This is how a legacy begins.
Alpha Prime Supps may be a relatively new supplement brand, but they're a serious one. Their energy and drive was put on display earlier in February of 2021, when Ben Kane of PricePlow flew down to Florida to see the promising young team in search of a new frontier in the supplement industry:
From racing to sports nutrition: Meet Caesar Bacarella
The story begins with Caesar Bacarella, a professional race car driver who competes in the NASCAR Xfinity Series, driving for Alpha Prime Racing. Alpha Prime runs a fantastic apparel business, but as a top-tier athlete, Caesar found himself amidst the world of sports supplements, looking for an extra edge in his health, fitness, and focus.

Are you ready for your legacy? After a year of hard work, Alpha Prime Supps has released their Legacy Series Pre-Workout and Pump Supplements
Caesar instantly fell in love with the world of supplements, and before you knew it, Alpha Prime began dabbling into supplements. Caesar's likable enthusiasm is downright infectious, and he was able to enlist Brian "Ike" Ikalina as his VP (explained in Episode #043 of the PricePlow Podcast). The duo began the Alpha Prime Supps, and with some incredibly impactful supplements, are well on their way to a new legacy.
The Alpha Prime Legacy Starts here
When it comes to the sports nutrition niche of the supplement industry, there's generally one way to begin your legacy: with an epic pre workout stack. Alpha Prime has done just that, with their new Legacy Series, which includes the Legacy Series Pre and Legacy Series Pump. Inside, we're treated to some incredibly powerful and well-dosed formulas, with a brand new innovation in the Pump formula.
A brand with drive
AP goes big on a couple of ingredients, so if you're ready to feel a sick pump and crystal clear energy, you're ready for the Legacy Series. It's all covered below -- but first check the availability on PricePlow and sign up for our Alpha Prime alerts -- we have a lot more coming from the hot upstart:
Alpha Prime Supps Legacy Series Pre-Workout – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
Alpha Prime Supps Legacy Series Pump – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
Alpha Prime Supps Legacy Series Pump – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
This area is reserved for Team PricePlow's upcoming Ingredients video.
Subscribe to our channel and sign up for notifications so you catch it when it goes live!
Between the two formulas in the Legacy launch, we've got a total of 16 excellently-dosed ingredients, so we're going to keep these write-ups succinct.
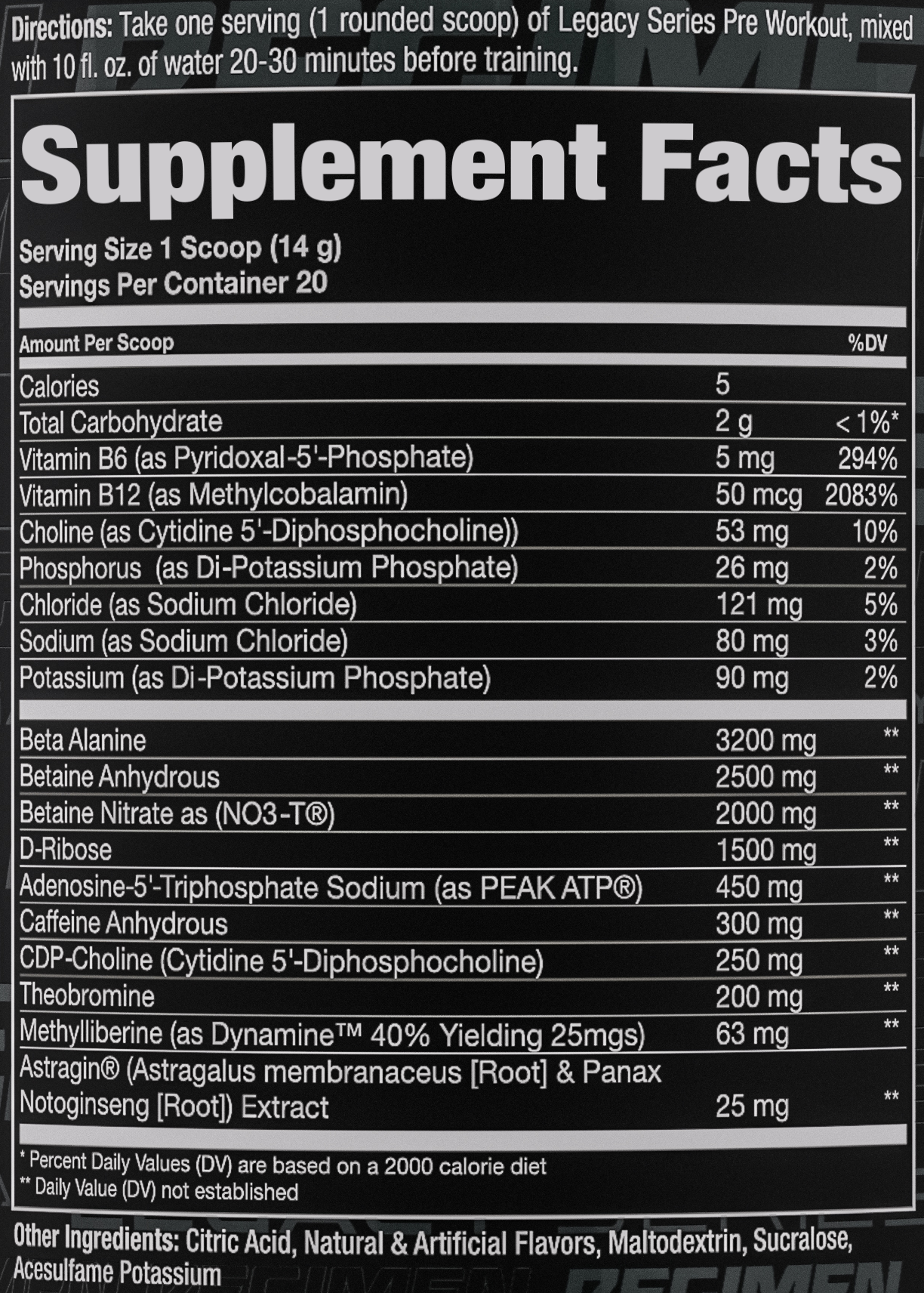
Legacy Pre Ingredients
-
Beta Alanine - 3200 mg
What better way to start a pre workout than to make it last longer with more muscular endurance?! That's exactly what beta alanine does -- this is the popular endurance-boosting (and occasional tingle-generating) amino acid that combines with L-histidine to build more carnosine.[1,2] Carnosine in turn helps muscle tissues buffer lactic acid, reducing overall fatigue.[2]
There have been numerous studies on beta alanine and its beneficial effects on endurance, so let's recap the two major meta analyses on the ingredient:
- The first 2012 meta analysis showed that beta alanine leads to endurance increases in exercises 1-4 minutes long across numerous sports and training types.[3] It looked at 15 studies that analyzed 360 separate athletes.
- The second meta analysis, published in 2016, expanded that thesis - they showed that beta alanine promoted significant endurance gains in training activities ranging from 30 seconds to 10 minutes![4] It analyzed 40 studies on 1461 athletes doing 70 different exercises.
Above, we mention the tingle factor -- this is actually known as paresthesia, and the 3.2 gram clinical dose that we have here in Legacy Pre may give you some. However, in 2019 a peer-reviewed article analyzing the safety profiles in the other beta alanine studies showed that there were no adverse effects from it.[5]
But that's not the end of our endurance. Now that we have your muscles lasting longer, let's get them hydrated, strong, and pumped:
-
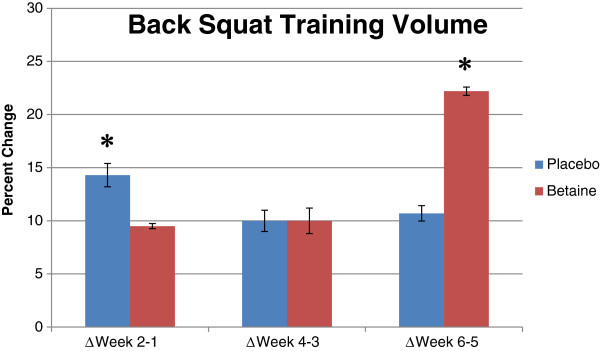
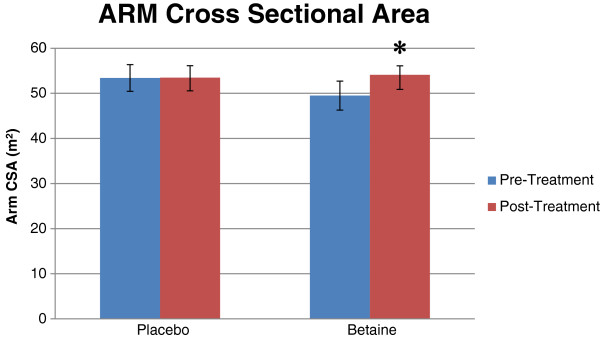
Betaine Anhydrous - 2500 mg
As you'll see, Alpha Prime bets big on betaine, the strength, size, and hydration-boosting ingredient also known as trimethylglycine. This alone is a clinical dosage, but there's plenty more to be found in the Pre/Post stack. Since it's heavily used in these two supplements, let's cover its research thoroughly and reference back to this area when needed.
The placebo effect was definitely strong with this group. But... the real gains obliterated placebo in due time![6,7]
Betaine is an osmolyte that helps with cell hydration but also acts as a methyl donor.[8,9] This means it leads to body-wide improvements, and we've seen studies supporting its use in:
- Athletic performance[10-15]
- Muscle growth[6,7]
- Fat loss[16,17]
- Heart health[9,10,18-20]
- Protection from heat shock[10,21]
In terms of pumps, make sure you drink enough water - the osmotic effects mean that betaine can increase the amount of water in cells,[8] giving that "swellular" sensation.
Good news: the muscle growth, fat loss, and some athletic performance studies cited above used this dosage -- 2.5 grams per day.[6,7,12-16]
Even better news: once we add more betaine from the rest of this formula and the rest of this stack, we may even be able to claim even more performance enhancement effects![10,11]
Finally, betaine can even help with a bit of a nitric oxide boost[20] -- but it's really here for the ergogenic and hydration properties.
As alluded to above, get ready for even more betaine:
-
Betaine Nitrate - 2000 mg
Attached to the epic betaine molecule is an even more epic molecule -- nitrate (NO3), used to form betaine nitrate. When ingested, nitrate follows the unique nitrate-nitrite-nitric oxide pathway through the salivary glands to boost nitric oxide in a big way.[22-24] Nitrates lead to incredible physical performance gains and better endurance, much of it through increased blood flow.[25,26]
Nitrate benefits
Various studies have shown that well-dosed nitrate, like we have here, can improve numerous metrics:
- Improved blood flow[25,26]
- Less oxygen needed for physical exertion / training[26-29]
- Increased strength, force, and power production[30,31]
- Significant nitric oxide boost[30,32]
- Better endurance / reduced fatigue[28,29]
- Increased overall cellular energy[31-33]
- Improved post-workout recovery[31-33]
There's also a solid meta analysis covering these benefits[25] -- various forms of nitrates have been well-researched!
Make no mistake, this is the main pump ingredient in Legacy Pre - so how much are we getting?
How much nitrate is in betaine nitrate?
Since betaine nitrate is ~35% nitrate and ~65% betaine, we'll get a fantastic 700 milligrams of nitrate along with 1300 milligrams more betaine, bringing us to roughly 3.3 grams of total betaine... and there's even more coming in the Legacy Pump supplement!
-
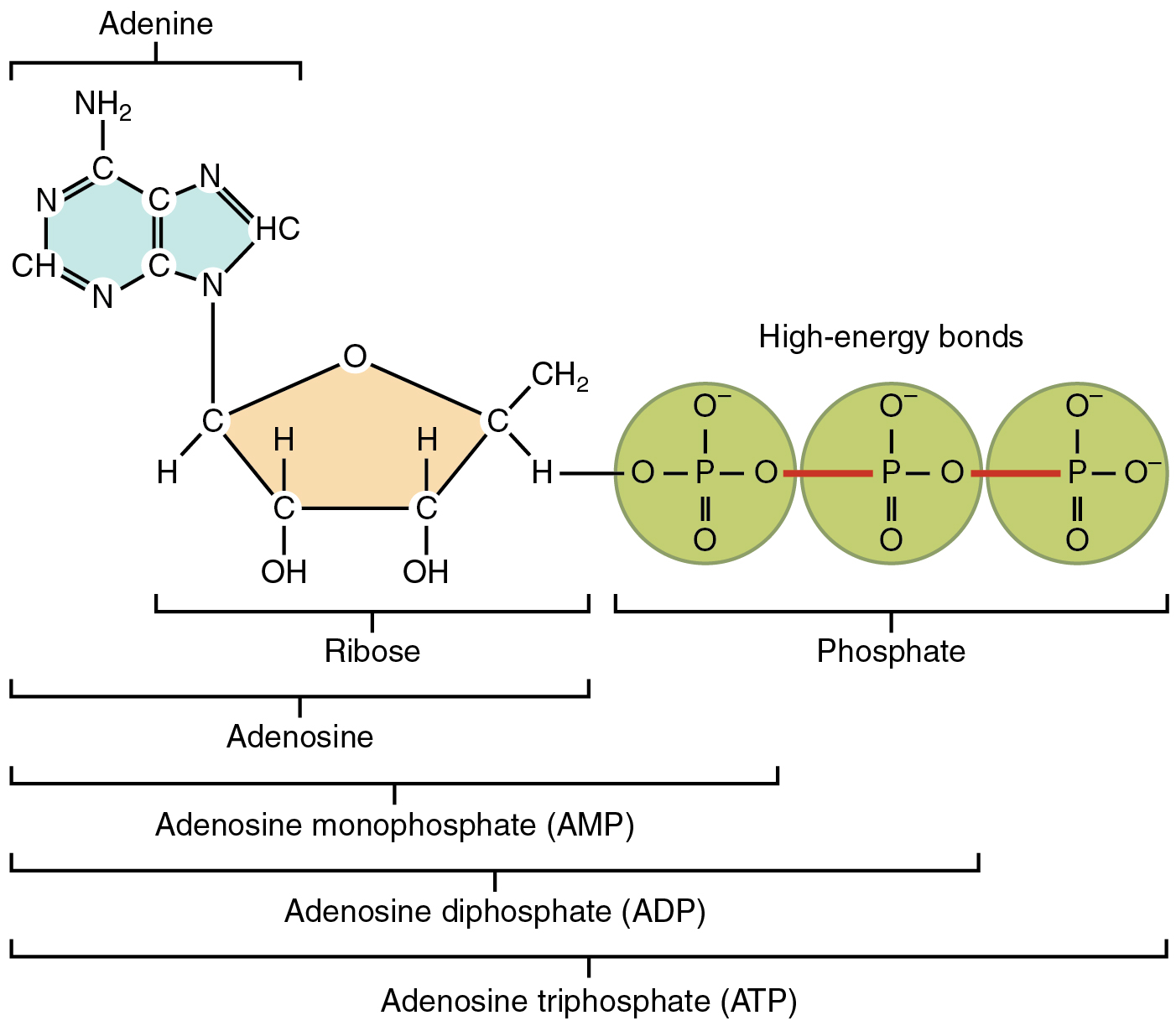
D-Ribose - 1500 mg
A great theme we'll see in Legacy Pre is how we can get cellular energy improvements -- both betaine and betaine nitrate are beneficial to our cell powerhouses, but the next two ingredients may be even better for that task.
First, let's talk about energy. Our cells don't deal in units of "calories" -- they utilize adenosine triphosphate, or ATP, to their intracellular "energy currency".[34] In general, more ATP production -- and more ATP availability for our cells -- is better for nearly everything.
One way to get more ATP? To provide the body more of its component parts. D-Ribose is a type of carbohydrate that actually composes part of the ATP molecule, alongside adenosine and phosphate. By providing additional ribose, you're ensuring that your body has the tools it needs to easily generate ATP - exactly what we need when training.
While our bodies are can make our own ribose, there are sometimes bottlenecks with some of the enzymes (such as glucose-6-phosphate dehydrogenase).[34] Just in case that's affecting you, we prefer to work around it by adding more ribose fuel to the fire. Research has shown ribose supplementation to assist with endurance, decreasing pain, cramps, and post-exercise stiffness.[35]
Have no fear if you're a low-carber - ribose has a lower impact on blood sugar than maltodextrin.[36] And if you're afraid of 1.5 grams of beneficial carbs, we're going to have to sit down and have a little talk.
Back to business, the point is that we want ATP and we want it now, and ribose keeps us away from a potential bottleneck. However, we can do even more -- by providing a form of ATP itself!
-
Adenosine-5'-Triphosphate Sodium (as PEAK ATP) - 450 mg
Since we're on the subject of ATP, Alpha Prime decided to skip the end-arounds and get straight to business by providing extracellular adenosine triphosphate from PEAK ATP. This patented ingredient is one of only exogenous ATP supplements we've seen to successfully work in research.
Once taken, PEAK ATP causes extracellular ATP levels to rise in the body, and this yields a few excellent effects like vasodilation, muscle excitability, and anabolic signaling.[37]
In 2013, researchers published a study using 400 milligrams of PEAK ATP per day, documenting that subjects had increased strength by 147% and lean mass by 100% compared to the placebo group.[37] Alpha Prime Supps actually went above that dose with 50 milligrams more!
Additional research showed that PEAK ATP can reduce fatigue during repeated high intensity exercise sets, and the study included both men and women.[38] The participants in the PEAK ATP group were generally able to keep their torque strength longer throughout exhaustive workouts.
-
Caffeine Anhydrous - 300 mg
On the note of energy, Alpha Prime Supps packs in a solid 300 milligrams of caffeine in one scoop, which should help you adjust your scoop size.
Most users know how caffeine hits them at this point -- this is a bit more than your average energy drink. It works primarily through the inhibition of adenosine and phosphodiesterase,[39] keeping you awake and alert. It also functions as a mild fat burner, since it can improve metabolic rate and boost metabolic flexibility through the liberation of fatty acids from fat tissue.[40-42] It's then up to you to use those fatty acids during your workout and burn them off!
Caffeine anhydrous is simply caffeine without water attached - it's fast acting and the type of caffeine we generally see in pre workout supplements.
-
CDP-Choline (Cytidine 5'-Diphosphocholine) - 250 mg
Focus time! In general, the body and brain love the essential nutrient choline because it strengthens cell membranes[43] and is the precursor to our "learning neurotransmitter", acetylcholine.[44] Healthy acetylcholine levels are important for overall focus and brain activity because it's heavily-involved in cognitive functions such as learning, memory formation, and attention.[45,46] By supplementing choline, we can get more acetylcholine made.
This is where CDP-choline (also known as citicoline) comes in - it's a high-bioavailability for of choline that is also quite experiential since it can boost the density of the brain's dopamine receptors.[47] In our anecdotal experience, CDP-choline is the form of choline we feel the most. It's an essential vitamin, so remember to eat your egg yolks, which are abundant in the nutrient.
-
Theobromine - 200 mg
A couple more energy-based ingredients to go in the Legacy Pre - now it's time to smooth out the caffeine strike with it's longer-lasting cousin, theobromine. Just like caffeine, it's a methylxanthine, and has similar effects in terms of inhibiting adenosine and phosphodiesterase.[48]
The difference between theobromine and caffeine is that theobromine is much more mild, but also much longer-lasting due to its longer half-life.[49] This is generally used to prevent a caffeine crash, as the theobromine keeps energy coming after caffeine begins to wear off.
Additionally, theobromine is experiential, providing better "feel" for users in one interesting study.[50]
200 milligrams is generally the highest dose we see with the ingredient lately.
-
Methylliberine (as Dynamine 40% Yielding 25mg) - 63 mg
Alpha Prime Supps Legacy Pre isn't done with energy yet - it finishes its stimulant trifecta with methylliberine, which is also trademarked as Dynamine. This neuro-activator provides a very fast-acting, feel-good cognitive boost - and is quite synergistic with caffeine in terms of cognitive performance, mental energy, and focus.
Found in tea leaves and classified as a purine alkaloid,[51] methylliberine has been shown to provide a similar energy boost to caffeine, only without the effects to the cardiovascular system.[51-54] It helps boost dopamine and norepinephrine levels while also inhibiting adenosine.[51-54]
We've been very bullish on methylliberine lately - it stacks excellently with caffeine, providing just a little extra "umph" to the workout experience.
Now it's time to boost the uptake of all of the above:
-
AstraGin (Astragalus membranaceus [Root] & Panax Notoginseng [Root]) Extract - 25 mg
Now it's time to tie it all together with a solid bioavailability boost from NuLiv Science's AstraGin. This is a patented form of astragalus and ginseng built to improve gut permeability, allowing for better absorption of other ingredients.[55]
On top of bettering gut function, AstraGin's components upregulate important mRNA transporters like SGLT1, GLUT4, and CAT1, leading to better sodium, carbohydrate, and amino acid shuttling to assist with nutrient delivery. The perfect way to tie the energy-packed Legacy Pre together.
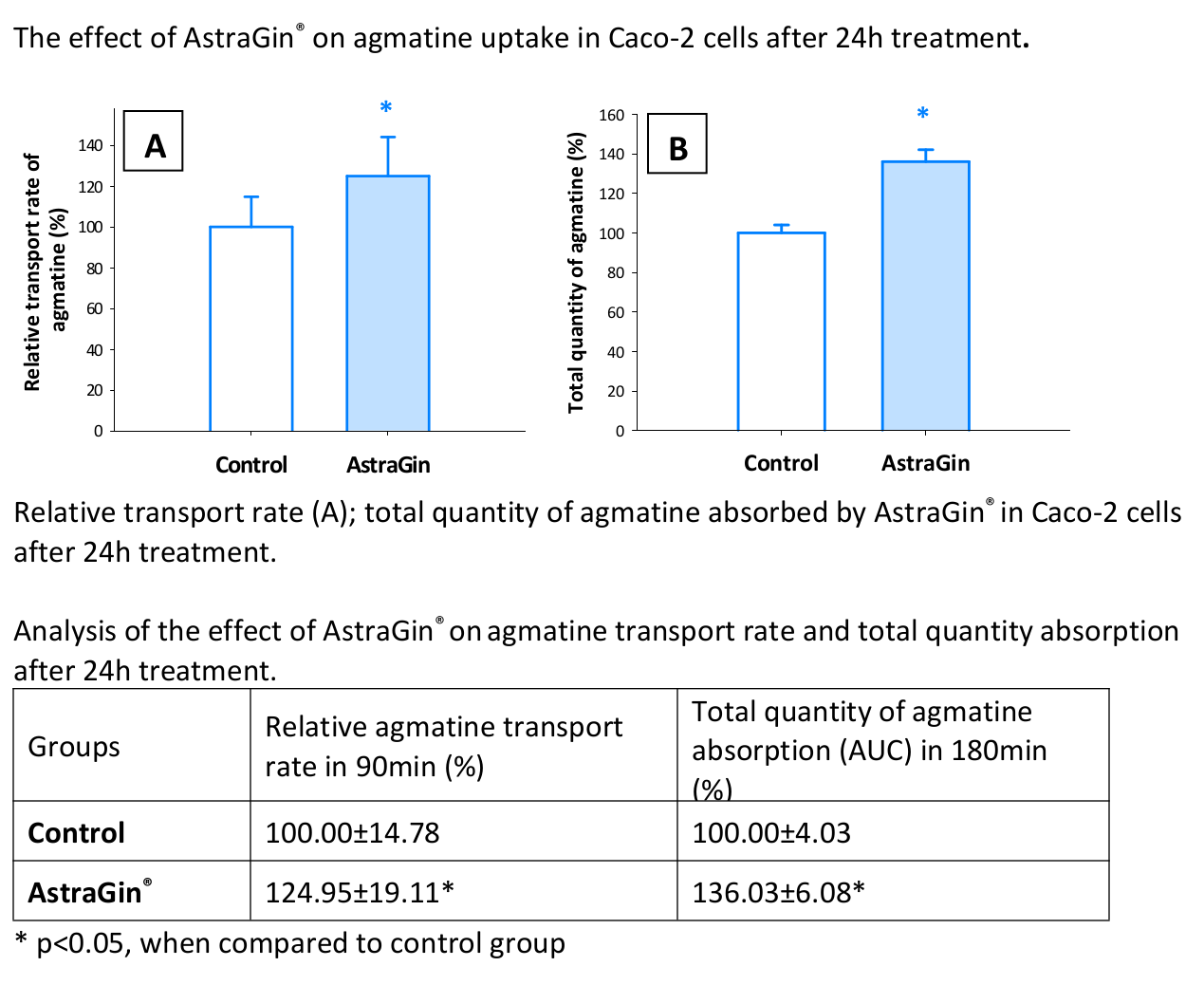
AstraGin is also in the Pump supplement, where we'll see even more ingredient synergy, with some data provided below.
Legacy Pre Flavors Available
You may notice that Legacy Pre-Workout has no citrulline. It relies heavily on the betaine / betaine nitrate blend for pumps. If you're looking for citrulline, look no further, as that's in the Legacy Pump!
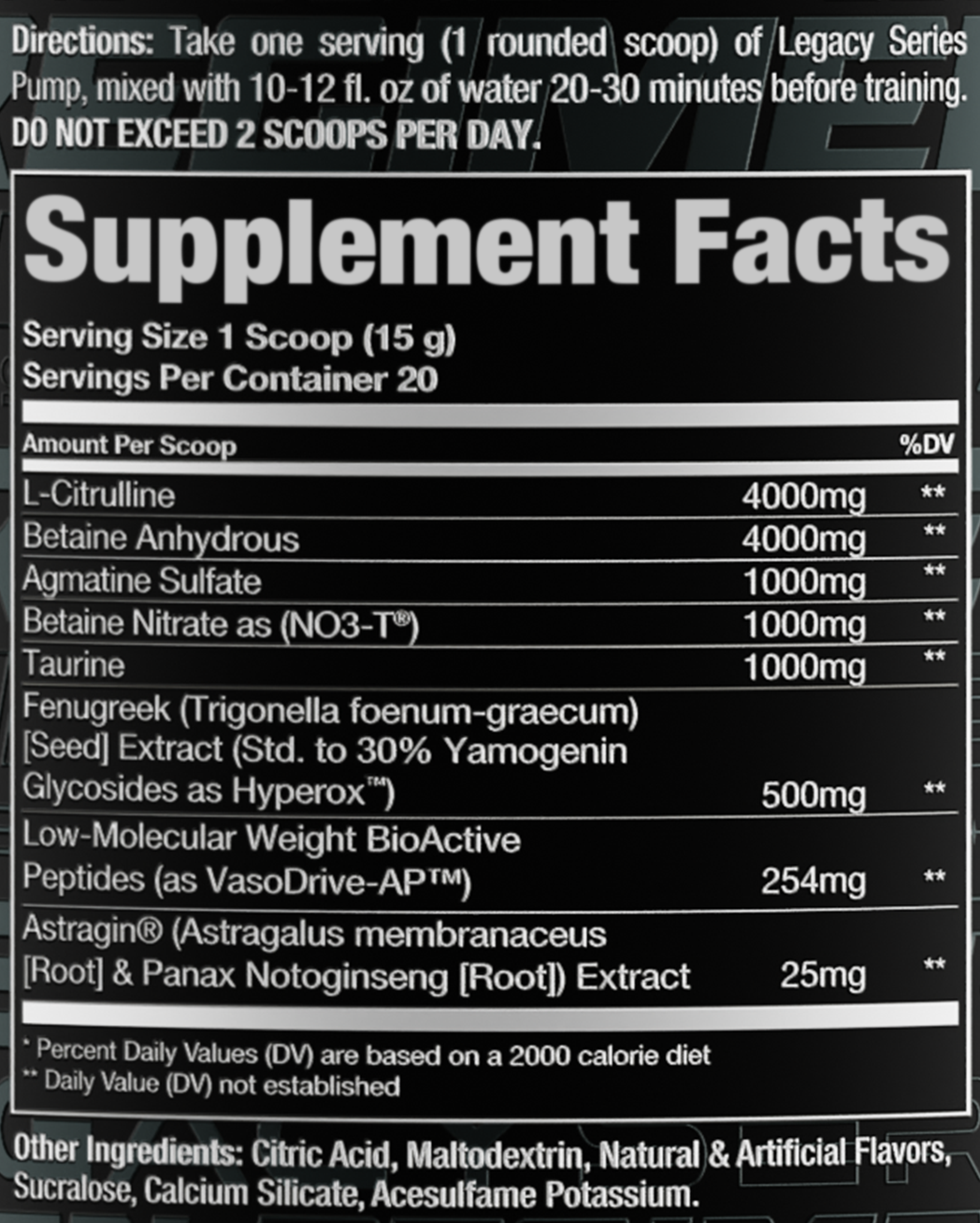
Legacy Pump Ingredients
Need more pump, or looking to go stimulant-free for a caffeine detox or evening workout? Alpha Prime Supps has you covered with their incredible Legacy Pump supplement. Here's where you get that citrulline in the stack, and even higher amounts of betaine.
-
L-Citrulline - 4000mg
Alpha Prime starts things off right with L-citrulline, the popular nitric oxide booster that is a precursor to the amino acid L-arginine, which subsequently generates more nitric oxide (NO).[56] Nitric oxide leads us to a vasodilation effect where blood vessels expand and relax, allowing for better overall blood flow.[57,58] And with that, we get pumps, as well as other great effects like improved nutrient delivery and lower blood pressure.
It may seem like citrulline takes the "long path" to nitric oxide, but it has been shown to outperform arginine supplementation for NO production in humans.[57] Reason being, if you were to supplement arginine directly, too much would get broken down in the gut before it can lead to NO gains.[59-62] Besides, high-dose arginine supplementation is awful on the gut.[63,64]
Citrulline simply does it better. And with those pumps, with get some awesome athletic benefits:[65-68]
- Greater work output
- Better recovery
- More ATP production
The clinical dose is 3 grams,[69] and as you can see, Alpha Prime Legacy Pump has more than that.
Speaking of dosing, take a look at the next ingredient:
-
Betaine Anhydrous - 4000mg
Here we have betaine again, with all the benefits we discussed above – and check the dose! A whopping 4,000 mg per serving!
As we noted in the betaine section for the pre-workout formula, most studies on the effects of betaine use a much smaller dose of about 2.5 grams per day.[6,7,12-16] Here we're increasing the clinical dose by about 50%. You are definitely going to feel it – in a good way!
-
Agmatine Sulfate - 1000mg
Whereas citrulline is an arginine precursor, agmatine sulfate is an arginine metabolite. In the arginine-citrulline cycle, agmatine sulfate works to inhibit arginase,[70] the enzyme that breaks down arginine – so agmatine sulfate basically extends the action of arginine, working synergistically with citrulline raise the levels of arginine, and hence nitric oxide in the blood.
Furthermore, agmatine has been shown to independently stimulate the production of nitric oxide synthase,[71] the enzyme responsible for synthesizing nitric oxide in endothelial cells, so agmatine is in itself working on nitric oxide production from both angles.
Intriguingly, agmatine also acts as a neurotransmitter with mood-elevating properties.[72]
-
Betaine Nitrate (as NO3-T) - 1000mg
We also covered betaine nitrate in the pre-workout section above – the thing to note here is that the dose is a little smaller, so we are getting less nitrate activity, but this is made up for in part by way more betaine from the bigger dose of betaine anhydrous.
-
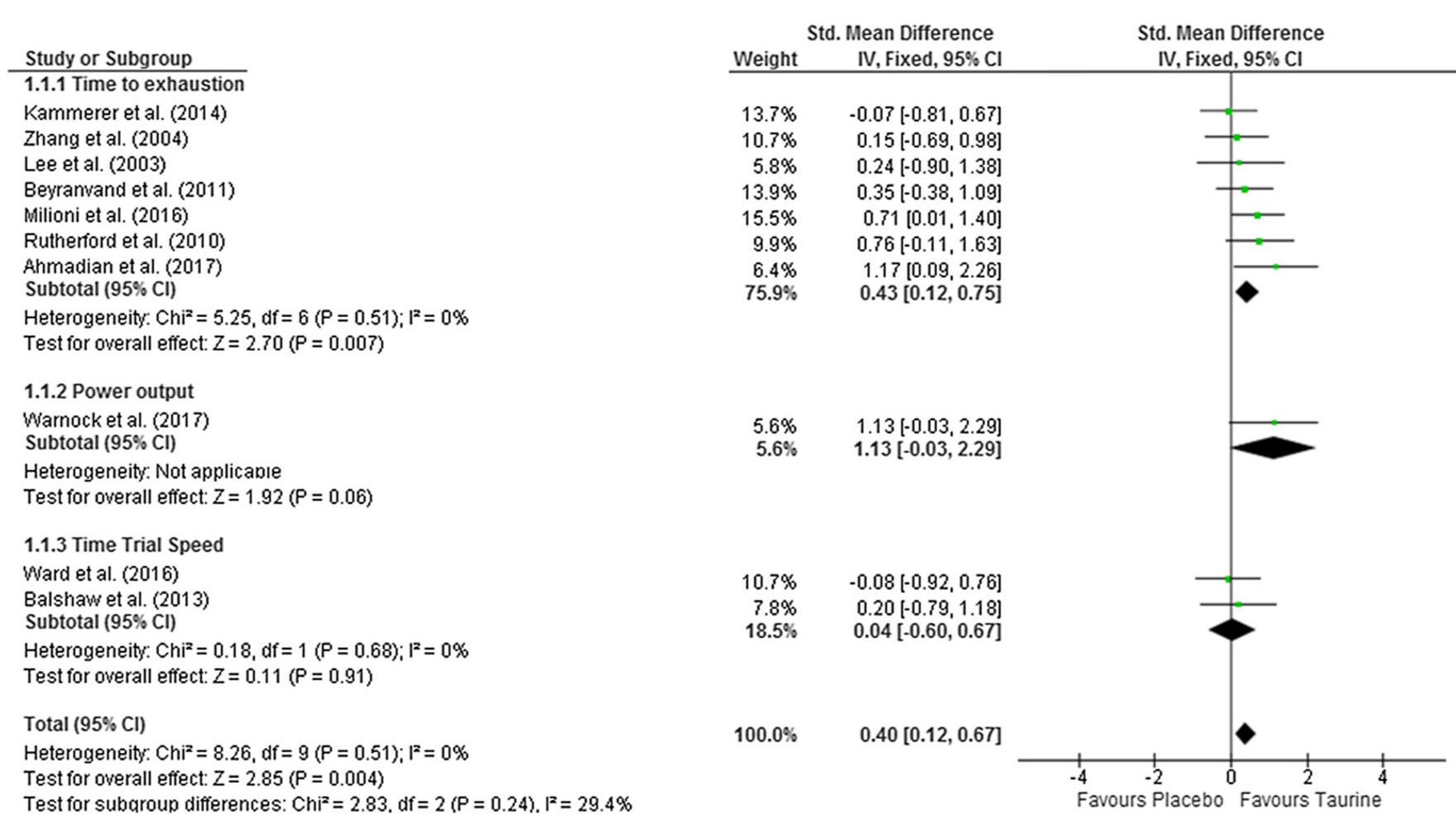
Taurine - 1000mg
With such massive nitric oxide support from this pump stack, the only major thing left for it to accomplish is maximizing cellular hydration. That's where taurine comes in – an osmolyte that promotes "osmotic swelling"[73] in mammals, thereby increasing the water content of cells, buffering mitochondria and protecting them from stress while supporting energy production.[74]
We call this a "water pump," to distinguish it from the traditional NO-mediated pumps that maximize blood flow. To get the most out of osmolytes, be sure to drink plenty of water when taking them.
Among other things, taurine has been shown to significantly increase physical endurance, as was demonstrated in a 2018 meta-analysis of ten different studies on taurine.[75] The researchers who did this meta-analysis found that a dose of anywhere from 1 to 6 grams of taurine daily significantly improved endurance.
Taurine's effects on cellular hydration have a lot to do with this, but so does its ability to combat oxidative stress by optimizing calcium signaling, which is going to facilitate muscle contractions, and supporting fat digestion.[75-78]
But interestingly, taurine goes beyond just a "water pump" and actually stimulates nitric oxide production as well.[78]
One last thing to note about taurine is that it has a significant positive effect on cognition[77] – not too surprising, considering that optimal flows of blood and water to the brain are so important for healthy brain function.
-
Fenugreek (Trigonella foenum-graecum) [Seed] Extract (Std. to 30% Yamogenin Glycosides as Hyperox) - 500mg
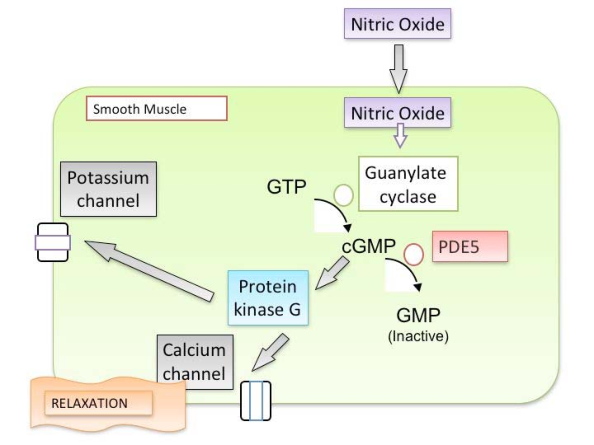
Fenugreek has a great and long-established reputation as a testosterone-boosting supplement. This extract of fenugreek, standardized for yamogenin, is intended to act as a phosphodiesterase-5 (PDE5) inhibitor.
How does this contribute to a pump, you ask?
Phosphodiesterase-5 inactives cGMP, a messenger molecule that mediates the vasodilatory effects of nitric oxide (NO). Inhibiting PDE5 potentiates the effects of NO.[79]
As shown in the diagram above, nitric oxide stimulates the production of a nucleotide called cyclic guanosine monophosphate (cGMP), which is what actually tells smooth muscle tissue to relax. In other words, cGMP is responsible for the vasodilation caused by NO.
By inhibiting cGMP, Hyperox is able to increase the vasodilatory activity of NO!
In an industry where a few heavy-hitting ingredients are used over and over again in 99% of products, it isn't often that we encounter a genuinely new ingredient. We're excited to see where Hyperox goes as AP's product line gains exposure.
-
Low-Molecular Weight BioActive Peptides (as VasoDrive-AP) - 254mg
VasoDrive-AP is a combination of two lacto-tri-peptides named isoleucyl-prolyl-proline (IPP) and valyl-prolyl-proline (VPP). Each one is a combination of three amino acids, sourced from casein, a protein complex that occurs naturally in milk.
These two compounds work to inhibit the angiotensin converting enzyme (ACE),[80,81] an enzyme that causes vasoconstriction.[82] When ACE is inhibited, vasoconstriction is substantially reversed, allowing for increased vasodilation,[83] which is what we're going for with any pump stack.
There are over 30 studies on these two lacto-tri-peptides, as reviewed in the peer-reviewed 2015 meta-analysis "Casein-Derived Lactotripeptides Reduce Systolic and Diastolic Blood Pressure in a Meta-Analysis of Randomised Clinical Trials."[80]
So once again we can see how AP is attacking the vasodilation problem from multiple angles – not just the NO pathway.
-
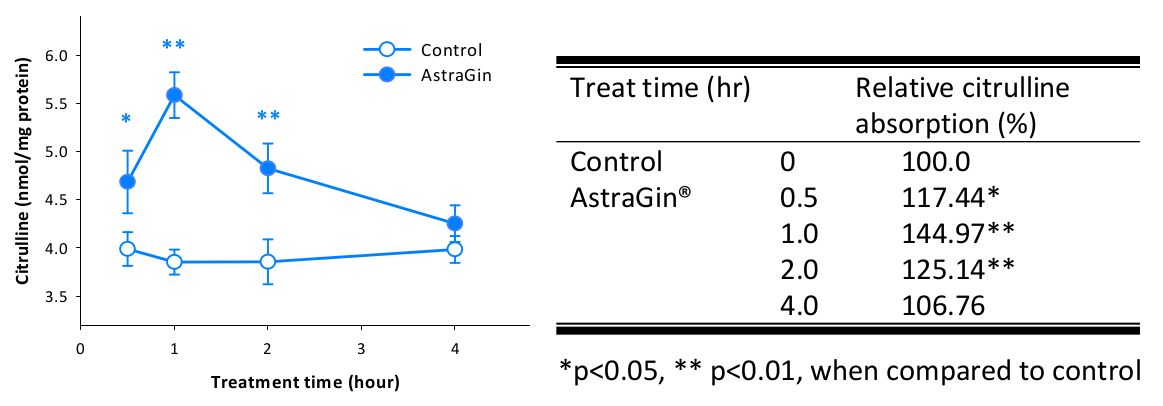
AstraGin (Astragalus membranaceus [Root] & Panax Notoginseng [Root]) Extract - 25 mg
AstraGin is a combination of Astragalus and Panax Notoginseng that's been shown to increase ingredient absorption, especially of amino acids!
One excellent trend we're seeing in the industry today is this increasing use of ingredient-enhancing ingredients that improve the absorption and bioavailability of other ingredients. Examples of this category would be BioPerine, an extract of black pepper fruits, and AstraGin, a blend of botanical extracts from the Astragalus and Panax genuses.
AstraGin works by activating certain transporters that move nutrients out of the gut and into the bloodstream – increasing gut permeability.[84]
The choice of AstraGin for this formula is particularly smart, because AstraGin has been studied specifically for its ability to increase the absorption of agmatine and citrulline – two ingredients that are present in Alpha Prime Supps Pump!
AstraGin enhances citrulline absorption[84] – note that citrulline concentrations peak at one hour, which is the middle of your workout if you take AstraGin and citrulline at the beginning of it.
So, pretty straightforward – AP is helping you get the best bang for your buck by including AstraGin, which will significantly improve the bioavailability of the citrulline and the agmatine in Alpha Prime Supps Pump.
Legacy Pump Flavors Available
Are you ready for a new legacy?
There's no doubt about it - Caesar, Ike, and the team at Alpha Prime have put together an insanely aesthetic brand and look - with formulas to follow. The same goes for their social media presence, which can now be found at @apregimen to follow the incredible apparel and products at @alphaprime.
Earlier in 2021, Ike told us that this brand was coming in a big way -- and he was absolutely right. Take a look at our vlog to see how much pride, energy, and excitement they're putting into their efforts. It's all made possible because there's simply something special about Caesar.
The Legacy Series Pre and Pump stack is quite the stamp for a young brand to put on the industry. If you're ready to start your next journey, take a look at Alpha Prime Supps and actualize it into your legacy.
Alpha Prime Supps Legacy Series Pre-Workout – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
Alpha Prime Supps Legacy Series Pump – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.











Comments and Discussion (Powered by the PricePlow Forum)