Four-time World's Strongest Man Brian Shaw founded Undefined Nutrition with one goal in mind: to help people transition from a state of undefined potential to defined accomplishment.
His philosophy is that necessity drives innovation. We think this is exemplified by the formula we'll be discussing today: Undefined Nutrition's Structure.
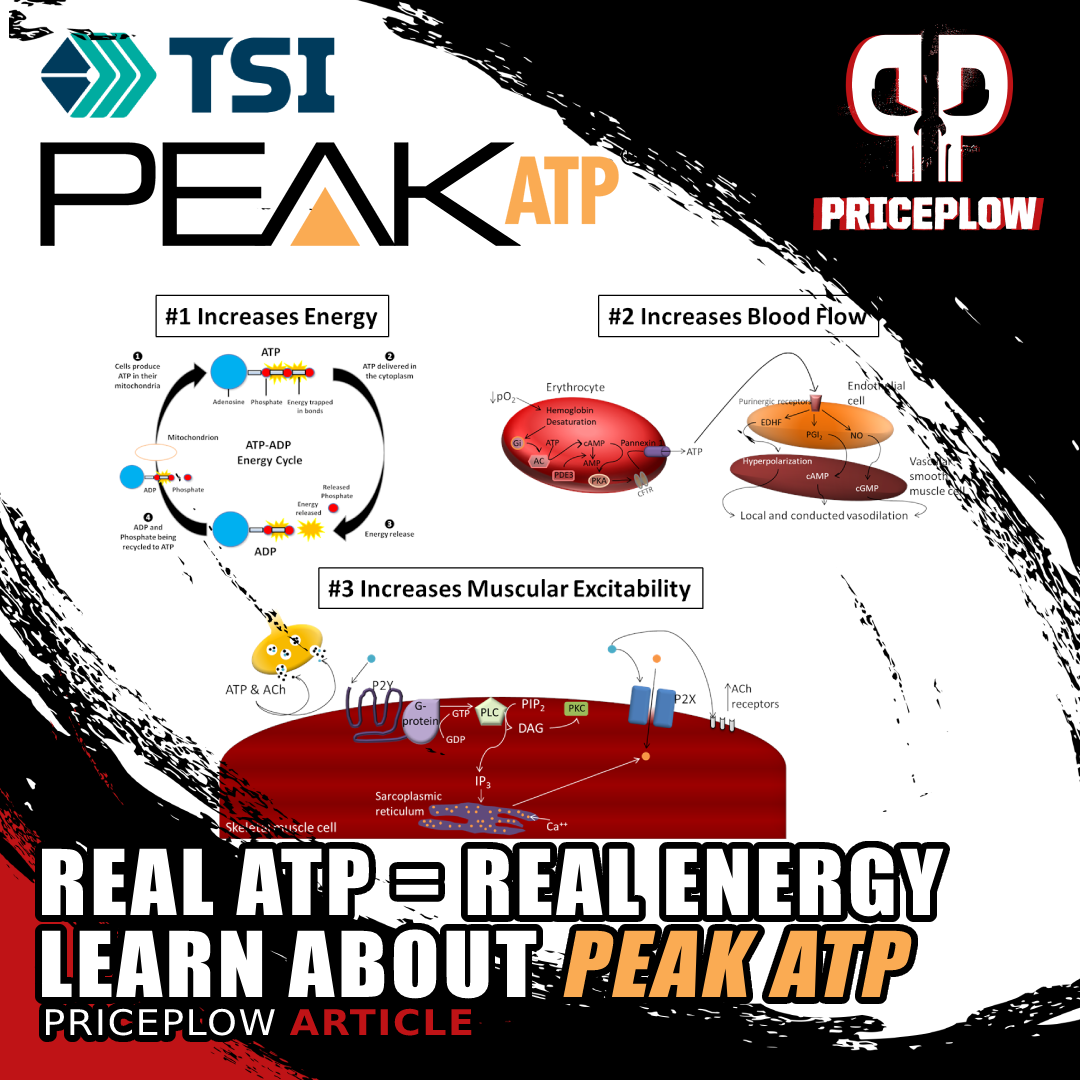
Structure is designed to maximize the anabolic and cardiovascular response to whatever killer workout you just crushed in the gym. Its innovation is in the use of ingredients like Peak ATP, which helps directly replenish cellular energy stores post-workout.
Everything you need to know about Peak ATP
In case you missed it, PricePlow has published a ton of Peak ATP data recently. Back in October, we came out with a massive guide titled "PEAK ATP: The Ultimate Guide to Disodium ATP Supplements". If you aren't sure what ATP is or why it's important – or you still think that oral ATP supplementation doesn't work – you've got to click the link and check out this article.
We also recently had a chat with Dr. Ralf Jaeger, one of PricePlow's favorite biochemistry and sports nutrition experts, about how ATP can benefit athletic performance – and not in the way most people expect! If you don't know what we're alluding to here, check out our interview with him at Dr. Ralf Jaeger: Using ATP for Nitric Oxide & Blood Flow | PPP #078.
HMB: Should We Call It A Comeback?
Also making an appearance is HMB, an ingredient that brought a serious amount of hype back in the early 2000s when it first appeared on the scene. Looking at the scientific literature from the vantage point of 2023, we've found some interesting connections, and agree with Undefined Nutrition's thinking that the ingredient has some latent potential.
So, is Brian Shaw and his team at Undefined Nutrition pioneering the re-discovery of its muscle-building potential? We believe so!
We'll get into the research behind both Peak ATP and HMB, as well as the two forms of creatine used, but first, sign up for PricePlow's news alerts on Peak ATP and HMB, and see where you can get Undefined Structure:
Undefined Nutrition Structure Creatine+ – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
This area is reserved for Team PricePlow's upcoming videos.
Subscribe to our channel and sign up for notifications so you catch it when it goes live!
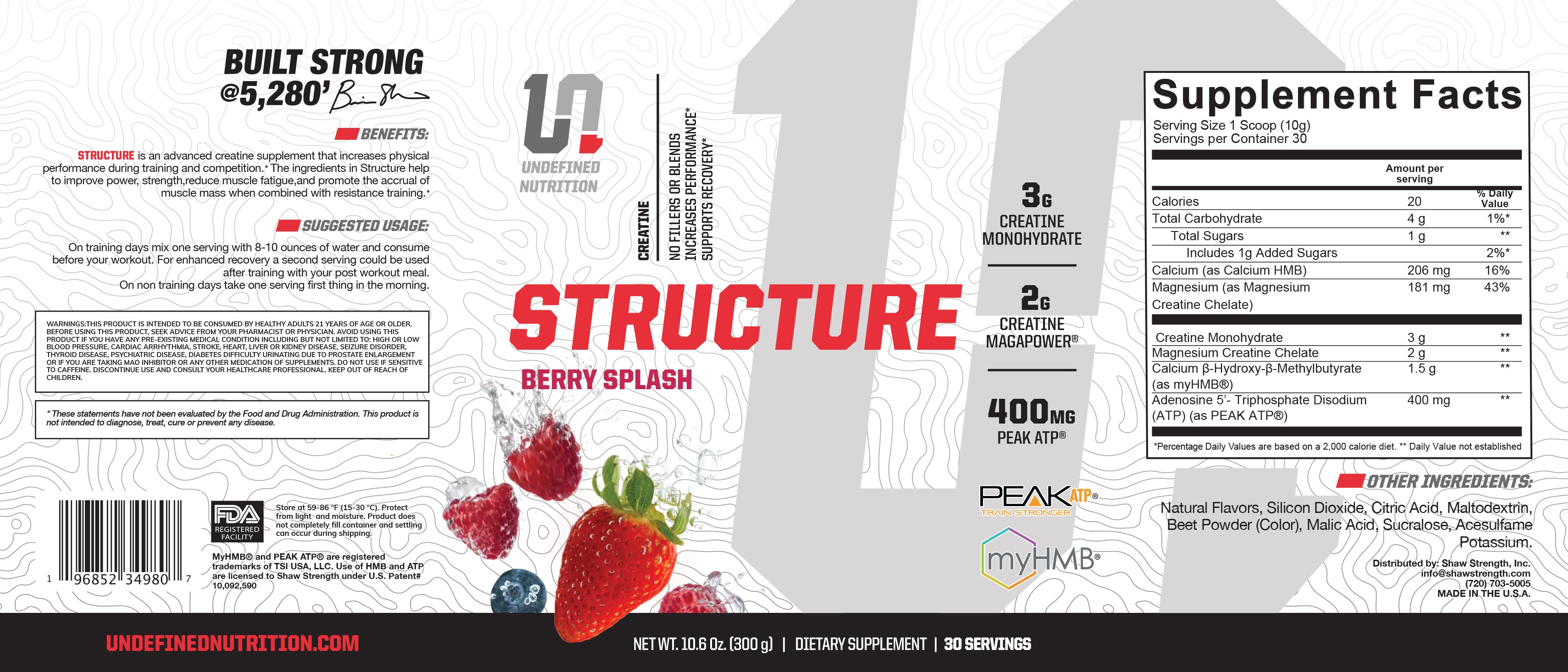
Undefined Structure Ingredients
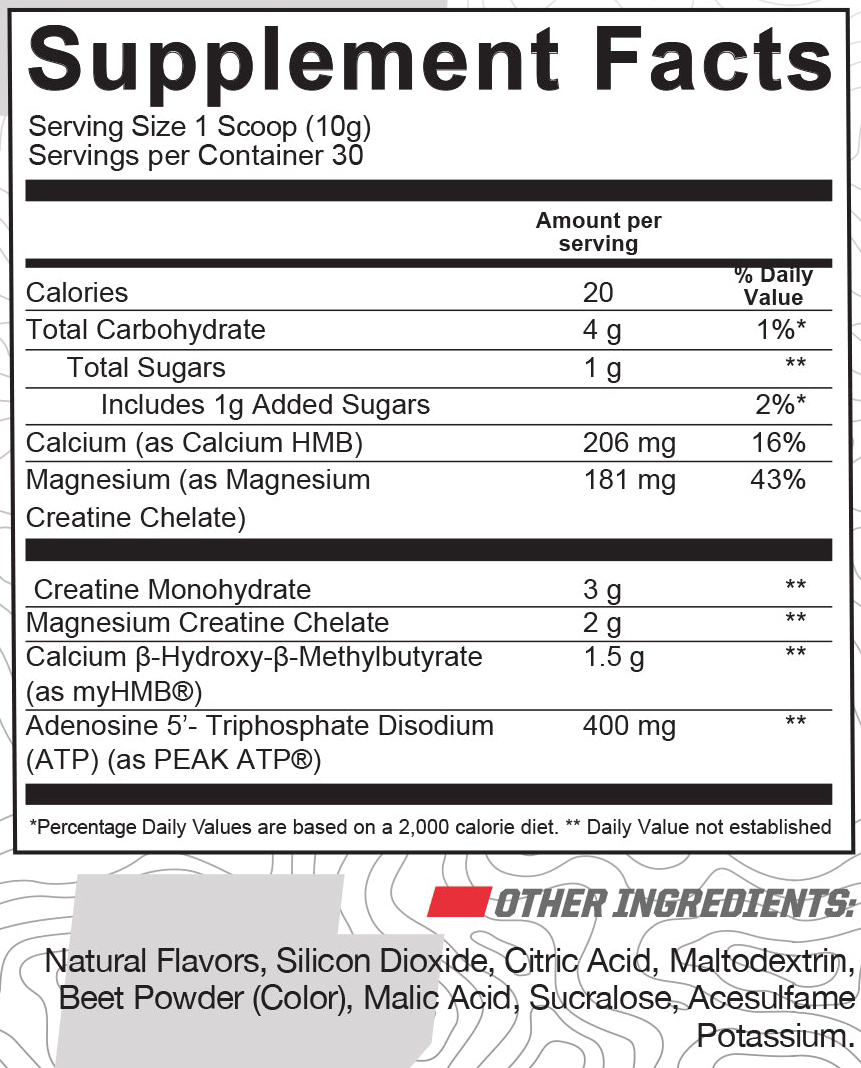
In a single 1-scoop (7.5 gram) serving of Structure from Undefined Nutrition, you get the following:
-
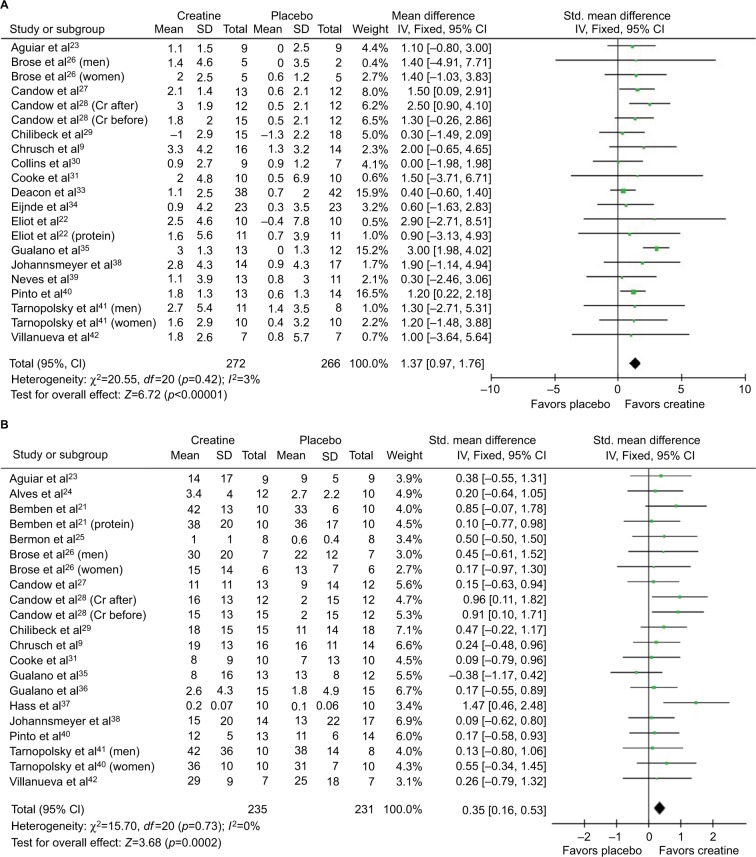
Creatine Monohydrate – 3,000 mg
For veteran supplement consumers, creatine needs no introduction. Almost everybody who's touched a barbell has tried supplementing with creatine at some point. As you can see from the label to the right, this is one of two creatine
Believe it or not, this now-ubiquitous supplement wasn't always so widely accepted. When creatine first showed up on the scene, it was met with a lot of skepticism. Now we know - it's beyond safe and effective.
Creatine's benefits
So why would you want to take creatine in the first place? Most of us have heard that it can help muscle growth in some way. Let's get into the specifics of how it works – along with other potential benefits.
There's a mountain of research on this subject, showing that supplemental creatine can improve:
- Power output[1,2]
- Total weight gain[2]
- Lean mass (muscle) gain[2-6]
- Sprinting velocity[7-9]
- Cellular hydration[10]
- Feelings of tiredness[11-14]
- Overall feelings of well-being[15-17]
- Testosterone production[18-22]
- Bone density[5]
Meat and other animal products are the most significant dietary source of creatine. In vegans and vegetarians, groups with low average creatine intake, creatine supplements can even improve cognition.[23,24]
So if you're currently following a plant-based diet, you may consider supplementing with creatine. But seriously, if you're a fan of Brian Shaw and Undefined Nutrition, you're probably eating plenty of meat, as you should be.
How creatine works
That list of benefits resulting from creatine supplementation is impressive in its breadth – so many different seemingly unrelated aspects of human health and performance appear to be improved by it. How is it possible that a single supplement can do so much?
The answer is creatine affects one of the body's most fundamental and critical metabolic processes – adenosine triphosphate (ATP) production.
It supports ATP production by delivering phosphate groups to cells' mitochondria, the organelles responsible for ATP synthesis. The phosphate groups combine with adenosine diphosphate (ADP), thus converting ADP to ATP.[25-28]
So how big of a difference does one phosphate group make? A huge one: it's the difference between unusable energy and usable energy.
If your body were an automobile, creatine would be the gasoline. Without it, you can't even start the car. ADP is more like crude oil – it needs to be refined into gasoline before it can be burned for energy.
Creatine's not the only factor in your body's capacity for producing ATP, but it's a big one. Technically, the body can produce its own creatine, too, but this is a metabolically expensive process. Ultimately, it diverts energy away from other tasks. Giving your body exogenous creatine through supplementation frees up that energy.
Creatine monohydrate
The most epic list of creatines you'll ever seen.[43] Here, we're intereted in creatine monohydrate and magnesium creatine - two very high yield forms!
Creatine monohydrate is a creatine molecule bound to a single water molecule.[29] This is the most widely used and researched form of creatine by far, so if you want something proven, monohydrate is the form we recommend.[30]
Creatine monohydrate is 87.9% creatine by weight,[43] which means we're getting 2.637 grams of actual creatine here, as well as a 1.688 gram yield from magnesium creatine chelate below, equaling a total of 4.325 grams of total creatine.
As we'll see in the next section, 3 grams of creatine monohydrate (2.637 grams total yield) is plenty to keep most people at saturation, but Undefined Structure has more than that -- perfect for Brian Shaw's bigger followers or anyone who wants to get to saturation quicker.
Recommended creatine intake
The typical adult man loses about 1.6% to 1.7% of his total creatine reserve each day.[31,32] Women lose slightly less.[33] Speaking in absolute terms, this translates to about a 2 gram daily loss of creatine.[33] Intramuscular creatine is broken down into creatinine, which is excreted via urine.[34-36]
Thus, taking a 2-gram dose of supplemental creatine per day is a good starting point if you want to maintain your creatine levels. But if you want to boost your creatine levels above baseline, and saturate your mitochondria with those all-important phosphate groups, 2 grams per day is the bare minimum – you'll want to take more than that.
Your size, activity and body composition are also factors in your creatine requirements. The bigger, more active, and more muscular you are, the more creatine you'll probably need.
One study found that daily exercise can increase the rate of urinary creatine loss by up to 50%.[37] In other words, athletes probably need 3 grams per day as a starting dose.
The "standard" dose of creatine is 5 total grams daily – although we only have 3 grams of monohydrate per scoop of Undefined Structure, the total amount of creatine from monohydrate and MagnaPowder is more along the lines of 5 grams.
Loading phase?
The most common method for creatine supplementation is to begin with a loading phase: take 20 grams of creatine per day for one week.
This practice is backed up by research,[38] but it's not strictly necessary. The dosage in Undefined Structure should get you to saturation soon enough. But if you really care, you can add some plain monohydrate to this.
Creatine's safety profile
Fortunately, the old concerns have been laid to rest while the most up-to-date research shows conclusively that creatine supplementation is safe and effective in both adults and adolescents.[30,39,40]
A 2021 review of data collected for the famous National Health and Nutrition Examination Survey (NHANES) between 2017 and 2018 found that there's no statistical relationship between dietary creatine intake and kidney disease.[41] When it comes to supplemental creatine, even the Mayo Clinic says it doesn't appear to have any impact on kidney function in healthy people.[42]
The important phrase to consider here is "in healthy people". Creatine might be unsafe for people with pre-existing kidney disease.[42] As always, if you aren't sure whether this applies to you, seek advice from a licensed medical doctor.
-
Creatine MagnaPower (Magnesium Creatine Chelate) – 2,000 mg
Creatine MagnaPower is a chelated form of creatine. Chelated means it's bound to a mineral – in this case, magnesium. It's 84.4% creatine by weight,[43] which means we're getting 1.688 grams of creatine here (and 4.325 grams of total creatine yield after counting in the monohydrate).
We're big fans of this form of creatine because we're big fans of magnesium (and obviously of creatine as well). Let's dig in:
How does it compare to creatine monohydrate?
In one double-blind, placebo-controlled study from 2004, weightlifters were randomized and supplemented with creatine monohydrate, creatine magnesium chelate, or a placebo. The volunteers took their prescribed treatments for 10 days. At the end of this phase, the researchers assessed how much each group had improved in their 1 rep maximum bench press weight.[44]
The researchers found that both creatine groups improved more than the placebo group – and that the effect size between both creatine groups was about the same. In other words, creatine magnesium chelate appears to work as well and effectively as creatine monohydrate with no statistically significant differences between them.[44]
Better bioavailability?
There's limited evidence to suggest that creatine magnesium chelate is more bioavailable than creatine monohydrate.[45] This is because the magnesium-chelated creatine molecule appears to be more chemically stable than the creatine monohydrate molecule.[45]
Interestingly, however, another study using 5.5 grams of magnesium creatine per day for 16 weeks showed higher creatinine levels[46] than we've seen in other long-term studies using 5-10 grams per day of creatine monohydrate.[47] Creatine is
Either way, creatine MagnaPower is serving primarily as another source of creatine. However, the magnesium attached to it has benefits of its own.
Benefits of magnesium supplementation
Magnesium is a mineral that's essential for many important metabolic processes. The magnesium creatine chelate in Undefined Nutrition Structure yields 181 milligrams of elemental magnesium, or 43% recommended daily value -- not a shy amount.
Although it occurs naturally in many common foods, the magnesium content of food has been declining for at least a century, thanks to certain agricultural practices.[48-53] As a result, Americans aren't getting nearly as much magnesium as we used to.
Another equally concerning problem is that magnesium deficiency is pretty hard to detect with a high degree of specificity.[48,54] It usually manifests as fatigue, insulin resistance, and poor cardiovascular function – nonspecific symptoms that are observed in a huge range of conditions.[54,55]
Magnesium deficiency is a cofactor for over 300 enzymes, and plays a central role in glycemic control, cellular energy production, blood pressure regulation, and more.[56] It can contribute to migraines, hypertension, cardiovascular disease, type 2 diabetes, and osteoporosis.[56]
Benefits of magnesium supplementation
Studies show that magnesium supplementation can improve:
- Blood pressure[57-60]
- HbA1c and blood glucose levels[57,61,62]
- Fasting insulin[57,61,63]
- Insulin sensitivity[57,61,62,64]
- Type 2 diabetes risk[65-67]
- Bone density[68]
- PMS symptoms[69-72]
- Lactic acid metabolism during and after exercise[73]
- Muscle mass and power[74]
- C-reactive protein levels[75] and effect[76]
- Interleukin-6 (IL-6) levels[77]
- Muscle damage during exercise[78]
- Migraine risk[79,80]
- Migraine symptoms[81]
So, as you can see, there are some great reasons to include a couple grams of magnesium-bound creatine rather than just a 5 gram dump of monohydrate. If our food wasn't so strip-mined of magnesium, we wouldn't think this was a big deal. But since so many are not getting optimal amounts of the critical mineral, it is a big deal. Kudos to Shaw and his team for using this.
One thing to note is that it isn't clear how bioavailable the magnesium in this ingredient really is. We know the creatine portion is definitely bioavailable and effective, but haven't seen data on plasma magnesium levels.
So for those really concerned about magnesium status, we still suggest topical magnesium chloride lotions and/or a high-quality mineral supplement like magnesium glycinate or magnesium taurate.
-
Calcium HMB – 1,500 mg
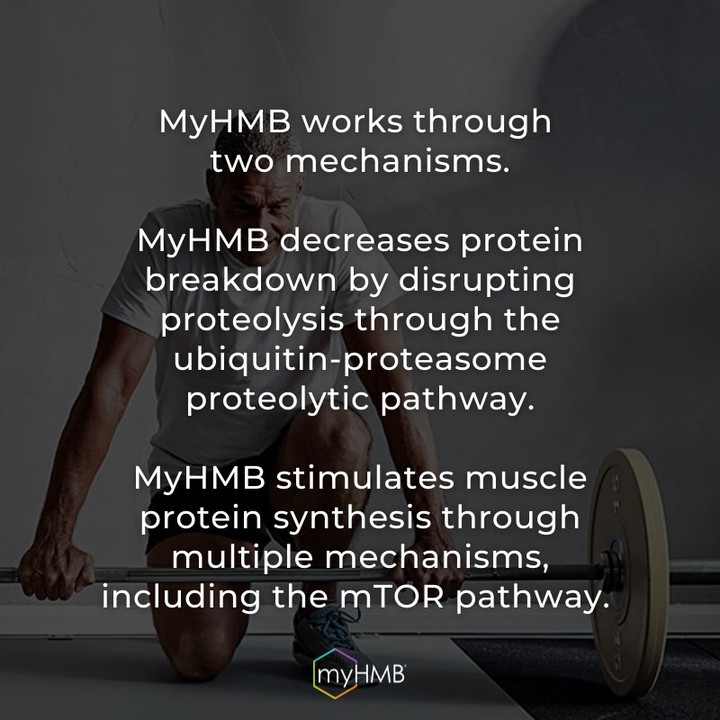
The HMB in calcium HMB stands for beta‐hydroxy‐beta‐methylbutyrate, and is a dietary supplement ingredient that's very useful for enhancing recovery enhance recovery from exercise-induced skeletal muscle damage, especially when used near a workout.[82]
Leucine: The antiproteolytic BCAA
We've written many times on the PricePlow Blog about the anabolic effects of the branched-chain amino acids (BCAAs) and leucine, which is known to be the most anabolic of the three BCAAs. It's commonly accepted that supplementing with additional leucine alongside resistance training can improve body composition and increase strength.[83-85]
Leucine has been shown to be antiproteolytic,[86] meaning that it helps prevent the hydrolysis of the body's proteins into its component peptides and amino acids. However, it takes very large doses for it to work, leading researchers to believe that there's a specific metabolite involved.[82,87] HMB was discovered to be one such molecule that significantly lowers muscle proteolysis beyond that of leucine on a gram-for-gram basis:
HMB: The leucine metabolite powering many of its effects
HMB is a leucine metabolite and has some pretty impressive anabolic effects, which are a big part of the reason why leucine supplementation helps build muscle.
The idea behind HMB supplementation is to give you the anticatabolic benefits of BCAAs more directly – cutting out the middleman, basically. However, only about 5% of leucine gets converted to HMB[88] - so if you want the effects of HMB, you either need impractically large doses of BCAAs, or you go directly to the metabolite itself.
Just like leucine, HMB helps stimulate muscle growth and prevent proteolysis (protein breakdown) by acting on the mammalian target of rapamycin (mTOR).[89]
Animal research also shows that HMB can upregulate growth hormone (GH) and insulin-like growth factor 1 (IGF-1),[90] both of which are well-established anabolic hormones.
HMB in human research trials
As usual, as much as we enjoy talking about biochemical mechanisms of action, it's just theory until the rubber meets the road. So let's see what human research has to say about the effectiveness of supplemental HMB.
So far, we've seen studies indicating that it can:
- Increase muscle mass and strength gains from resistance training[91-93]
- Improve aerobic endurance and work capacity[94-97]
- Decrease post-workout muscle damage and soreness[91,98-101]
- Accelerate recovery from exercise[102]
- Improve body composition[103]
Why didn't HMB work as well in some studies?
In the early 2000s, HMB came out with a bang, and even with the success of the studies cited above, it was perhaps over-hyped by some brands. This led to expectations that were supraphysiological, which doesn't make sense given that it's an amino acid metabolite.
No less an authority than the International Society of Sports Nutrition (ISSN) contends that past negative studies on HMB have been hampered by methodological flaws, including a lack of sufficiently intense exercise in experiment designs, and poor compliance with treatments prescribed to study participants.[82]
HMB seems to be one of those ingredients that exerts its best effects when you do as well. If you're not training hard enough and dieting strictly enough to require every last sliver of leucine and its metabolites, it's unlikely you'll get results of the successful studies that recruited athletes who did train to that level.
But if you follow Brian Shaw, "insufficient training intensity" is almost certainly a phrase that's not allowed anywhere near your household. And in that case, HMB makes total sense next to the above and below ingredients.
Learn more in PricePlow's massive HMB Guide
The above discussions are hammered out in our massive article titled HMB (β-hydroxy β-methylbutyrate): Performance-Driven Muscle Supplement - this guide gets into the above research and debate and far more, and should be read by any athlete who's training to levels like Brian Shaw does. But now it's time to get into Peak ATP:
-
Adenosine 5'-Triphosphate Disodium (Peak ATP) – 400 mg
Peak ATP is exactly what its name implies – supplemental ATP. As we already discussed, the two forms of creatine in Undefined Structure are used as part of a great strategy for boosting ATP – in the long term. But for a more immediate boost in ATP levels, it works better to supplement with ATP directly.
PeakATP is another ATP enhancing compound that is comprised of a slightly different make than elevATP and needs a much higher dose to be effective.
This is especially important because exercise – the process by which we build new muscle – consumes ATP at a high rate.[104] Thus, if we want to replace lost ATP and also keep ATP levels high during strenuous exercise, direct supplementation is the way to go.
Orally bioavailable
In the past, many supplement companies have attempted to formulate ATP supplements, but were hampered by the generally poor oral bioavailability and low shelf stability of ATP.
Peak ATP is a patent ingredient that consists of disodium ATP,[105-107] a form of ATP with verifiable bioavailability and efficacy, which, as we'll see, has been backed by a ton of research.
A 2021 research review of ATP disodium literature found more than 10 randomized controlled trials where oral ATP disodium was found to have significant positive effects on human health and performance.[108]
Workout volume
Peak ATP is a patented oral ATP supplement that's been shown to increase blood flow, boost muscle activation through calcium release, and help boost muscle mass, strength, and recovery. This article covers the biochemistry, mechanism, and human research in detail.
The key to building muscle is volume – you have to lift enough to trigger hypertrophy. And according to one 2019 study published by the Journal of Strength and Conditioning Research, ATP disodium can help with this.[109]
In this randomized, double-blind, placebo-controlled study, the subjects served as their own placebo controls by doing two different workouts. Before one workout, they got ATP disodium. Before the other, they got a placebo.[109] Again, the subjects didn't know which treatment they received, and neither did the researchers. This eliminates the potential for placebo effect bias to confound the results.
In both workouts, the subjects were trained to failure – they did squats until their muscles couldn't power through one more repetition. This is the point where the energy required by the exercise exceeds the muscles' energy supply.
The researchers kept track of total weight lifted during these workouts, which is simply the number of repetitions completed, multiplied by the weight on the bar. This is a way of calculating the total work completed during a workout.
Not only did the participants do better on ATP disodium than they did on the placebo – they did way better. In the placebo workout, they moved an average of 3,995.7 kilograms per workout.[109] In the disodium ATP workout, they moved an average of 4,967.4 kilograms per workout![109] that's a 25% increase in total volume – a huge difference.
Admittedly, this study was limited by its relatively small sample size – only 11 participants. Still, we almost never see effect sizes this big in sports supplement research.
Gains in 1RM, power, muscle thickness
In another randomized, double-blind, placebo-controlled study, resistance-trained males received either 400 milligrams of ATP disodium or a placebo for 12 weeks.[110]
In Episode #078 of the PricePlow Podcast, Dr. Ralf Jaeger dove into ATP, explaining how supplementing Peak ATP improves workout performance.
That the participants were already resistance-trained is an important detail to bear in mind. They already collected the low-hanging fruit of initial adaptations to exercise. Once you've gotten your "noob gains," additional gains are much more challenging. When, at this point, a supplement increases performance, it really says something about its efficacy.
This study is also distinguished by the fact that the participants even had their nutrition controlled by a prescribed diet.[110]
At the start of the study, the participants' 1 rep max on the big three lifts – squat, deadlift, and bench press – were measured to establish a baseline. The researchers monitored each participants' 1RM throughout the study period. The same method was applied to their vertical jump power and muscle thickness.[110]
Although both groups improved their 1RMs during the study period, the ATP disodium group gained more strength. On average, the ATP group gained about 55 kilograms on their 1RMs – the placebo group only gained 22 kilograms.[110]
The ATP group also did better when it came to vertical jump power. They improved t by approximately 15%, while the placebo group saw only an 11% increase.[110]
Most importantly, the ATP disodium group gained much more muscle than the placebo group.
The muscle thickness of the ATP disodium group increased by about 5 millimeters – the placebo group saw only half that increase.[110]
Read what the researchers had to say about this:
"In addition to ATP's capacity to buffer fatigue during repeated high volume sets and increase total training volume, the supplement may increase skeletal muscle blood flow, thereby enhancing muscle O2 recovery. This is critical as muscle deoxygenation is associated with decreased performance under repeated high intensity contractions. Specifically, extracellular ATP directly promotes the increased synthesis and release of nitric oxide (NO) and prostacyclin (PGl2) within skeletal muscle and therefore directly affects tissue vasodilation and blood flow. This is supported by research suggesting increased vasodilation and blood flow in response to intra-arterial infusion and exogenous administration of ATP. It can be speculated that these changes in blood flow may lead to an increased substrate pool for skeletal muscle by virtue of increased glucose and O2 uptake."[110]
In other words, ATP disodium can improve recovery by giving you a nice blood flow boost (and pump).
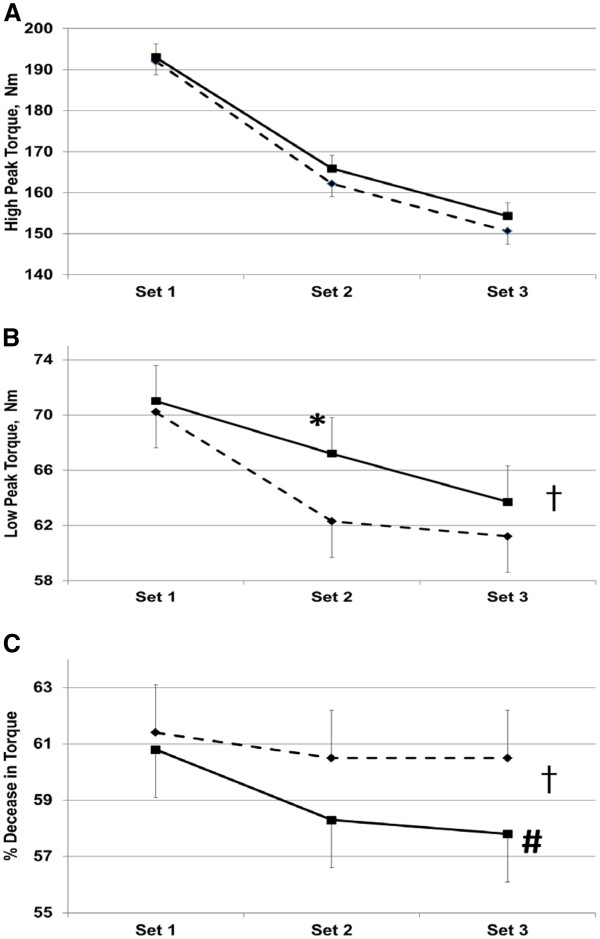
Torque during resistance exercise
Last but not least, let's briefly touch on a 2012 randomized, controlled study published by the Journal of the International Society of Sports Nutrition.[108]
In this study, subjects got either ATP disodium or a placebo. They took the prescribed treatment for 15 days, and at the end of the supplementation period, performed 3 sets of 50 knee extensions on a machine designed to measure the torque each participant produced during exercise.[108]
Study participants who took 400 mg ATP disodium for 15 days performed much better on 3 sets of 50 leg extensions than the placebo group.[108] "Low peak torque" is the lowest peak torque that each group was able to produce, on average, during the final 10 contractions of each 50 rep set.[108]
The group that received ATP disodium had much higher peak torque, and exhibited less fatigue than the placebo group.[108]
The big one: ATP drives vasodilation!
What's interesting about Peak ATP's pro-anabolic and performance-boosting effects is that they're observed in studies conducted over days or weeks, and the benefits seem to compound as time goes on.
At first glance, this seems counterintuitive. When it comes to the effects of intense exercise, it's easy to think of cellular energy supply as something immediately consumed and replenished— more of a short-term consideration than a long-term one.
But as we've written on the PricePlow Blog many times, blood flow is a crucial element of performance and recovery, and recovery can definitely affect your performance baseline in the long term.
Vasodilation leads to better circulation and tissue perfusion, thus enabling more efficient clearance of metabolic waste, and better delivery of crucial nutrients to hungry muscle cells. All of this can amplify the anabolic response to exercise.
Believe it or not, exogenous ATP can significantly improve cardiovascular function, and we think this probably has a lot to do with the benefits of consistent ATP disodium supplementation.
More to the point, discussing the vasodilatory effect of exogenous ATP can help us understand why it's such an awesome ingredient for a post-workout formula.
Let's kick things off with a direct quote from one of our cherished scientific references on ATP function:
Once released, ATP binds to purinergic (P2X and P2Y) receptors on endothelial cells. Binding results in the endothelial cells releasing nitric oxide via endothelial nitric oxide synthase, prostacyclin, and endothelium-derived hyperpolarizing factor, all 3 of which affect the smooth muscle of the vasculature via cyclic guanosine monophosphate, cyclic adenosine monophosphate, and hyperpolarization, respectively.[111]
This makes sense when you think about it – endothelial cells are no less in need of energy than any other type of cell. Supplying them with that energy in the form of exogenous ATP increases the likelihood that they'll successfully perform their physiological role, which is generating NO and triggering arterial vasodilation.
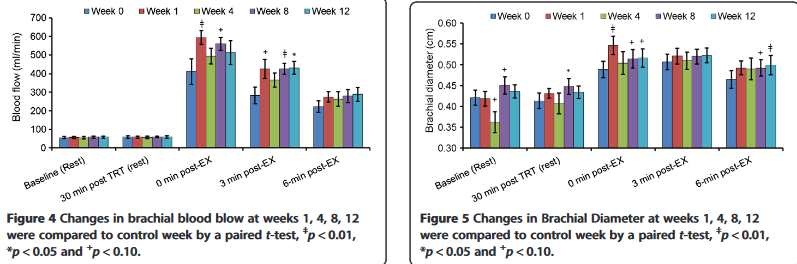
Ralf Jaeger study: Peak ATP enhances cardiovascular response to exercise
Remember Dr. Ralf Jaeger, the podcast guest we named in the introduction to this article? Well, he authored a study looking at the effects of Peak ATP on cardiovascular function.
In his study, subjects took 400 milligrams of Peak ATP for 12 weeks. Dr. Jaeger's team measured their response to exercise throughout the study period, and here's what they found:[111]
Twelve weeks of supplementation with Peak ATP caused cumulative cardiovascular benefits throughout the entire study period.[111]
Each time the researchers tested the study participants' cardiovascular response to exercise – at weeks 0, 1, 4, 8, and 12 – that response intensified as time went on.
This is evidence that the benefits of Peak ATP supplementation are cumulative – it's not only beneficial when taken immediately before exercise.
Exogenous ATP is used as a vasodilator in medical settings
In fact, medical science has known for quite a while that exogenous ATP is an effective vasodilator, even in people who aren't exercising at all. A 1999 paper explains that bolus injections of ATP are useful in the treatment of hemorrhagic shock, pulmonary hypertension, and paroxysmal supraventricular tachycardias, thanks to ATP's ability to improve cardiovascular function.[112]
ATP has even been used to induce low blood pressure for surgical purposes![112] Of course, low blood pressure isn't necessarily what we want from Peak ATP supplementation, but it just goes to show you the power of exogenous ATP's vasodilatory effect.
So while many think that this ingredient is for energy, and that's indeed one aspect, it's really for blood flow... and all of the benefits that come with it! You can learn far more in our article titled PEAK ATP: The Ultimate Guide to Disodium ATP Supplements.
Dosage and Timing
Normally, with creatine supplements, we say to take it anytime of the day that works for you, just get it in every day. However, with Peak ATP in the fold, we agree with Undefined Nutrition's labeling -- take it pre-workout to get the nitric oxide boosting, ATP-assisting effects when they're most useful.
If you're extra large, or in a greater hurry to get to creatine saturation, you can also take a scoop post-workout, especially if you just hit it really hard and want to clinically dose HMB when it's best.
Flavors Available
Structure launched in Berry Splash and Tropical Citrus flavors. It's good to know that Structure is naturally colored.
Conclusion
Structure from Undefined Nutrition is built on a very interesting formula. Although short, this list of ingredients is a reflection of cutting-edge, research-backed industry trends.
More and more supplement formulators are catching on to the fundamental biochemical mechanisms that underlie processes like muscle protein synthesis, recovery from exercise, and aerobic adaptation.

Will we see HMB replace BCAAs? Probably not, because the industry trend has been from BCAAs to essential amino acids (EAAs) – a more, not less, complete suite of amino acids.
But the trend to EAAs is something we see more in intra-workout formulas. Undefined Structure is a pre/post-workout muscle growth formula, and in these applications, HMB might make more sense because of the specificity in its mechanism of action.
Targeting the body's ATP supply with Peak ATP is another example – we've been harping on mitochondrial health for many years now, and there are tons of supplements out there that purport to improve mitochondrial function. But since the end result of mitochondrial function is ATP production, it might make more sense (at least in some situations) in practice to directly supplement with exogenous ATP now that the oral bioavailability problem has been solved with Peak ATP.
Stacking Peak ATP with creatine actually covers both bases because, in a nutshell, creatine works by improving mitochondrial function.
We're pretty interested to see how this formula does. Knowing Brian Shaw's faithful fans, they'd buy it no matter what. But now, after reading this, they can rest assured that the formula would be awesome even if he wasn't associated with it!
HMB has been around for a long time, but hasn't gotten much play recently. Maybe 2023 is the year it makes a comeback.
Undefined Nutrition Structure Creatine+ – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.










Comments and Discussion (Powered by the PricePlow Forum)