More iron won't fix deficiency when inflammation blocks absorption. Lactoferrin supports iron homeostasis by reducing inflammation and restoring balance.
You're exhausted. Your iron levels aren't as high as they should be. The multivitamin sitting in your cabinet promises 100% of your daily iron needs, maybe more, and you take it religiously. Yet the fatigue persists, and if you add even more iron, you end up dealing with constipation and nausea on top of everything else.
Welcome to the iron paradox, where the well-intentioned solution of health practitioners and the supplement industry keep millions trapped in a cycle of increasing doses, diminishing returns, and mounting side effects.
The fundamental problem isn't the quality of iron supplements or even the dose. It's the entire framework: treating iron status as a simple input-output equation when human biology operates on entirely different principles. Standard iron supplements like ferrous sulfate can actually worsen inflammation through oxidative stress, potentially elevating the very hormone that blocks iron absorption and creating a counterproductive cycle.
More Isn’t Always More: An Honest Discussion on Iron
Iron status depends on a complex network of factors: hormones like estrogen and testosterone that influence iron regulation, storage and transport proteins like transferrin and ferritin, cofactors like vitamin C that affect absorption, gastric acid levels that determine iron solubility, and physiological states like pregnancy, menopause, and endurance training that dramatically alter iron needs and utilization. The body coordinates all these variables through sophisticated feedback loops, not simple addition.
As such, proper iron supplementation and maintenance isn't about adding more metal to your system. It's about supporting the body's sophisticated regulatory mechanisms -- that involve hormones, cytokines, transport proteins and more -- that determine where iron goes, when it's absorbed, and how it's utilized. Getting this wrong doesn't just waste money. It can worsen the very problems it's meant to solve.
The good news? There's a smarter approach grounded in how iron homeostasis actually works. It involves lactoferrin, the iron-binding glycoprotein found in human milk and throughout the body. And recent breakthroughs in precision fermentation technology have made human-identical lactoferrin commercially available for the first time with Helaina's effera®, offering a fundamentally different strategy for supporting iron status.
Biology Over Buzzwords: Exploring a Better Way to Correct Iron Issues
But to understand why this matters, we need to understand how the body actually manages iron. This article details the story behind iron homeostasis, and how we can better support this critical system. Before diving in, sign up for our Helaina and effera news alerts so that you're notified on new studies and announcements.
Subscribe to PricePlow's Newsletter and Alerts on These Topics
Iron Homeostasis: The Body’s Master Regulatory System
What Is Homeostasis?
Homeostasis is the process by which biological systems maintain stability through constant adjustment. Your body doesn't maximize blood sugar or body temperature. It regulates them within tight ranges through feedback loops that sense deviations and trigger corrective responses.
Iron operates the same way. The body maintains iron balance through dynamic regulation of absorption, storage, and distribution. When iron is needed for red blood cell production, absorption increases and stored iron mobilizes. When iron is sufficient or inflammation is present, absorption decreases and iron gets sequestered away from circulation.
This is fundamental physiology, and it's controlled by a hormone most people have never heard of:
Hepcidin: The Master Regulator
Discovered just over two decades ago, hepcidin is the central regulator of systemic iron homeostasis.[1] This small peptide hormone, produced primarily by the liver, controls iron levels throughout the body by regulating ferroportin, the only known cellular iron exporter.
Here's how it works: Ferroportin sits on the surface of cells that release iron into the bloodstream, primarily intestinal cells (which absorb dietary iron), macrophages (which recycle iron from old red blood cells), and liver cells (which store iron). When hepcidin binds to ferroportin, it triggers ferroportin's internalization and degradation.[1] But without ferroportin on the cell surface, iron cannot exit these cells and enter circulation. Iron becomes trapped.
This mechanism gives hepcidin extraordinary power over iron availability. Increase hepcidin production, and iron absorption plummets while stored iron gets locked away. Decrease hepcidin, and absorption increases while stores mobilize. The liver adjusts hepcidin levels based on signals about the body's iron status and needs.

Helaina's effera™ is revolutionizing supplements with the first human-equivalent lactoferrin. Research shows better bioavailability and reduced immune response compared to bovine sources.
The Inflammation Connection
Hepcidin doesn't respond only to iron levels. It also responds powerfully to inflammation, and this connection creates major problems for iron status.
When inflammatory cytokines like IL-6 rise, they trigger hepcidin production through the STAT3 signaling pathway.[2] Elevated hepcidin then blocks ferroportin, restricting iron availability even when the body has adequate stores. This creates the "anemia of inflammation", a condition where iron becomes functionally unavailable despite normal or even elevated total body iron.[3]
From an evolutionary perspective, this makes sense. Iron is essential for bacterial growth, so the body restricts its availability during infection to create a hostile environment for pathogens. Iron-binding proteins like transferrin in blood and lactoferrin at mucosal surfaces act as a defense system, sequestering free iron so bacteria cannot access it.
But chronic low-grade inflammation, increasingly common in modern populations, means many people live with persistently elevated hepcidin. Their iron stores are locked away, inaccessible despite being physically present. This creates a vicious cycle: excess iron generates reactive oxygen species and drives inflammation through oxidative stress, which further elevates hepcidin and worsens iron restriction. The "add more iron" approach can literally fuel the problem it's trying to solve!
effera™ human-identical lactoferrin demonstrates no alloimmune response in groundbreaking clinical trial, while bovine lactoferrin triggered antibody responses in over 50% of participants. First study to definitively answer the alloimmunization question for precision-fermented proteins.
This is why simply adding more iron often fails, and can even worsen the situation. If hepcidin is elevated, adding iron doesn't solve the underlying regulatory dysfunction. The new iron either gets absorbed poorly (because hepcidin blocks intestinal ferroportin) or gets trapped in storage cells (because hepcidin blocks macrophage and liver ferroportin). Unabsorbed iron sitting in the gut feeds pathogenic bacteria and generates additional oxidative stress, further driving the inflammation that elevated hepcidin in the first place.
More is not more. You can't override iron dysfunction with brute force. You have to work with it. Thankfully, we have additional tools to support a better strategy.
The Meta-Analysis That Changed Everything
In January 2022, researchers from China Agricultural University published a comprehensive meta-analysis that would fundamentally challenge conventional thinking about iron supplementation.[4]
Setting Up the Paradox
The study pooled data from 11 clinical trials comparing lactoferrin supplementation against ferrous sulfate, the standard iron supplement, in populations with iron deficiency or iron-deficiency anemia. Ferrous sulfate provides substantial elemental iron in a highly absorbable form. Lactoferrin, by contrast, is an iron-binding protein that contains relatively little iron per dose. It's perhaps better explained as an "air traffic controller" by Anthony Clark in Episode #180 of the PricePlow Podcast.

Dan DeMarino and Anthony Clark from Helaina dive deep into precision fermentation technology and effera™ human-equivalent lactoferrin, revealing how 5-week development cycles and machine learning models are revolutionizing bioactive protein production on Episode #180 of the PricePlow Podcast.
Standard assumptions would predict ferrous sulfate to deliver superior outcomes. More iron content, higher absorption, better results, right? The data revealed something entirely different.
The Clinical Outcomes: Lactoferrin Resoundly Wins
Across multiple markers of iron status, lactoferrin supplementation produced significantly better outcomes than ferrous sulfate:[4]
- Serum iron increased by an additional 41.44 µg/dL compared to ferrous sulfate (p < 0.00001). This represented a clinically meaningful difference in circulating iron availability.
- Serum ferritin, the primary marker of iron stores, increased by an additional 13.60 ng/mL (p = 0.003). Lactoferrin not only improved immediate iron availability but also built reserves more effectively.
- Hemoglobin, the iron-containing protein in red blood cells and the ultimate functional endpoint, increased by an additional 11.80 g/dL (p < 0.00001). This represented a substantial improvement in the condition's most important clinical outcome.
These weren't marginal differences. They were large, consistent, and highly statistically significant across diverse populations.
The Paradox Revealed
Then came the counterintuitive finding that makes this data so scientifically fascinating: fractional iron absorption with lactoferrin was actually lower than with ferrous sulfate, decreasing by 2.08% (p = 0.02).[4]
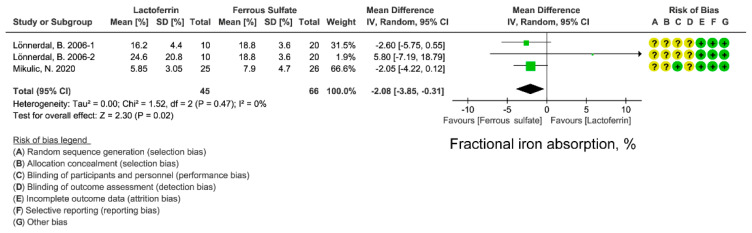
The Paradox Revealed: Lower Absorption, Better Outcomes. Lactoferrin supplementation resulted in 2.08% lower fractional iron absorption compared to ferrous sulfate (p = 0.02). This contradicts conventional logic: if lactoferrin absorbs less dietary iron, how does it deliver superior clinical outcomes? The answer lies in restoring the body's ability to access iron already present in storage.[4]
Read that again. Lactoferrin led to less iron absorption than ferrous sulfate, yet delivered better clinical outcomes across every measure of iron status and function.
This violated the basic logic that's driven iron supplementation for decades. If lactoferrin provides less absorbable iron, how does it improve iron status more effectively? The answer requires rethinking what's actually limiting iron status in these populations.
The Resolution: It’s Not About Absorption
The key came from measuring inflammatory markers. Lactoferrin supplementation significantly reduced IL-6, a primary inflammatory cytokine, by 45.59 pg/mL compared to ferrous sulfate (p < 0.00001).[4]
This massive reduction in inflammation explains everything. By lowering IL-6, lactoferrin reduces hepcidin production. Lower hepcidin means ferroportin remains functional. Functional ferroportin allows iron to exit storage cells and reach circulation. The body's existing iron stores mobilize and become available.
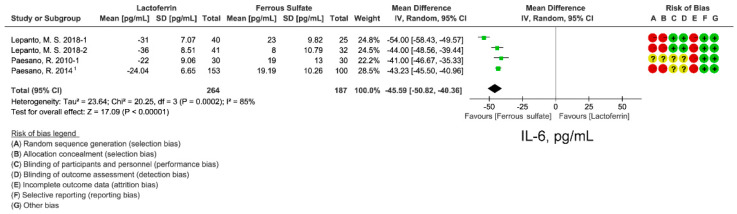
The Mechanistic Resolution: Inflammation Drives Iron Restriction. Lactoferrin supplementation reduced serum IL-6 by 45.59 pg/mL compared to ferrous sulfate (p < 0.00001). This dramatic reduction in inflammatory signaling explains lactoferrin's superiority despite lower absorption. By suppressing IL-6, lactoferrin lowers hepcidin production and restores iron mobilization from existing stores, addressing the regulatory dysfunction that limits iron availability during chronic inflammation.[4]
Lactoferrin wasn't winning by delivering more iron. It was winning by restoring the body's ability to use the iron already present.
How Lactoferrin Actually Works
The Zhao meta-analysis revealed lactoferrin's superiority but left questions about precise mechanisms. Additional research has clarified lactoferrin's dual approach to supporting iron homeostasis.
-
Mechanism 1: Inflammation Modulation
Lactoferrin's anti-inflammatory effects extend beyond IL-6 reduction. It modulates immune responses at multiple levels, reducing pro-inflammatory signaling while supporting regulatory pathways that resolve inflammation.[5]
By suppressing IL-6-driven hepcidin production, lactoferrin allows ferroportin to remain on cell surfaces. This releases iron trapped in macrophages (where recycled iron from old red blood cells accumulates) and enterocytes (intestinal cells that absorb dietary iron).[5] Rather than forcing more iron into an already dysfunctional system, lactoferrin restores normal iron trafficking.
Laura Katz and Pamela Besada-Lombana take us inside Helaina's Manhattan R&D facility to reveal the precision fermentation science, clinical breakthroughs, and empathy-driven culture behind effera® lactoferrin on Episode #197 of the PricePlow Podcast.
This approach addresses a fundamental limitation of standard iron supplements: they don't fix the underlying regulatory dysfunction. Ferrous sulfate can even worsen inflammation through oxidative stress, potentially elevating hepcidin further and creating a counterproductive cycle.
-
Mechanism 2: Intelligent Iron Delivery
Lactoferrin also supports iron absorption through direct mechanisms. It binds iron with high affinity, protecting it from interactions that would otherwise limit bioavailability. When lactoferrin reaches the intestine, it can transfer iron to lactoferrin receptors on intestinal cells, providing an alternative absorption pathway to standard non-heme iron absorption.[6]
Research has shown that apo-lactoferrin (lactoferrin without iron bound) can actually enhance iron absorption more effectively than holo-lactoferrin (iron-saturated).[7] In infants, apo-lactoferrin increased iron absorption by 56% compared to holo-lactoferrin, suggesting that lactoferrin's ability to mobilize endogenous iron may be more important than the iron it carries.
This dual mechanism works synergistically. Inflammation modulation restores systemic iron regulation, while intelligent delivery ensures dietary iron reaches tissues effectively. Together, they support iron homeostasis rather than attempting to override it.
Why Structure Matters: effera® as Human-Identical Lactoferrin
Lactoferrin's clinical benefits are clear, but not all lactoferrin is equivalent. Most commercial lactoferrin comes from bovine milk, which shares approximately 70% amino acid sequence homology with human lactoferrin.[8] Those differences matter.

We went behind the scenes at Helaina's Manhattan lab to see how they make human-identical effera™ lactoferrin through precision fermentation.
The Bioequivalence Question
In 2024, researchers published landmark results from a randomized, double-blind trial directly comparing human-identical lactoferrin (effera®, produced via precision fermentation in Komagataella phaffii) against bovine lactoferrin.[9]
The study followed 66 healthy adults for 84 days, measuring antibody responses to supplemented lactoferrin as the primary endpoint. This addressed a critical safety question: could consuming non-native lactoferrin trigger immune responses that would limit efficacy or safety?
The results revealed a striking difference between lactoferrin sources:
- Bovine lactoferrin triggered a significant antibody response. By day 56, antibody levels had increased approximately 3-fold compared to baseline (post/pre ratio: 3.01).[9] The body recognized bovine lactoferrin as foreign and mounted an immune response against it.
- effera® at both dose levels (340 mg/day and 3,400 mg/day) showed no significant antibody increase.[9] The post/pre ratios were 1.07 and 1.02, respectively, indicating the immune system treated effera® as self rather than foreign.
You can read more about this groundbreaking trial in our detailed coverage on the Peterson 2024 study and our podcast with Dan DeMarino and Anthony Clark where they discuss the significance.
Production and Safety Profile
effera® is produced through precision fermentation using Komagataella phaffii yeast engineered to express human lactoferrin. The result is a protein with identical amino acid sequence to human milk lactoferrin, making it structurally indistinguishable from the lactoferrin naturally present in human tears, saliva, and other bodily fluids.
Watch how it's made in our tour of Helaina's Manhattan facility, where we got exclusive access to their precision fermentation process.
Safety testing has been extensive. GLP-certified studies established a no-observed-adverse-effect-level (NOAEL) of 2,000 mg/kg body weight per day in rodents, roughly 400 times the proposed human intake levels. Comprehensive immunotoxicity testing showed no adverse effects on immune function. effera® has achieved GRAS status and received substantiation through the CARSE process, confirming its safety as a food ingredient.
The human-identical structure offers clear advantages: no foreign epitopes to trigger antibody responses, optimal binding to human lactoferrin receptors, and function that mirrors endogenous lactoferrin throughout the body. For applications targeting iron homeostasis, immune support, or gut health, these structural differences translate to meaningful functional advantages.
What This Means for Consumers
The iron homeostasis framework changes how we should think about iron supplementation:
- Not everyone needs more iron. Many people with low iron status already have adequate stores that are simply unavailable due to elevated hepcidin from chronic inflammation. Adding more iron won't fix this regulatory problem and may worsen it through oxidative stress.
- Context determines strategy. For acute, severe iron deficiency without inflammation, high-dose ferrous sulfate may still be appropriate under medical supervision. For chronic low-grade iron insufficiency, inflammation-associated iron restriction, or maintenance of healthy status, lactoferrin offers a fundamentally different and potentially superior approach.
- Dosing matters. Clinical studies of lactoferrin have used doses ranging from 100 mg to 340 mg daily, with the Zhao meta-analysis showing benefits across this range. effera®'s Peterson trial tested up to 3,400 mg daily with excellent safety and no antibody response, meaning the body recognizes effera as endogenous, but most applications use doses in the 100-300 mg range.
- Target populations benefit most. Several populations stand to benefit most from lactoferrin's approach to iron homeostasis:
- Menopausal women face a clear application: declining estrogen levels often trigger increased inflammation and hepcidin expression, creating the exact dysfunction lactoferrin addresses.
- Pregnant women benefit through multiple pathways beyond iron regulation alone, including support for fetal development, immune modulation during critical periods, and reduced risk of pregnancy complications.
- Athletes experiencing both training-induced inflammation and increased iron turnover may benefit from lactoferrin's dual mechanism of inflammation reduction and intelligent iron delivery.Anyone with chronic inflammatory conditions affecting iron status represents a candidate for this approach.
Integration with existing protocols is straightforward. Lactoferrin can be taken with or without food, and there's no need to separate it from other supplements or medications (unlike ferrous sulfate, which has numerous interactions).
Biology Over Buzzwords: A New Framework
The shift from "more iron" to "better regulation" reflects a broader principle that applies far beyond iron supplementation. Human biology optimizes for homeostasis. Systems that have long evolved to maintain balance don't respond well to brute-force interventions that ignore regulatory mechanisms.
The Zhao meta-analysis demonstrated this principle quantitatively. Lactoferrin's superiority came not from delivering more iron, but from supporting the body's existing regulatory machinery. By reducing inflammation and restoring hepcidin balance, lactoferrin allowed natural iron homeostasis to function properly.

Laura Katz, founder and CEO of Helaina, discusses the revolutionary effera™ human-identical lactoferrin technology and precision fermentation platform on Episode #167 of the PricePlow Podcast.
effera® takes this framework further by providing human-identical structure. The Peterson trial's demonstration of no antibody response with effera® versus significant antibody production with bovine lactoferrin shows that even subtle structural differences matter when trying to optimize for the best biological outcomes within the body.
This represents a new standard for iron support: supplements that work through homeostatic regulation rather than pharmacological override. As research continues to reveal lactoferrin's mechanisms in gut health, immune function, and longevity applications (topics for future coverage), this framework will only grow more relevant.
For now, the iron story provides a clear proof of concept. When you understand biology, you can design smarter interventions. The "more iron" trap kept millions supplementing ineffectively because it ignored the fundamental principle: the body doesn't need more iron dumped into a broken system. It needs the regulatory mechanisms that control iron fixed.
That's where biology, not buzzwords, leads us. A better solution comes in the form of lactoferrin, and a better form of lactoferrin comes from Helaina, the sponsors of this article, as none other than effera®.
Want to learn more about effera®? Check out our comprehensive overview or listen to our latest podcast with Helaina's leadership discussing the company's growth and future directions.