Jocko Willink is one of America's foremost exponents, and exemplars, of self-discipline – and most of us would agree that discipline is a huge factor in personal success. He's also the founder of Jocko Fuel, one of the hottest new brands in the supplement market.
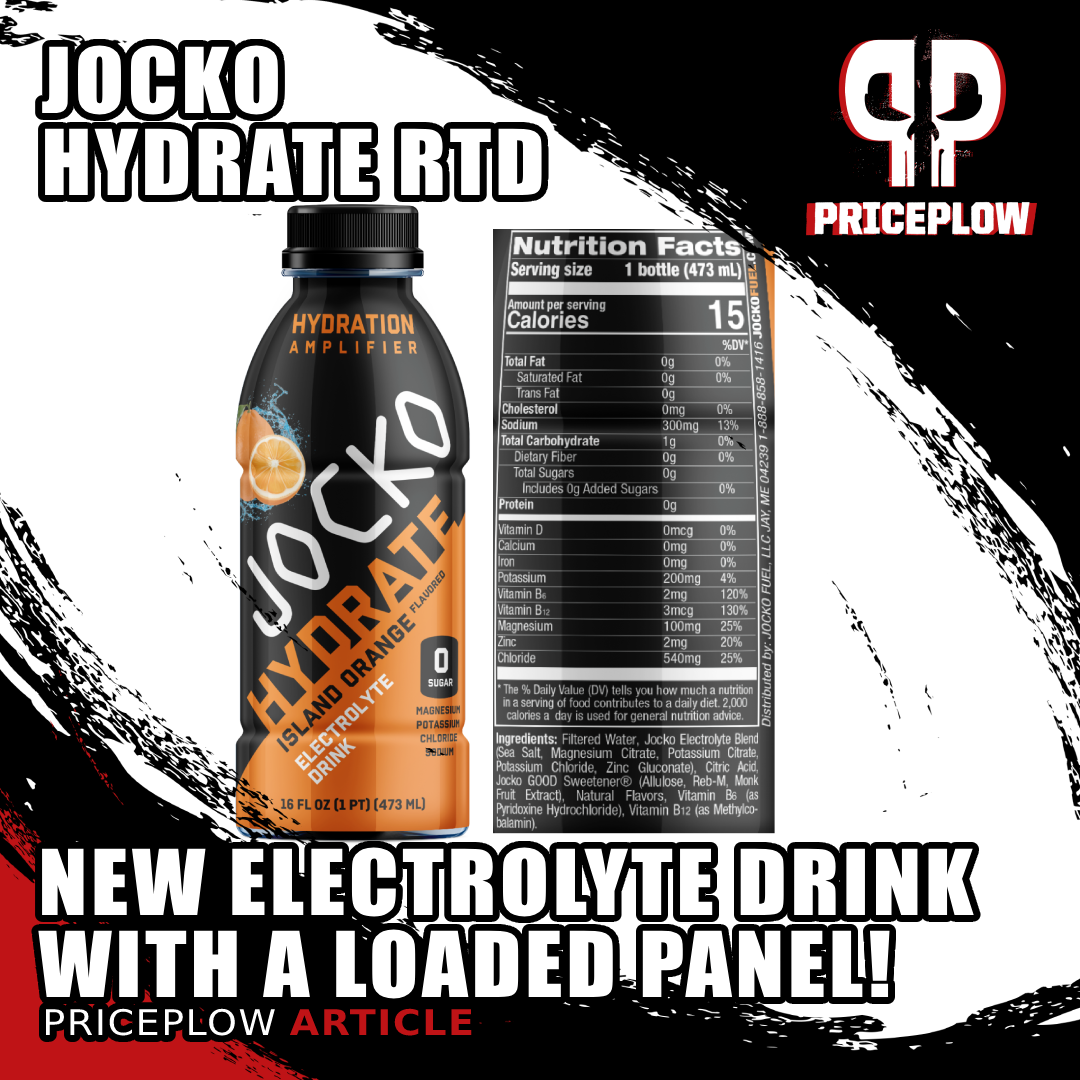
Jocko Fuel has revealed the Jocko Hydrate RTD drink, an absolutely delicious hydration beverage that stays true to Jocko's mantra of no artificial colors or sweeteners
When it comes to physical training, willpower matters a lot. But let's be real, no matter how mentally tough you are, the human body has physical limits. Among those limits, hydration is one of the most important. Nothing will kill your performance, or your recovery, faster than a state of dehydration.
In order to help you keep your fluids up, Jocko Fuel has designed Jocko Hydrate RTD, an incredibly tasty beverage loaded with key electrolytes and vitamins that you can drink on the fly. And when we say tasty, we mean it -- you won't believe this is naturally flavored and sweetened!
Over time, we've seen the supplement industry's typical electrolyte profile expand, and Jocko Hydrate RTD is a great demonstration of this trend. Here we have not only sodium, potassium, and magnesium in a 3:2:1 ratio, but zinc as well. So, in addition to the full complement of electrolytes, you'll also get some crucial testosterone support.
PricePlow Podcast Episode #132 – Jocko Himself!
In case you missed it, check out Episode #132 of the PricePlow Podcast in which we interviewed Jocko at the 2024 Vitamin Shoppe expo. In this episode, we discuss the genesis of Jocko Fuel, as well as Jocko's creation of the company with co-founder and chief product officer (CPO) Brian Littlefield of Episode #111.
Now let's get into the formula, but first, check prices and availability on PricePlow, and sign up for our Jocko Fuel news alerts:
Jocko Fuel Hydrate Drink RTD – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
This area is reserved for Team PricePlow's upcoming videos.
Subscribe to our channel and sign up for notifications so you catch it when it goes live!
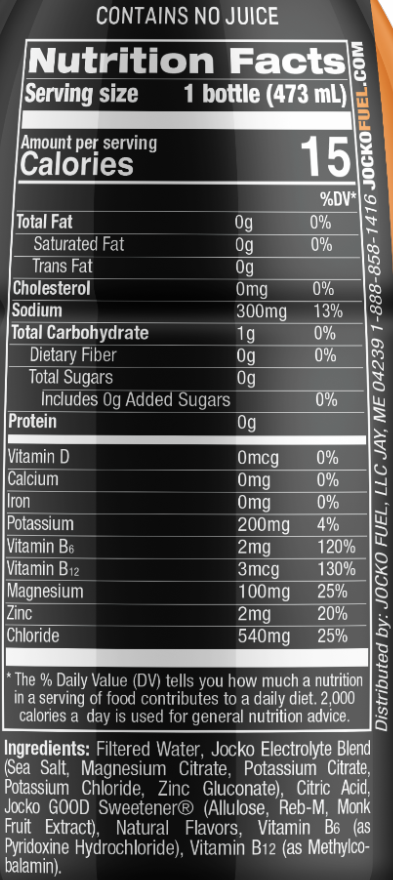
Jocko Hydrate RTD Ingredients
In a single 473 mL (16 ounce) serving of Jocko Hydrate RTD, you get the following:
-
Sea Salt - Providing 300 mg Sodium (13% DV)
Americans today live in fear of sodium, and try to minimize our intake wherever possible. So, you may be surprised to see that a single serving of Jocko Hydrate RTD contains about 300 mg sodium, which is 2-3 times more than the typical sodium content of hydration products.
Athletes should worry about too little sodium, not too much!
While there's definitely such a thing as eating too much sodium, there's a fine argument to be made that the threshold for harm is higher than generally believed – and that you may need a little more sodium than you think, too. As a matter of fact, sea salt is one of the most important ingredients for supporting optimal hydration, which is why we're seeing it show up more and more in RTD hydration formulas like Jocko Hydrate.
It's also worth mentioning that, as we teased in our hydration guide, Jocko Hydrate contains all the electrolytes in appropriate ratios, which helps mitigate any potential downside associated with extra sodium.
Before we start our discussion of sodium, it's important to emphasize that you should carefully consider all dietary sources of sodium when calculating your daily sodium intake.
Sodium is lost the most in sweat
So why don't we sweat the salt in Jocko Hydrate? The main reason is that hydration formulas are typically designed for consumers who are active, and presumably sweating a lot – and sodium is the primary electrolyte we lose in sweat, by a long shot. In a single liter of sweat, we lose about 0.9 grams of sodium, on average, with the second-biggest loss being potassium at a mere 0.2 grams per liter.[1] Given that we lose more than four times as much sodium as potassium,[1] you can see why we might be interested in replacing sodium specifically.
If you're exercising, doing manual labor, or even just going for a brisk walk in the heat, you could lose enough sodium to end up sodium deficient, especially if your dietary sodium intake is low, which is a pretty common scenario among health-conscious consumers eating a whole-foods based diet. Too little sodium and your muscles' ability to contract may be impaired,[2] as muscles that can't access adequate sodium typically work below their full capacity.[3]
In serious cases, sodium deficiency caused by dehydration — the technical term for which is hyponatremia — can be fatal![4]
The question of exactly how much sodium any given person needs is a fairly involved discussion in its own right. So, if you want to learn about that, check out PricePlow's Ultimate Hydration Guide.
Where's the threshold for sodium intake?
Even though there's a legitimate need for extra sodium in certain cases, it's definitely possible to get too much. So how much is too much? As is the case with so many other topics in nutritional science, the long-standing consensus is being questioned by emerging research.
Despite the fact that Americans have long been told to consume no more than 2,300 milligrams of sodium per day, there's reason to believe this recommended maximum may actually be closer to the minimum sodium needed by most people. The reason this matters is that, ironically, the negative effects of consuming too little sodium resemble those of consuming too much. A 2015 research review points out that (emphasis ours):[5]
"[C]urrent evidence from prospective cohort studies suggests a J-shaped association between sodium intake and cardiovascular events, based on studies from >300 000 people, and suggests that the lowest risk of cardiovascular events and death occurs in populations consuming an average sodium intake range (3-5 g/d). The increased risk of cardiovascular events associated with higher sodium intake (>5 g/d) is most prominent in those with hypertension."[5]
In other words, the negative effects of consuming too much sodium don't even start until you hit 5,000 mg per day, and consuming less than 3,000 mg a day is statistically associated with the same type of cardiovascular mortality as consuming too much. Note that this 3,000 mg minimum is actually higher than the 2,300 mg maximum that has been officially recommended for so long.
Get ready for an epic interview - in Episode #111 of the PricePlow Podcast, we brought on Brian Littlefield, Chief Product Officer of Jocko Fuel, who announces the new naturally-sweetened Jocko Pre-Workout
The conclusions of this meta-analysis were uncannily borne out by one study in particular, which found that patients whose urinary sodium excretion indicated a dietary intake of less than 3,000 mg per day had a higher risk of being hospitalized for congestive heart failure.[6] What's more, this study found that sodium intakes up to 7,000 mg per day did not, on average, increase the subjects' risk of cardiovascular disease.[7]
An earlier meta-analysis, from 2011, looked at seven different studies and concluded that salt restriction actually increased cardiovascular mortality in heart disease patients.[8]
Are we saying that you, specifically, should start generously salting your food? No – dietary matters must be tailored to the individual. So please, before you adjust your sodium intake, ask your doctor whether that's a good idea.
But we do think the 300 mg of sodium in Jocko Hydrate RTD is probably good for most people. (Again, talk to your doctor!)
Regarding the individual variability in sodium response, we should mention a particularly interesting study from 1987 that discussed the fact that for any given patient, consuming more sodium was roughly as likely to lower their blood pressure as it was to raise it. Interestingly, most participants saw no blood pressure change whatsoever in response to altered sodium intake.[9]
On the other hand, a different study — a randomized controlled trial (RCT) — found that patients who ate a low-sodium diet had a 25% lower risk of heart attack or stroke compared to a placebo (sham intervention).[10] Since RCTs are very high quality evidence, we do need to take this result seriously.
Ultimately, it depends on multiple personal factors, your blood pressure, and your individual biology and medical history. Talk to your doctor if you have any questions about whether an additional 300 mg of sodium will be an issue for you.
-
Potassium (as Potassium Citrate and Potassium Chloride) – 200 mg (4% DV)
Potassium is another key shortfall nutrient,[11] and is especially important as the electrolyte that balances sodium. In fact, there's some research that strongly suggests one's potassium-to-sodium intake ratio actually has a bigger impact on cardiovascular health than sodium intake alone.[12-16]
Since some studies have found that sodium restriction is very difficult to implement in practice,[17,18] this means that increasing potassium consumption may be a better strategy for minimizing cardiovascular disease risk.
Important for vasodilation
Unsurprisingly, in light of its impact on cardiovascular health, potassium is a potent vasodilator.[19-21] So, as a bonus, this ingredient may help you get a better pump in the gym. But realistically, this dose is so small that in the context of the Jocko Hydrate RTD formula, it's better to understand it as helping counterbalance sodium.
-
Magnesium (as Magnesium Citrate) – 100 mg (25% DV)
Magnesium is a mineral that's absolutely crucial for optimal health. It's also an electrolyte, which is why it's in Jocko Hydrate.
The mineral plays a central role in more than 600 different metabolic processes within the human body, including cellular energy production and ribosomal protein synthesis.[22] It's no surprise, then, that even a mild magnesium deficiency can wreak absolute havoc on one's health.
Brain health
Magnesium is an important building block for neurotransmitters.[23] We all know how important neurotransmitters are for brain health, emotional self-regulation, and cognitive performance – but they're also key for sleep and relaxation. For instance, the neurotransmitter gamma aminobutyric acid (GABA) requires a plentiful supply of magnesium ions for its synthesis to occur,[24] which is one of the main reasons why magnesium supplementation can have an immediate, noticeable, and positive impact on anxiety and stress.
Need more? Jocko Magnesium is here with a 3-ingredient blend to support recovery, sleep, and stress!
Remember that GABA is an inhibitory neurotransmitter, meaning it opposes the action of glutamate, your brain's main excitatory neurotransmitter. These two neurotransmitters need to be properly balanced for brain health. And since magnesium supplementation can help muscles relax, it can relieve tension in the most literal sense possible.[25,26]
Keeping magnesium stores topped off is especially important given the role the mineral plays in sleep regulation, and the fact that dysregulated sleep severely increases one's risk of serious health problems.[27] For example, a 2015 study showed that among men and women under the age of 65, those with even a slight shortfall were 22% more likely to have depression.[24]
There's a great meta-analysis that demonstrates magnesium can consistently improve symptoms of anxiety and stress.[28] The sheer volume of this data qualifies magnesium as one of the best-researched supplements in existence.
Conversely, untreated magnesium deficiency can give rise to all sorts of issues linked to stress and anxiety, including chronic fatigue.[23,29,30]
Magnesium's impact on mood, stress and anxiety is enough on its own to justify magnesium supplementation, but it turns out there's even more to this amazing mineral than that:
Decreases cortisol
We've already discussed how magnesium supplementation can increase both the quantity and quality of sleep.[31,32]
One of the most important mechanisms behind this pro-sleep effect is magnesium's ability to downregulate cortisol, your body's main glucocorticoid stress hormone. Given that we all have to deal with our fast-paced, 24/7 interconnected modern world, anything that can help us keep cortisol under control is a potentially powerful tool in our health arsenal. If you're feeling a little run down lately, consider the possibility that magnesium supplementation could help you sleep better.[32]
One especially compelling study showed that magnesium intake correlates inversely with sleep midpoint. This means that people who ingest adequate magnesium generally fall asleep earlier in the evening than those who don't.[33]
Metabolism
While sleep and mood are the two dimensions of health most palpably impacted by magnesium supplementation, there are others too. Again, given the fact that magnesium is implicated in such a vast array of cellular-metabolic processes, it's not surprising that correcting a magnesium deficiency could have broad implications for human health.[34-36]
Here's just a partial list of the benefits:
- Lower blood pressure[37-40]
- Decreased HbA1c and better blood glucose control[37,41,42]
- Increased insulin sensitivity[37,41-43]
- Lower risk of type 2 diabetes and metabolic syndrome[44-46]
If you're on any kind of restrictive diet, including caloric restriction, monitoring your daily magnesium intake is probably one of the most important things you can do to ensure optimal mental and physical health. There's so much that can go haywire when your magnesium levels drop too low.
Athleticism
Of course, we're talking about Jocko, and this is a hydration formula, so we definitely need to wrap this up with a little discussion of the athletic benefits associated with magnesium supplementation. They include:
- Increased bone mineral density[12]
- Quicker lactic acid (lactate) detoxification[13]
- Increased lean mass and athletic power[14]
- Decrease in exercise-induced stress and muscle damage[11,15]
Next time you're killing it in the gym after hitting Jocko Pre-Workout or dominating the mats with Jocko GO Energy Drink, consider the steps you'll need to take for recovery, and consider adding a magnesium-rich supplement like Jocko Hydrate RTD. Especially because, as is the case with all electrolyte minerals, you're liable to lose a significant amount of magnesium in sweat.[16]
-
Zinc (as Zinc Gluconate) – 2 mg (20% DV)
Zinc is referred to as the master mineral of the male endocrine system for good reason – it's absolutely indispensable for testosterone synthesis.
Even slight shortfalls in zinc intake can wreak absolute havoc on T levels. According to one 1996 study, dietary zinc restriction can cause a 75% drop in T, from about 40 nmol/L to 10 nmol/L, on average.[47] That's an incredibly large decrease. The same study also found that providing elderly, mildly-zinc-deficient men with zinc supplements doubled their T, from 8 nmol/ to 16 nmol/L.[47]
These kinds of effect sizes – 75% decreases, 100% increases – are far beyond what we usually see in nutritional research. Needless to say, anyone who's trying to maximize testosterone should avoid zinc deficiency at all costs.
Even if you're consuming enough zinc, supplementing with this mineral can still improve your overall androgenic profile. That's because zinc also plays an important role in boosting dihydrotestosterone (DHT),[48] one of testosterone's most active metabolites and the one that's arguably the most masculinizing of the androgens.[49]
-
Vitamin B6 – 2 mg (120% DV)
Jocko Willink joins PricePlow for Episode 132 to talk about founding Jocko Fuel, doing the right thing when formulating supplements, and Jocko's entire stack from start to finish
Vitamin B6 is a building block for key metabolic coenzymes like pyridoxal 5' phosphate (PLP) and pyridoxamine 5' phosphate (PMP), which are both required for hundreds of metabolic reactions in the human body.[50] Among other things, both enzymes are involved in protein metabolism, which we think you'll agree is pretty important.[50]
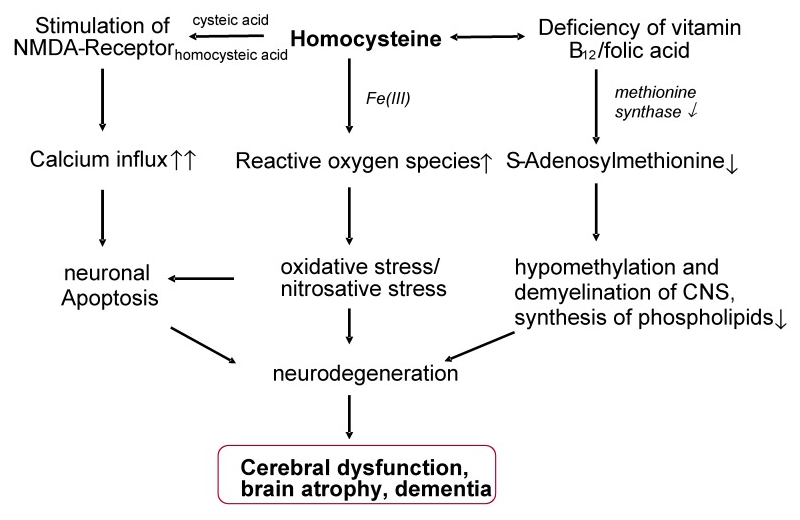
The vitamin is also needed for the production of neurotransmitters like dopamine, meaning it can help support cognition.[50] It also regulates homocysteine, an amino acid that can increase one's risk of cardiovascular problems if blood level rise too high. Vitamin B6 is also involved in hemoglobin synthesis, immune function, gluconeogenesis, and glycogenolysis.[50]
Studies show that taking B6 is associated with decreased risk of cardiovascular disease, cancer, and cognitive dysfunction.[50]
-
Vitamin B12 (as Methylcobalamin) – 3 mcg (130% DV)
Methylcobalamin is PricePlow's favorite form of vitamin B12. This particular B12 vitamer acts as a methyl donor, which enables it to support an impressive range of methylation-dependent metabolic processes.[51]
This vitamin is required for red blood cell synthesis, and its deficiency can cause megaloblastic anemia,[52,53] a form of anemia characterized by red blood cells that are larger, but less numerous. This corresponds to a net decrease in aerobic capacity.
Thanks to its impact on methylation, vitamin B12 plays some of the same metabolic roles as folate. For example, low B12 is linked to high homocysteine, and in pregnant women, a significantly increased risk of birth defects.[54-56]
Similar to folate, B12 plays an important role in maintaining homocysteine homeostasis. Thanks to this – and its role as a precursor to S-adenosylmethionine (SAMe) – even slight B12 deficiencies can cause irreversible brain damage.[57]
Even slightly deficient levels of B12 – on the low side of the normal range, even – are linked to impaired memory performance,[58] thanks largely to B12's homocysteine-regulating effect.[57] But since B12 is also a key building block for S-adenosylmethionine (SAMe), that makes it important for methylation, myelination, and phospholipid synthesis in the central nervous system.[57]
While B12 supplementation hasn't been proven to increase energy levels in non-deficient subjects, fatigue is an early and crippling symptom of B12 deficiency,[59] and something we would obviously like to prevent. Since B12 is water soluble, the body rapidly excretes any excess, making the risk of supplementing with this vitamin generally quite low.
-
Jocko GOOD Sweetener (Allulose, Reb-M, Monk Fruit Extract)
Finally, although the dose isn't specified, including the Jocko GOOD Sweetener is more about what you avoid. We're huge fans of Jocko's commitment to all-naturally-sweetened products, since the jury is very much still out on the health impact of the most synthetic stuff.
You can listen to this discussed in great detail in Episode #111 of the PricePlow Podcast with Brian Littlefield, who formulates these products, and works painstakingly hard to keep it delicious while he keeps the sweeteners natural.
Flavors Available
Hydration: The Ultimate Guide. How do you stay hydrated? This article covers the best approach to fluid and electrolyte intake, also cautioning against what may harm your hydration status
As mentioned above, all of Jocko's flavors are naturally flavored, naturally sweetened, and have no artificial colors! Below is a list of all available flavors:
Conclusion: An RTD Hydration Drink for Grown-Ups
Jocko Hydrate RTD has all the makings of a state-of-the-art hydration formula – a moderate dose of sodium to help offset sweat losses, balanced by a little potassium, plus some key B vitamins for energy and methylation support. It's worth stressing that formula also contains magnesium, which at this point is a standard hydration-formula ingredient and the use of which is one of the best recent industry trends.
Where Jocko Hydrate RTD differs from the typical hydration product is in its use of zinc, which makes a ton of sense. We're hoping this trend catches on just like magnesium did.
Jocko Fuel Hydrate Drink RTD – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.









Comments and Discussion (Powered by the PricePlow Forum)