Next to immunity, gut health is one of the most sought-after health supplement categories this decade. Revive MD, a booming brand born out of the sports nutrition sector that's overtaken the general health category, has released Revive MD GI+ in true Revive fashion.
This wisely-formulated supplement provides several unique ingredients to give users several types of protection for the gastrointestinal tracts. GI+ was created to protect GI health for both Revive MD's athlete's and non-athletic users looking for a powerful gut health supplement that you just can't get in a capsule formula. As a powdered formulation, you achieve higher doses and can get more prebiotic and probiotic fiber inside.
Revive MD, a supplement brand that's no stranger to all-in-one formulas, has put out their comprehensive GI Health supplement, GI+
GI+: A multi-faceted Gut Health Supplement
GI+ is built for the following benefits:
- Support gut lining integrity
- Protect the gastric mucosa and gut environment
- Promote healthy gut bacteria growth, and
- Boost GI immune function
If you've followed our other Revive MD articles, you'll know that they're in-depth because the supplements are in-depth, with several ingredients working together to achieve their goals. This one's not much different, and it starts off with a bang with a different form of glucosamine (N-acetyl-glucosamine) that we don't see often enough.
We dig into the analysis below, bringing dozens of citations to support the supplement, but first see the prices and our PricePlow-powered coupons:
Revive MD GI+ – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
This area is reserved for Team PricePlow's upcoming Ingredients video.
Subscribe to our channel and sign up for notifications so you catch it when it goes live!
Revive MD GI+ Ingredients
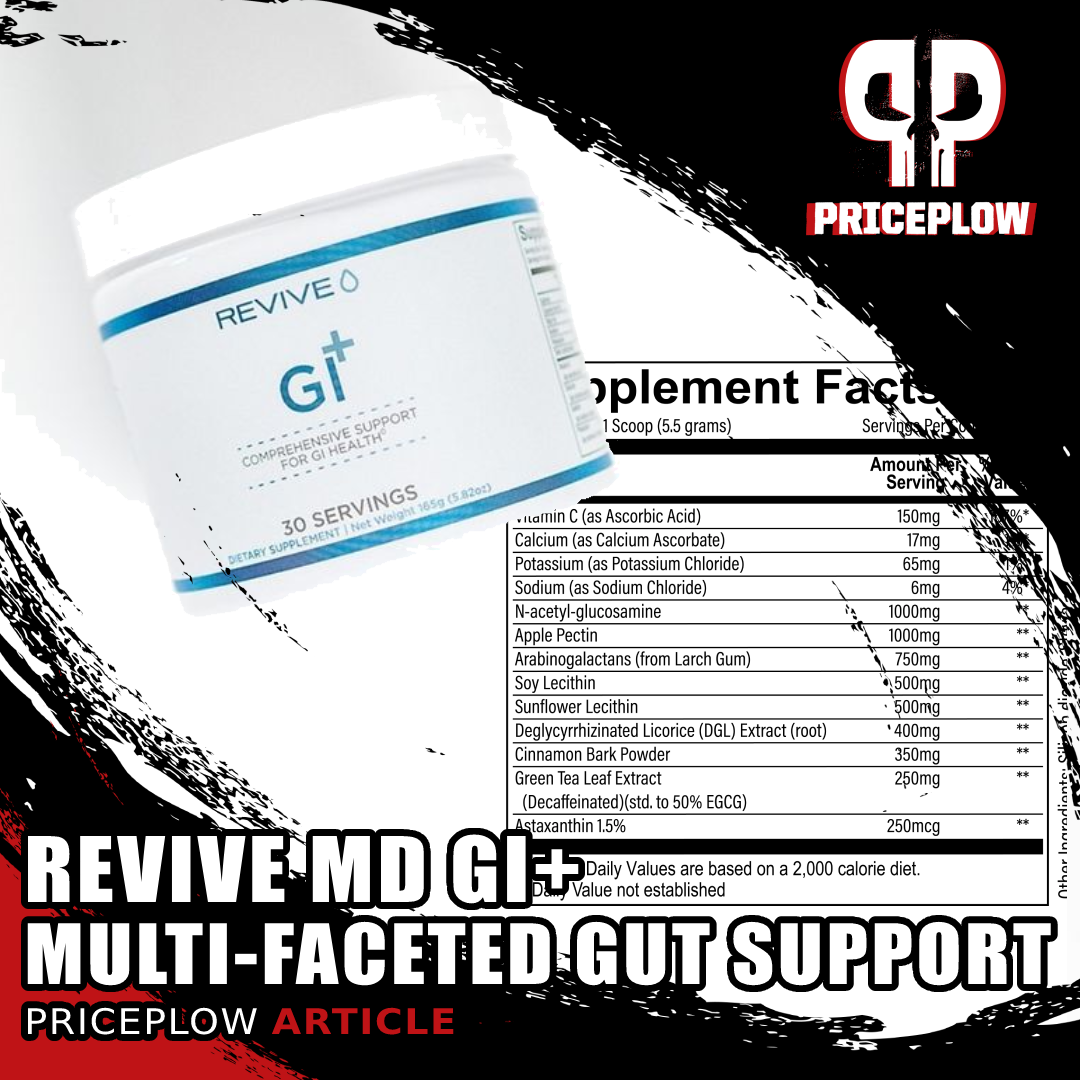
Every 5.5 gram scoop of GI+ provides you with the following ingredients:
-
N-acetyl-glucosamine - 1000mg
Sometimes, you just have too many ingredients to do it in a capsule. At 5.5g dosage, it has to be in a powder!
We often see glucosamine in joint supplements, where it's well-known to provide minor overall pain reduction and joint support (as demonstrated in several studies and meta-analyses on knee osteoarthritis).[1,2] On top of an impressive 2020 analysis connecting glucosamine supplementation with longer lifespan / lower all-cause mortality,[3] we're extremely confident that glucosamine is healthy and beneficial. But why is it in a gut health supplement, and why N-acetyl-glucosamine?
Collagen is largely composed of N-acetyl-glucosamine, both in the chains of keratin and hyaluronic acid.[4] In 1977, researchers published an article in Gut connecting glucosamine synthetase -- the primary enzyme in the synthesis of intestinal mucosa glycoproteins -- to Crohn's disease severity.[5] What they saw was that glucosamine synthetase was lower in Crohn's disease patients' colon mucosa compared to healthy individuals, but patients who were recovering more quickly had more elevated levels of the enzyme.
So in 1983, researchers published an article in The American Journal of Gastroenterology comparing uptake of N-acetyl glucosamine in intestinal mucosa for patients with IBS (inflammatory bowel disease).[6] They recruited 9 subjects with Crohn's disease, 9 with ulcerative colitis, and 26 healthy controls.
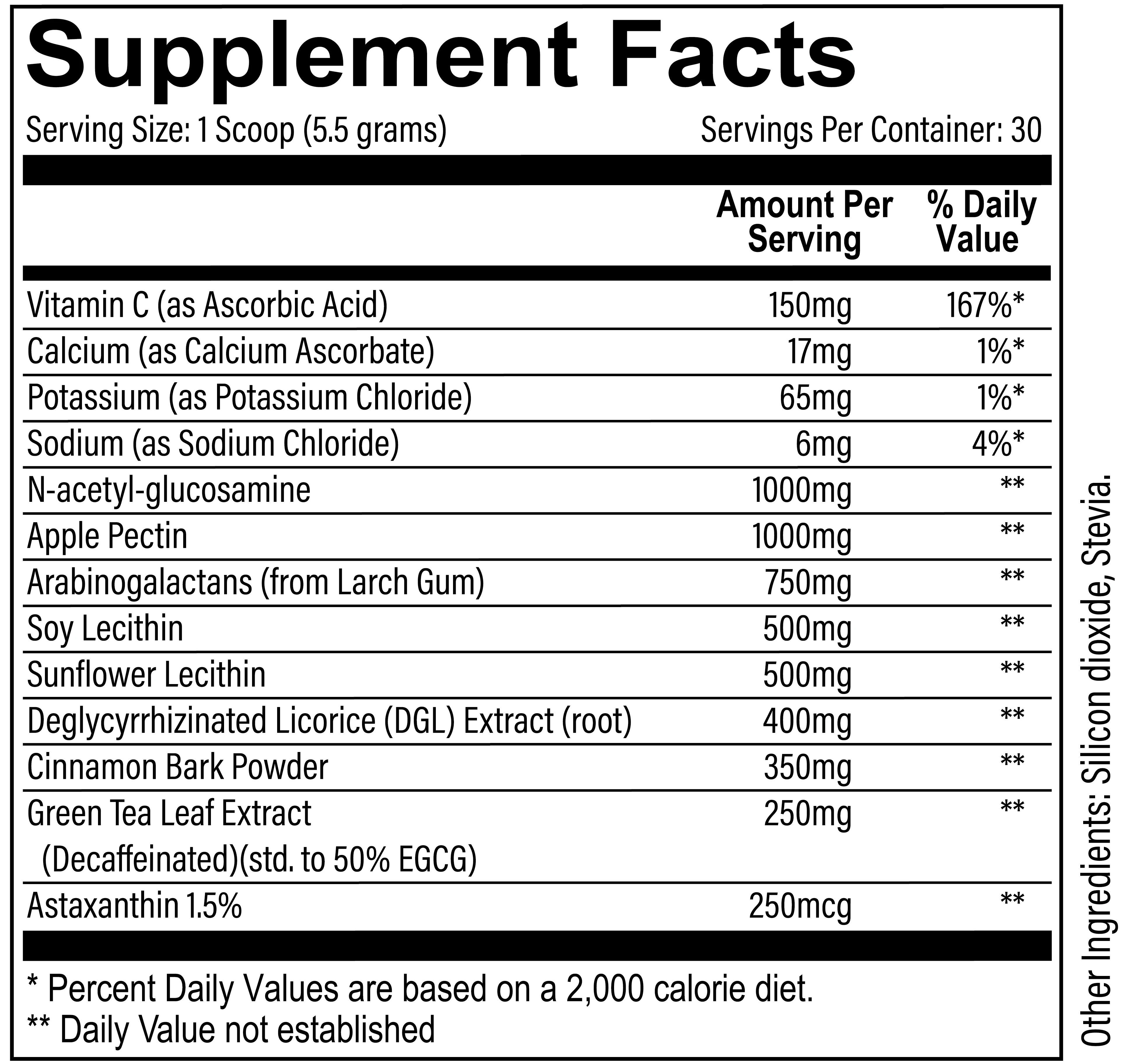
Simplified summary of the central role of N-acetylglucosamine (GlcNAc) in the metabolism of the amino sugars.[7]
Upon incubating soft intestinal mucosa tissues in glucosamine and N-acetyl-glucosamine (written as GlcNAc in many studies), they found that Crohn's patients had a tougher time converting glucosamine to N-acetyl-glucosamine due to acetylation issues. This showed that N-acetyl-glucosamine is far more effective for individuals with gut health problems.[6]
This brings us to the most commonly cited study on N-acetyl-glucosamine in Crohn's patients, a 2000 pilot study published in Alimentary Pharmacology and Therapeutics.[7] Here, researchers recruited 12 children with severe inflammatory bowel diseases (10 with Crohn's disease, 2 with ulcerative colitis) that were not responding to other normally-effective treatments. The goal was to see if N-acetyl-glucosamine could be absorbed and help repair tissues in the GI mucosa.
The children were given 3-6 grams of N-acetyl-glucosamine orally (taken 3 times daily). Of the 12, eight recovered and needed no further intervention![7]
Ultimately, despite having lower overall glucosamine absorption than glucosamine sulfate (which is better for joint issues), N-acetyl-glucosamine works better for gut issues, as it's what's directly used for tissue regeneration and unhealthy guts have trouble converting other forms of glucosamine to it.
-
Apple Pectin - 1000mg
Apple Pectin is a prebiotic dietary fiber, which is "a non-digestible compound that, through its metabolization by microorganisms in the gut, modulates the composition and/or activity of the gut microbiota, thus conferring a beneficial physiologic effect on the host."[8]
A review published in Current Developments in Nutrition discovered that adequate prebiotic fiber intake is associated with several benefits:
- Increases amount of good bacteria in the gut, including bifidobacteria and lactobacilli
- Improves calcium absorption
- Enhances beneficial metabolite production
- Improves immune system status
- Provides positive effects on gut barrier permeability
- Decreases the risk of allergies
- Decreases protein fermentation[9]
A prebiotic fiber assisting with stool normalization
Pectin works by forming a gel when combined with water,[10] and this can normalize stool.[11] Studies have shown that high-dosed pectin can reduce both diarrhea and constipation,[12,13] acting as a prebiotic and stimulating gut bifidobacteria in patients with IBS, effectively alleviating symptoms.
It may also alleviate symptoms of GERD (gastroesophageal reflux disease), although that was shown in subjects requiring tube feeding.[14]
A large double-blinded, placebo-controlled study on 255 children with acute diarrhea showed that 320mg apple pectin combined with chamomile improved symptoms significantly better than placebo.[15] However, the chamomile is a confound for our purposes with GI Plus, although researchers largely attribute the effects to the pectin, not the chamomile.
As an added benefit, pectin increases satiety and may suppress appetite,[16] which will please dieters. There are other benefits such as lipid improvements that can be researched, but aren't relevant to this supplement.
-
Arabinogalactans (from Larch Gum) - 750mg
Arabinogalactan is found naturally in larch trees and is a complex carbohydrate that works as a dietary fiber and can stimulate the immune system and fight viral and bacterial infections. It is made of long chains of two sugars, arabinose and galactose, hence its name.[18]
Butyrate generation and anti-ulcer effects
When ingested, arabinogalactan makes its way to the colon, where bacteria slowly ferments it into short-chain fatty acids such as butyrate. Butyrate is incredibly healthy for colon and gut health, and is an energy source for the cells in the colon.[17,19]
Animal studies have shown that plants that are high in arabinogalactan can reduce stomach ulcers.[20-22] In vitro, proteins bound to arabinogalactan have been shown to block H. pylori -- an inflammatory bacteria that may cause ulcers -- from attaching to stomach cells.[23]
-
Soy Lecithin - 500mg; Sunflower Lecithin - 500mg
Both soy lecithin and sunflower lecithin above are used to improve delivery nutrients, specifically those that are hydrophobic ("water fearing") and fat soluble. When used as "liposomes", these ingredients improve dispersion in intestinal fluids.[24] This ultimately enables more nutrients to be carried in via an increase in intestinal bioavailability,[25] but this doesn't apply to all foods nor all ingredients.
We consider the lecithin combination here as not just a way to increase absorption of the ingredients in GI Plus, but as a way to increase overall dietary absorption throughout the rest of the day.
-
Deglycyrrhizinated Licorice (DGL) Extract (root) - 400mg
Licorice comes from Glycyrrhiza plants, and have long been used for digestive health problems. However, its main constituent, glycyrrhizin, can reliably increase cortisol[26,27] and lower testosterone,[28,29] something we definitely don't want!
The latest part of the incredible Revive MD gut supplement stack, Gut Health+ helps to limit harmful bacterial overgrowth in just two capsules!
Commonly known as DGL, Deglycyrrhizinated Licorice, is created when the licorice has been had its glycyrrhizin and 18β-hydroxyglycyrrhizic acid removed, alleviating the above concerns, but keeping many of the benefits for gut health.
With the glycyrrhizin removed, we hope to get some of the benefits of standard licorice supplementation -- such as improved digestion / reduced nausea,[30] improved elimination of H. pylori,[31] and fewer ulcers[32] -- without the side effects.
DGL has had success in studies on subjects with ulcers,[33] is protective against aspirin-induced mucosal damage in mice,[34,35] and has been shown to stimulate more mucus formation and secretion.[36]
In general, DGL seems to work best in providing support against ulcers. It stimulates defense mechanisms to help prevent ulcer formation while supporting mucous membrane healing.[37]
DGL stimulates the normal defense mechanisms that prevent ulcer formation and stimulate healing of the damaged mucous membranes. DGL provides the following benefits:[36-38]
-
Improved blood supply to damaged mucosa
- Increased number of mucus-producing cells to protect mucous membranes
- Greater overall mucus production
- Intestinal cell life span[36-38]
There are other antiviral, anti-inflammatory benefits as well, but in terms of gut health, we're generally seeing support against ulcers by way of mucus barrier protection and generation with DGL.
-
-
Cinnamon Bark Powder - 350mg
We generally write about cinnamon in terms of blood sugar and insulin support, but it's also traditionally been used for gut health!
A study published in 2016 demonstrated that feeding pigs at room temperature increases carbon dioxide gas in the stomach. However, adding cinnamon reduces gastric acid and pepsin secretion from stomach walls, ultimately "cooling" the stomach.[39]
In addition, the cinnamon provides a bit of flavor to GI Plus.
If you've ever experienced a "hot" case of heartburn or gut inflammation, cinnamon could be a great ingredient to look at.
-
Green Tea Leaf Extract (Decaffeinated)(std. to 50% EGCG) - 250mg
Green Tea offers multiple powerful catechins, including EGCG. Turns out, they do far more than just help with fat oxidation
Green Tea Extract is quite a catch-all in the supplement world, with benefits ranging from fat oxidation to immunity to lipid improvements. But what about gut health?
There are a few studies that show what green tea can do for the gut:
A 2019 study at The Ohio State University showed that green tea consumption improves healthy bacteria in the intestines.[40] This may assist in reducing intestinal wall permeability, assisting with leaky gut issues.
Other studies have shown that green tea may improve the overall digestive process,[41] which may be elucidated by the mechanism shown above - healthy bacteria improvements.
Interestingly, green tea has some components that may fight food allergies by suppressing Th2 immune cells that are often responsible for immune responses to certain foods.[42]
-
Astaxanthin 1.5% - 250mcg
Astaxanthin is the red pigment in salmon and other seafood that provides several health benefits related to the reduction of oxidative stress. Astaxanthin boosts pathways that help regulate autophagy (the clearance and removal of old cells and dysfunctional units) -- it helps boost gut mucosal lining health by keeping cells young and fresh.
Astaxanthin has been shown to support sIgA,[43,44] which is secretory immunoglobulin A, a primary immune compound found in the gut mucosa.
A placebo-controlled 2008 study showed that the pigment could significantly reduce heartburn.[45] It functioned best against subjects infected with high amounts of H. pylori, the bacterium responsible for causing stomach ulcers.
Overall, we're seeing several ingredients in GI Plus that are effective against this bacteria, and it should be promising for anyone that has trouble fighting it.
-
Vitamins and Minerals Added
Vitamin C (as Ascorbic Acid) - 150mg (167% DV)
Calcium (as Calcium Ascorbate) - 17mg (1% DV)
Potassium (as Potassium Chloride) - 65mg (1% DV)
Sodium (as Sodium Chloride) - 6mg (4% DV)
It's always great to see a bit of electrolyte and mineral balance added to the supplement, and the salt (sodium chloride) is likely added for some flavor support.
Revive MD's Zinc is out, and it brings 50mg elemental zinc from OptiZinc (zinc monomethionine).
The most prominently dosed ingredient of the added vitamins and minerals is Vitamin C, which most users know for its general antioxidant and anti-inflammatory properties. A 2019 review published in Redox Biology stated that greater vitamin C intake can restore gut-liver functions as well as antioxidant status.[46]
In that review, the researchers make the connection between metabolic syndrome and gut function impairment, which depletes vitamin C and in turn impairs vitamin E trafficking.[46] Supplemental vitamin C intake can restore some function, although it's of course best to remove gut-destroying ingredients such as omega-6 polyunsaturated fatty acids from seed oils / "vegetable oils" from the diet in the first place.
Dosage and Timing
Revive MD's website states to mix GI+ with water or the beverage of your choice, and you can take it with or without food. One scoop a day is all that's needed.
If on a diet, it may make sense to take it before meals, as the fiber can have an added benefit of satiety, causing you to eat less in general.
Flavors?
At the time of publishing, there's only an unflavored version, but the area below will be updated if any flavored GI+ variations come out:
GI Plus: Revive MD Makes a Different Kind of Gut Health Supplement

GI+ stacks great with Revive MD Daily Greens!
Given the ultra-processing that takes place lately, the deterioration in quality of our foods has led to all kinds of gut problems that weren't too common just generations ago. We always plead with users to permanently remove processed foods -- especially those high in inflammatory omega-6 polyunsaturated fatty acids from seed oils like soybean oil -- from their diet.
But while these "anti-nutrients" are literally everywhere in our processed food supplies, we continue to have growing gut and bowel problems. As a response, there are several gut health supplements that have made it to the market.
GI Plus is the latest in this category of gut health supplements, and in true Revive MD fashion, they throw a lot of unique ingredients at the problem. Some ingredients that we've never used before, and others that are different variations of common ones, such as N-acetyl-glucosamine, which looks incredibly promising.
If digestion, stomach comfort, gut health, and bowel movements aren't your strong suits, GI+ is a supplement worth trying before anything else, because life's less fun when you can't be confident in your digestive system.
Revive MD GI+ – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.








Comments and Discussion (Powered by the PricePlow Forum)