation for this is the beneficial impact that higher serum BHB levels had on the mice's neuronal mitochondrial function, as well as its anti-inflammatory effects.
As the literature has progressed, authors of two recent research reviews have independently state that:
- "It is widely accepted that ketosis (increased blood ketone body levels, e.g., β-hydroxybutyrate) can generate neuroprotective effects"[28]
- Administration of exogenous ketone supplements, such as ketone salts, "generates rapid and sustained nutritional ketosis and metabolic changes, which may evoke potential therapeutic effects in cases of central nervous system (CNS) disorders, including psychiatric diseases."[29]
We strongly believe that this goes well beyond mere blood glucose regulation, however. For instance, both reviews cited above discuss improved mitochondrial function and enhanced neurotransmitter levels.[28,29] This leads us to a new field of benefits:
-
Mitigates Traumatic Brain Injury (TBI) and Concussion Damage
All trauma to the head, however slight, has the potential to initiate a neurometabolic cascade that impairs neuronal health and function.[30]
Rob Rogers of Ketone Labs joins PricePlow for Episode #131 to explain the story behind goBHB, and how they're BACK on the market for supplement formulators!
The primary mechanism is physical trauma's tendency to disrupt neurons' ability to burn glucose, which represents an enormous potential threat to your precious, irreplaceable brain cells – remember, they need a constant supply of energy in order to survive and flourish. If these cells lose the ability to metabolize sugar, they may be at serious risk of death,[30] and that neuronal loss is a significant factor in the occurrence of brain damage following head trauma.
In this context, exogenous BHB has the potential to spare neurons from this grim fate – if the neurons have ketones available to burn instead of glucose, they can survive the metabolic disruption caused by the trauma, ultimately mitigating any potential brain damage.[31]
Despite the paucity of human studies on this subject,[32] some animal research has been conducted that's extremely promising. Generally, it shows that exogenous BHB supplementation can significantly reduce the extent of brain tissue damage following a TBI.[31,33]
Athlete prophylactic?
We discussed this in the aforementioned Episode #131 with Rob Rogers, who pointed out that exogenous BHB supplements could be administered to athletes prior to games as a preventative measure, while also providing performance-boosting fuel. Food for thought (and your brain).
We go deeper into this topic in our article, "The Case for Ketone Supplementation in Contact Sports: A Game-Changer for Brain Protection".
-
Neuropsychiatric Benefits
Although mental illness remains incompletely understood, the most cutting-edge research suggests that neuroinflammation plays an important role in depressive syndromes and symptoms. In connection with that, it's worth mentioning that BHB can decrease the expression of inflammatory regulators such as interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α), which have been implicated in the pathophysiology of depression. It's no surprise, then, that BHB supplementation can significantly reduce the severity of depression-related behaviors.[34]
In one study, rodents that were administered exogenous BHB performed significantly better on tests of mental and physical stress resistance, such as the forced swim test (FST) and open field test (OFT).[35]
-
Appetite Regulation
Fuel your workouts with the power of "dual fuel", combining goBHB ketones and carbs for optimal performance.
The metabolic benefits linked to exogenous BHB consumption have knock-on effects as well. For example, a 2017 study showed that BHB supplementation can lead to significant reductions in appetite, insulin, and ghrelin,[36] which is essentially the hormone that stimulates hunger. Generally, the more ghrelin present in your blood, the stronger your desire to eat will be.[37]
In light of this finding, it makes a great deal of sense that keto dieters report feeling less hungry when following this way of eating!
Body Composition
Although several studies examine the link between the keto diet and fat loss, human findings on exogenous BHB remain indeterminate. However, animal research provides compelling reasons to believe that supplemental BHB could help us lose excess weight and maintain that loss.[38]
In one such study, overfat mice that consumed a high-fat diet for 10 weeks exhibited a higher basal metabolic rate (the rate of energy expenditure at rest) and lost substantial amounts of fat when administered BHB supplements for an additional 12 weeks.[38]
This may sound like it follows the familiar keto research pattern: subjects consuming a low-carb, mixed-macro diet who lose fat by becoming fat adapted. However, the truly interesting aspect of this study is that the animals were already fat adapted prior to the study's start. This implies that exogenous BHB confers additional metabolic benefits, beyond those observed from endogenous ketone production through nutritional ketosis.
Cardioprotective
A human study published in 2017 found that exogenous BHB administration can significantly decrease blood glucose, free fatty acids, and triglyceride levels.[22] All three of these are biomarkers for cardiovascular disease risk, suggesting that BHB may support the health and function of the cardiovascular system.
This was confirmed by another study, which demonstrated that six weeks of exogenous BHB supplementation significantly lowered blood pressure in subjects aged 18 to 35.[39]
Reduces Visceral Fat
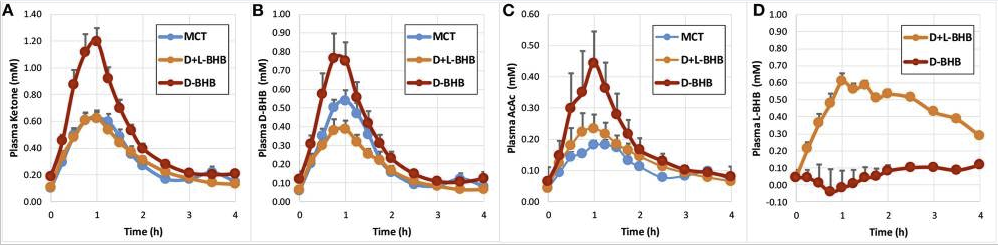
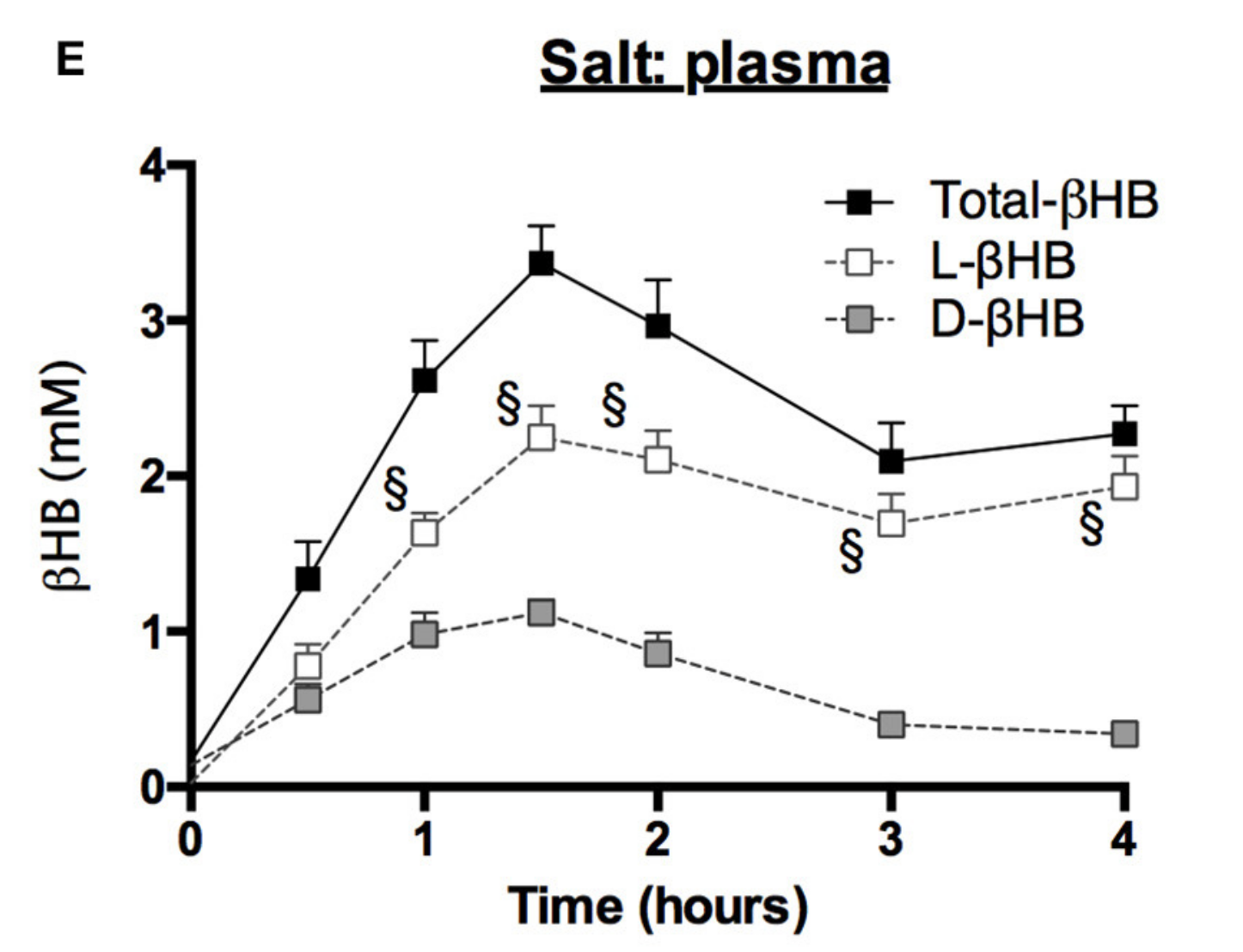
Blood ketone kinetics following gram-matched oral doses of D-BHB, D+L-BHB, and MCT in 15 fasted participants at rest. (A) Plasma ketone, (B) D-BHB, (C) AcAc, and (D) L-BHB levels over 4 h. Values are means + SEM.[40]
In another 2017 study, BHB supplements improved blood lipids and decreased visceral fat in rats.[41] This is a significant finding, as visceral fat mass strongly correlates with insulin resistance and metabolic syndrome. The development of these conditions can have a devastating impact on cardiovascular health.
The study reported higher HDL cholesterol, lower LDL cholesterol, and lower triglycerides – the holy grail of cardiovascular health.[41] There's a substantial body of peer-reviewed evidence showing that a low HDL to triglyceride ratio is associated with insulin resistance.[42-47]
We consider HDL cholesterol to be your "metabolic report card", and while the pharmaceutical industry excels at lowering LDL cholesterol, it doesn't fare nearly as well in safely elevating HDL cholesterol. So when we find a dietary supplement that safely improves HDL levels, we take note.
Improves Metabolic Flexibility
Arguably, the coolest thing about exogenous BHB is that it decouples the benefits of ketosis from the ketogenic lifestyle – exogenous ketones work regardless of whether you're in a state of nutritional ketosis.[48]
No matter how many carbs you're eating, how much you're eating, or when you're eating, exogenous BHB administration can offer you the benefits of endogenous ketone production.
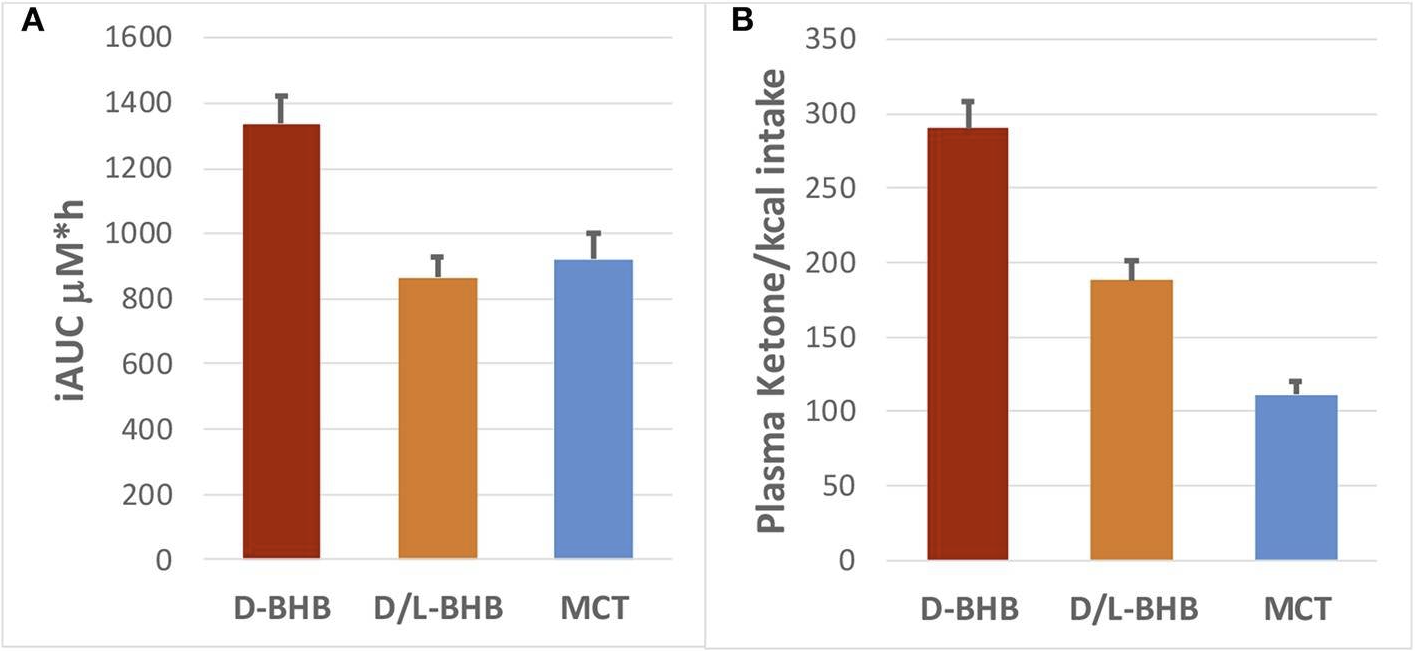
(A) Plasma ketone iAUC (μM*h) for D-BHB, D+L BHB and MCT, and (B) their respective ketone production per calorie consumed (iAUC/kcal).[40]
This includes metabolic flexibility, which is the ability of your cells to burn either fat or glucose for energy. Studies dating back to the early 90s have found that exogenous BHB can spare glucose by serving as an alternate fuel source.
In practice, this means that if you're an endurance athlete who's carb-loading for an event, taking a BHB supplement can help preserve your precious glucose supply from being burned by lower-intensity efforts, thereby keeping it available for the high-intensity efforts where it's absolutely necessary. For athletes, this adds up to decreased lactic acid production and improved aerobic endurance.[49]
This isn't surprising, since lactic acid (a.k.a. lactate) is a byproduct of anaerobic glucose metabolism and is known to induce muscular fatigue as it accumulates. Even during aerobic exercise (defined as an intensity level under the individual's lactate threshold), some anaerobic metabolism takes place. By encouraging your body to burn fat instead of glucose, exogenous BHB can decrease lactate formation and increase endurance during aerobic activity.[50]
BHB in Athletes
Although the studies on this topic are few, it appears that BHB administration in human athletes can indeed improve aerobic performance through glucose sparing.[51] However, high-intensity (anaerobic) efforts seem to be relatively unaffected.[52,53]

Beyond new energy drinks, there are tons of applications to consider with BHB, and formulators can now license goBHB to make their own
One interesting benefit for athletes is BHB's potential to mitigate or prevent the temporary cognitive decline that typically follows hard athletic efforts.[53]
Muscle Building
Studies dating back to 1988[54] have demonstrated how BHB can also support muscle growth. It does this in two ways: not only does it increase muscle protein synthesis (MPS), but it also decreases the breakdown of existing muscle tissue and the oxidation of amino acids like leucine, allowing them to remain intact to stimulate MPS.[55,56]
In other words, BHB is both protein-sparing and muscle-sparing.
Supports ketogenic or intermittent fasting lifestyles
If you're still committed to the intermittent fasting and/or ketogenic lifestyle, you may have to contend with drops in energy -- especially during the initial adaptation phase. This makes exogenous BHB supplementation a great stopgap. By supplying your body and brain with ketones, you can keep them powered without disrupting your fast or your adaptation to ketosis.
Some research has shown that the administration of medium chain triglycerides (MCTs), which the body converts directly into ketones like BHB, can significantly decrease the severity of keto-induction (also known as the keto flu).[57] MCT is just not as powerful as BHB.
Sleep Benefits
While most people associate beta-hydroxybutyrate (BHB) with energy production and cognitive enhancement, recent research has revealed another compelling benefit: improved sleep quality.
A 2025 randomized, double-blind, placebo-controlled study published in Bioscience, Biotechnology, and Biochemistry found that supplementing with D-BHB before bedtime significantly improved multiple sleep parameters in adults experiencing temporary fatigue and poor sleep.[18]
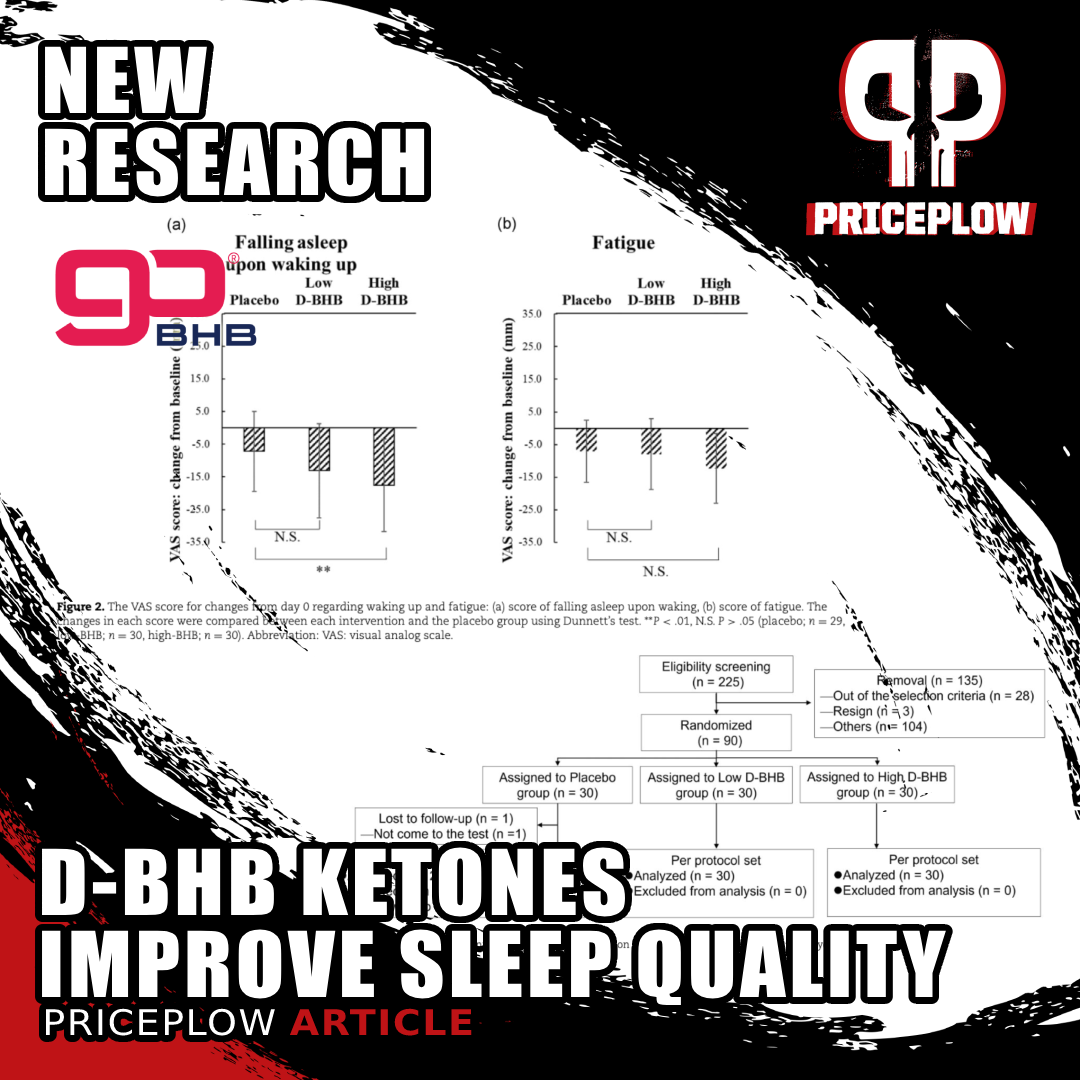
New research shows BHB ketones can significantly improve sleep quality! Study found 1.5-2.9g of D-BHB taken before bed enhanced multiple sleep parameters including easier falling asleep and feeling more refreshed upon waking.[18]
Key Study Findings
The Japanese research team enrolled 90 participants and divided them into three groups:
- Low D-BHB group (1.5g)
- High D-BHB group (2.9g)
- Placebo group
After 14 days of supplementation taken one hour before bedtime, researchers observed significant improvements in four key areas of sleep quality:[18]
- Easier sleep initiation and maintenance - Participants in the low-dose group (1.5g) found it easier to fall asleep and stay asleep throughout the night, with approximately 10% improvement compared to placebo.
- Increased dream frequency - Both dosage groups experienced 8-10% more dreaming, suggesting enhanced REM sleep, which is crucial for cognitive function and emotional processing.
- Reduced morning grogginess - Both groups reported feeling less sleepy upon waking, with scores improving by 9-10% compared to placebo.
- Feeling more refreshed - The high-dose group (2.9g) reported an 8% improvement in feeling refreshed upon waking, indicating better sleep quality and recovery.
What's especially noteworthy is that these benefits occurred without changing overall sleep duration -- BHB improved sleep quality rather than just extending sleep time. The effects were even more pronounced in participants with poorer baseline sleep quality, suggesting those with sleep disturbances may benefit most.
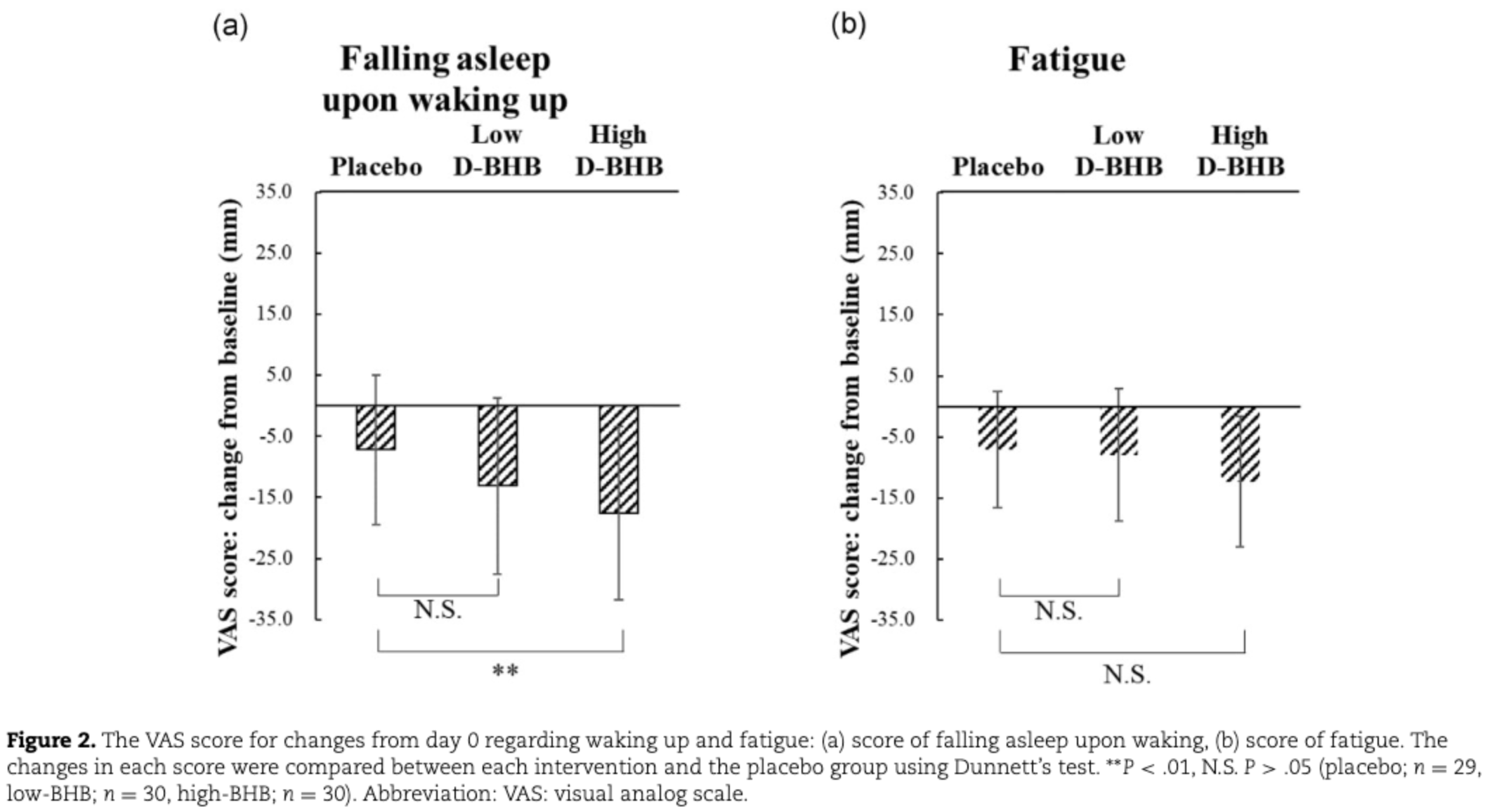
This graph reveals one of the key findings from the ketone sleep study - the significant improvement in "falling asleep upon waking" scores. The chart shows how the high-dose D-BHB group (2.9g) experienced substantially greater improvement in this metric compared to placebo, indicated by the statistically significant difference (**P < .01). While both BHB groups showed improvements in fatigue scores as well, the effect on sleep transition quality was most pronounced. These visual analog scale (VAS) measurements provide clear evidence that ketone supplementation before bed can help people feel more alert and refreshed upon waking.[18]
This study and the potential mechanisms are discussed in greater detail in our article, "Sleep Deeper with D-BHB: Research Confirms Ketone Supplement Improves Sleep Quality".
With such a great number of benefits, we're excited to see BHB supplements making a mainstream comeback -- they're clearly not just for keto dieters.
But what are the differences between the various forms of BHB supplements, and which ones should you consider taking?
The Different Forms of BHB (Salts, Free Acids, Esters)
Not all BHB is created equal. While all forms can increase blood BHB levels, some do so more effectively than others -- while others unfortunately leave a disaster in the liver in their wake.
-
D-BHB vs. D/L-BHB
Flow State in a bottle?! With the new L-BHB free acid ingredients from Ketone Labs, we're starting to believe it. Understand how this energy-providing ketone isomer may work better for nootropic (cognitive) applications!
First, we must distinguish between the two enantiomers of BHB: L-BHB and D-BHB (sometimes known as D/R-BHB). Enantiomers are like your left and right hands—they're mirror images of the same molecule, but have different orientations. While they contain the same atoms and bonds, the way they're arranged in space is different, meaning they can behave differently in biological systems.
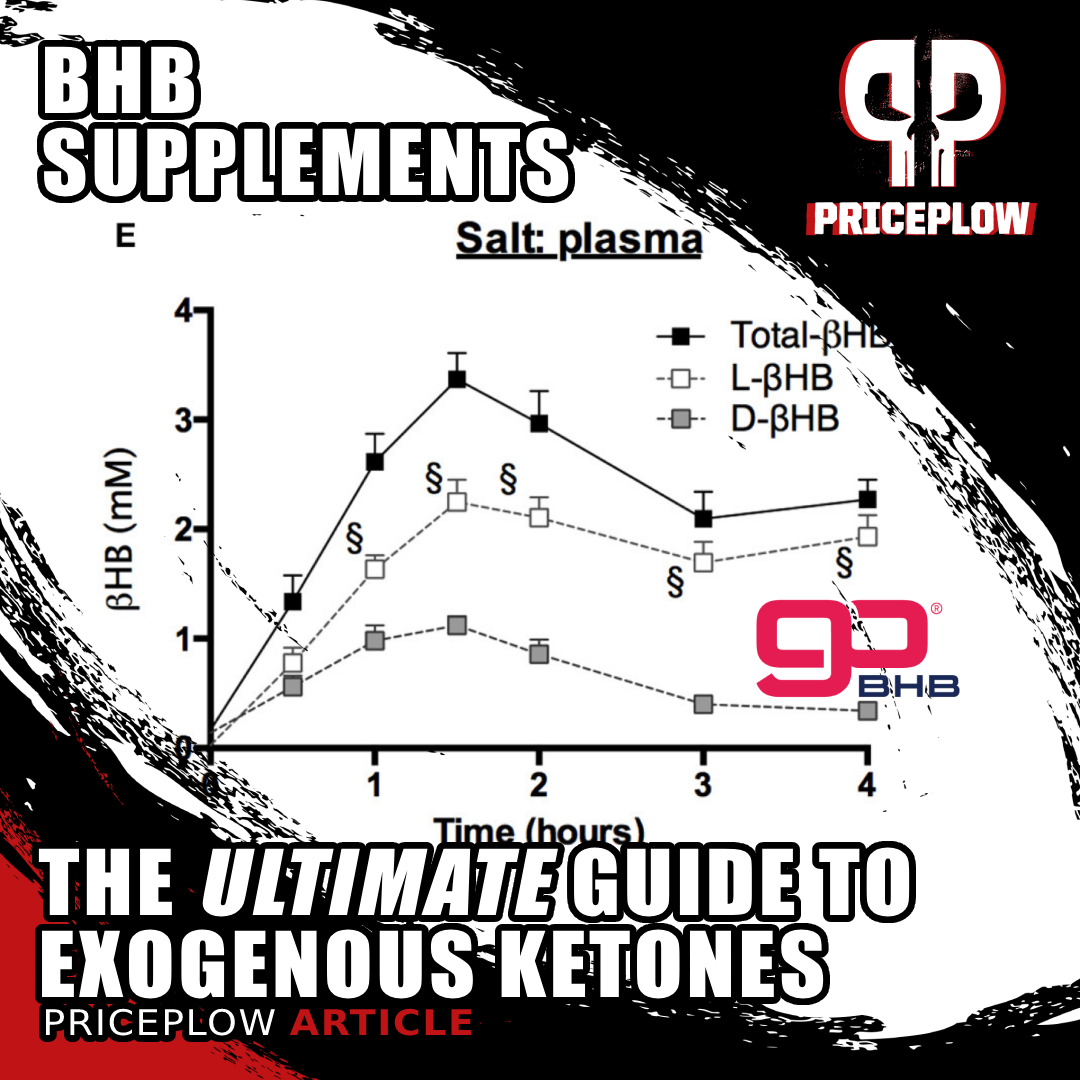
Most individuals looking to increase their measurements of blood BHB levels opt for D-BHB, which has been shown by several research studies to produce more ketones measured in the blood. In one of these studies, researchers compared the ketogenic effects of:[40]
- D-BHB
- D/L-BHB (a mixture of D-BHB and L-BHB), and
- MCT (medium-chain triglycerides).
D-BHB raises blood ketone levels more than MCT
The pure D-BHB was found to be much more ketogenic, raising blood ketones to significantly higher levels while providing fewer calories.[40] After consuming D-BHB, blood ketone levels increased significantly, reaching a peak concentration (Cmax) of 1.2 mM, compared to 0.62 mM for both D+L-BHB and medium-chain triglycerides (MCT). So D-BHB produced approximately 1.7x higher blood ketone levels than the racemic BHB mixture or MCT.[40]
D-BHB was not only shown to produce significantly more ketones – it also, crucially, provided more ketones per calorie consumed. The figure for ketones per calorie was 2.6 times higher for D-BHB than for MCT due to the lower caloric density of D-BHB (4.6 kcal/g) compared to MCT (8.3 kcal/g), and the area-under-the-curve (iAUC) of ketone levels over 4 hours was 1.5x higher for D-BHB compared to D+L-BHB and MCT.[40]
Measurement methods matter: D/L-BHB Increases Both
However, this all may come down to measurement methods. Research has also shown that ingesting D/L-BHB, which is half D-BHB and half L-BHB, will unsurprisingly increase both, and the combined total is dramatic.[22]
When measuring both D-BHB and L-BHB in plasma, D/L-BHB's total BHB concentrations are significantly larger.[22] So has conventional wisdom of D-BHB's 'superiority' simply been due to measurement methods?
While we've been exploring the benefits of L-BHB as a potential nootropic (also discussed in both Episodes #131 and #138 of the PricePlow Podcast), pure D-BHB remains the trusted go-to. The comparison study cited above[40] explains that L-BHB (also sometimes known as S-BHB) is "not metabolized significantly into energy intermediates".[22,40,58] L-BHB has shown great promise as a nootropic ingredient, and scientists are beginning to dispute those statements regarding energy metabolism - there is still much to be explored.
But it goes further than just left- or right-handed orientation:
-
Free Acid BHB vs. BHB Salts vs. Ketone Esters
There are three primary forms of BHB supplements on the market:
BHB Salts
BHB Salts are formed by binding beta-hydroxybutyrate to mineral ions such as sodium, magnesium, calcium, and occasionally potassium. These salts are popular exogenous ketone supplements because they not only provide BHB to increase ketone levels but also supply essential electrolytes that can be depleted during ketosis.
For example, sodium and magnesium are critical for nerve function and muscle contractions. However, consuming large amounts of BHB salts can lead to an excessive intake of these minerals, which may be a concern for individuals monitoring their mineral consumption.
Gary Millet of Ketone Labs / goBHB joins the PricePlow Podcast for Episode #138 to talk about the future of BHB research and exciting new applications to come.
BHB salts are widely available as goBHB, and we enjoy sodium and magnesium BHB especially, just noting to maintain appropriate sodium to potassium ratios in our diets.
However, as beverages become more popular, a new form of BHB is taking over the market:
Free Acid BHB
Also sold as goBHB, Free Acid BHB is the pure form of beta-hydroxybutyrate without any mineral ions attached. In its liquid form, it's more readily absorbed by the body because it doesn't need to dissociate from a salt compound during digestion. This allows for quicker elevation of blood ketone levels, providing a rapid source of energy.
Free Acid BHB is also advantageous for those who wish to avoid excess intake of minerals like sodium or calcium that are present in BHB salts. Its relatively neutral taste and liquid formulation make it a convenient option for inclusion in beverages like energy drinks (for example, Vault Caffeine-Free Energy Drinks).
Ketone Esters (beware!)
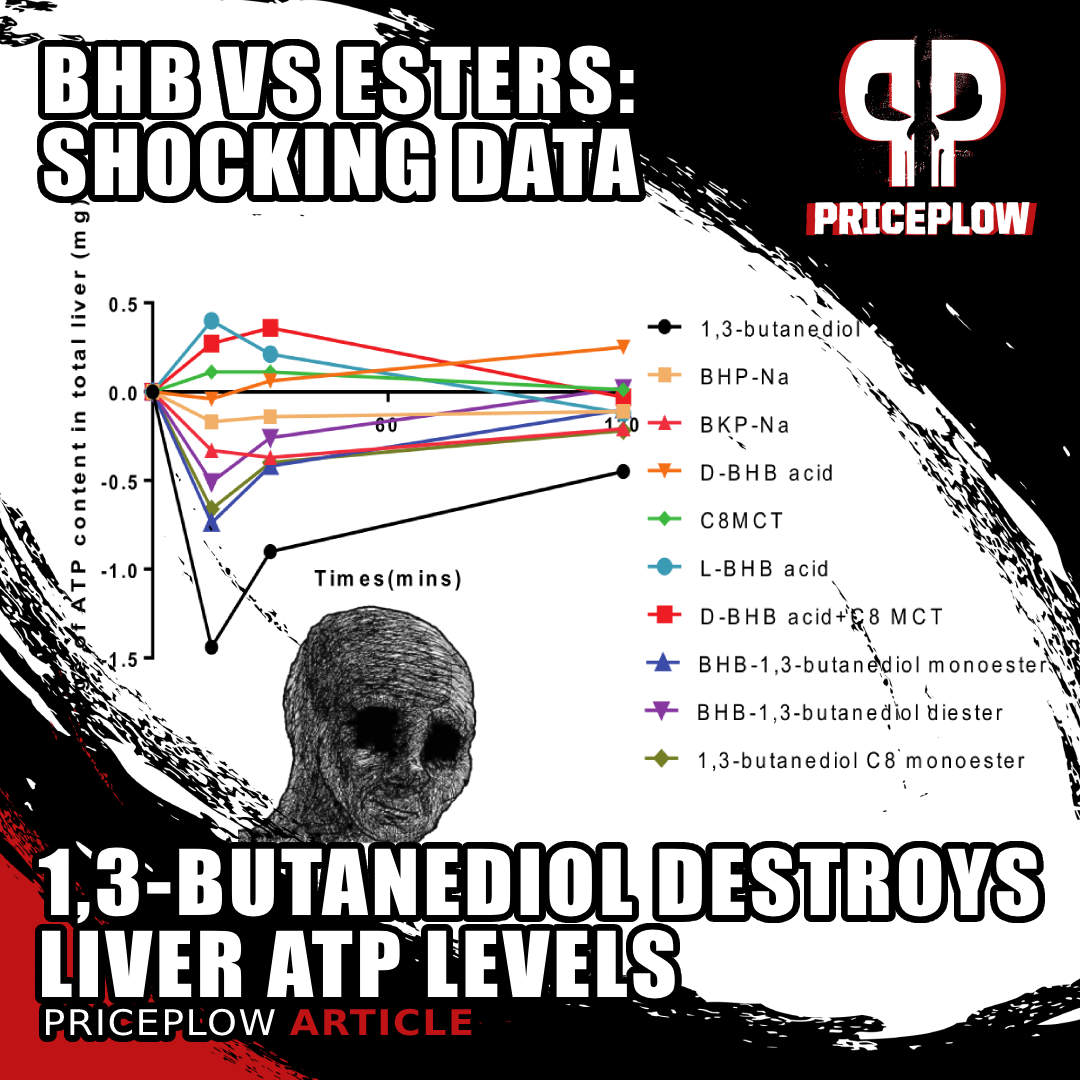
Ketone esters are compounds in which beta-hydroxybutyrate is chemically bonded to an alcohol molecule, typically sold as 1,3-butanediol. Ketone esters can significantly raise blood ketone levels, but they have a major problem aside from their extremely unpleasant taste: when ingested, they're metabolized in the liver to release BHB -- along with the alcohol component!
This raises significant safety concerns because 1,3-butanediol behaves similarly to alcohol in the body, potentially harming liver function. Earlier this year, we discussed new data demonstrating that 1,3-butanediol depletes liver ATP levels, whereas free acid D-BHB, free acid L-BHB, and MCT increase ATP. This is akin to robbing Peter to pay Paul, and it's not a good long-term solution.
The above article details the numerous side effects of these ketone esters,[59-63] specifically:
New unpublished preclinical data shows that 1,3-butanediol is a net ATP consumer in the liver, as opposed to free acid BHB and MCT which are ATP (energy) producers.[7] This sheds a whole new light on the BHB vs. Ketone Esters.
- Body mass loss[59]
- Dehydration[59]
- Decreased fertility[62]
- Delayed fetal skeletal growth[62]
- Metabolic acidosis[59]
- Stunted growth[60]
- Hepatotoxicity[60,61]
- Physical dependence[63]
- Sinusoidal dilation[59]
Unsurprisingly, 1,3-butanediol is metabolized similarly to ethanol.[64]
Even worse is the ketone ester 1,4-butanediol, which is under the Department of Justice's watch list due to its toxicity,[65] as there have been several overdoses from it -- sometimes fatal.[66-68]
Due to these concerns, we're very wary of ketone esters and prefer BHB salts or free acid BHB as safer alternatives.
BHB Dosage
The suggested amount of supplemental BHB depends on one's goals. While we'll never say no to any amount of BHB, we find that the best experience really starts at the 5 gram dose level. This is most conveniently achieved with powders (as BHB salts) and liquids (as BHB free acid).
However, even a couple of grams can provide many individuals with a quick boost. Ketone Labs allows for capsules to be formulated at 800 milligrams per serving, and gummies at 400 milligrams per serving. With that said, we'd generally try taking a couple servings daily to increase those amounts.
For those seeking sleep improvements, the 2025 sleep study discussed above utilized evening dosing of 1.5 or 2.9g, taken one hour before bedtime.[18]
Conclusion: BHB is not just for Keto Dieters, But Pick the Right One
goBHB is not just a "keto" supplement -- one of the best benefits is in fact productivity from improved mental clarity and stimulant-free energy!
As we continue to see the resurgence of exogenous BHB supplements, it's clear that these ketones aren't just for keto dieters anymore. While the early days of goBHB saw marketing aimed specifically at ketogenic enthusiasts, today, we recognize the potential benefits of BHB for a broader audience. Whether you're a high-performance athlete looking for energy and endurance, someone interested in enhancing brain function and metabolic flexibility, or someone who simply wants better sleep quality, BHB supplements offer a wide array of advantages.
One of the most exciting aspects of the BHB resurgence is its versatility. We've found that goBHB as Free Acid BHB works best in energy drinks for a quick and clean energy boost, while D-BHB salts shine in powdered supplements, especially when athletes need longer-lasting fuel. The industry has evolved, and so has our understanding of how to best utilize these ketones.
With a growing body of research supporting its benefits, from enhancing cognition to improving athletic performance, the future looks bright for BHB. We're thrilled to see how these supplements continue to evolve and support a healthier lifestyle for everyone. Stay tuned and sign up for our Ketone Labs news alerts as we explore more BHB innovations and product launches in the months to come!




Comments and Discussion (Powered by the PricePlow Forum)