There are many reasons to get into the nutritional supplement game. Maybe you want more energy, or to sleep better, or to push yourself harder in the gym. But probably the number-1 most common reason we hear from our readers is body composition.
People want to get lean and stay lean while packing on the muscle – something that's not easy for most of us to do. It's not a huge surprise, to say the least, that any supplement that moves the needle in this direction tends to be popular with consumers.

We've long said that GlucoVantage dihydroberberine has 5x the bioavailability if traditional berberine. In this article, we explore the very well-designed study that demonstrated this.
Now let's talk about the holy grail of body composition supplements: berberine - a potent plant alkaloid that improves the body's insulin response so well that it outperforms popular pharmaceutical drugs.
But, to be a little more specific – dihydroberberine. Dihydroberberine is a better, patented[1] form of berberine from NNB Nutrition, sold under the name GlucoVantage.
GlucoVantage dihydroberberine: 5x the bioavailability?!
We've written about berberine and GlucoVantage dihydroberberine before, in our articles titled Berberine: The Best Glucose Disposal Ingredient Just Got Better and GlucoVantage: Dihydroberberine for Superior Insulin Sensitivity.
It's one of our favorite ingredients, because it works, and doesn't require high doses like traditional berberine does.
Dihydroberberine is a metabolite of berberine and was isolated and marketed to solve a specific problem – the relatively low oral bioavailability of berberine. Research has shown that it has 5 times the bioavailability of traditional berberine.[2] In this article, we're going to dig specifically into this study to explain how and why that'st he case.
This will help you understand how berberine works, and why dihydroberberine is more bioavailable than berberine. Before digging in, you can sign up for our news alerts on the ingredient so that you don't miss future research and product coverage:
Subscribe to PricePlow's Newsletter and Alerts on These Topics
Note: In this article, we introduce insulin sensitivity, glucose disposal, berberine's effects, and the dihydroberberine solution to berberine's problems. If you already understand these topics, you can click to skip to the research study discussion showing 5x better bioavailability.
Glucose Disposal and Why It Matters
For decades, the conventional wisdom has been that body composition is all about calories in, calories out (CICO). And while it's true that the amount of food you eat does matter, it's pretty clear by now that there's far more to the story. After all, the type of calories in can affect the amount of calories expended[3] -- these variables are never as static or simple as some tend to make them.
The insulin obesity hypothesis has gained a lot of ground in recent years, and is used to better explain our ongoing metabolic crisis. First, let's very briefly explain that we can consider insulin to be the "energy storage hormone". The pancreas secretes insulin when the body senses glucose in the bloodstream, signaling for the hormone to move the glucose into cells.[4] (We prefer it to go to muscle cells, but more on that later.)
With the insulin obesity hypothesis, the idea is that insulin resistance and sensitivity are key drivers of fat gain or loss. Put very simply, if you're insulin resistant (which means that your cells don't respond as strongly to insulin-signaling as they should), then you'll have a tendency to store carbohydrates as fat.[5]
A big part of the reason for this is that when your cells don't take up glucose in response to insulin, your body tries to compensate by producing even more insulin. Meanwhile, research has demonstrated that beta-oxidation (fat burning) significantly slows when blood sugar or insulin levels are elevated.[6,7]
Thus, fat burning is impaired when your insulin levels are elevated above baseline,[8] which naturally leads to a situation where your body fails to burn any fat for fuel. All the while, you try to feed your starving, energy-depraved cells by eating more and more. It gets metabolically "stuck" - poor at using the glucose available to it, while unable to burn the fat trapped in the body.
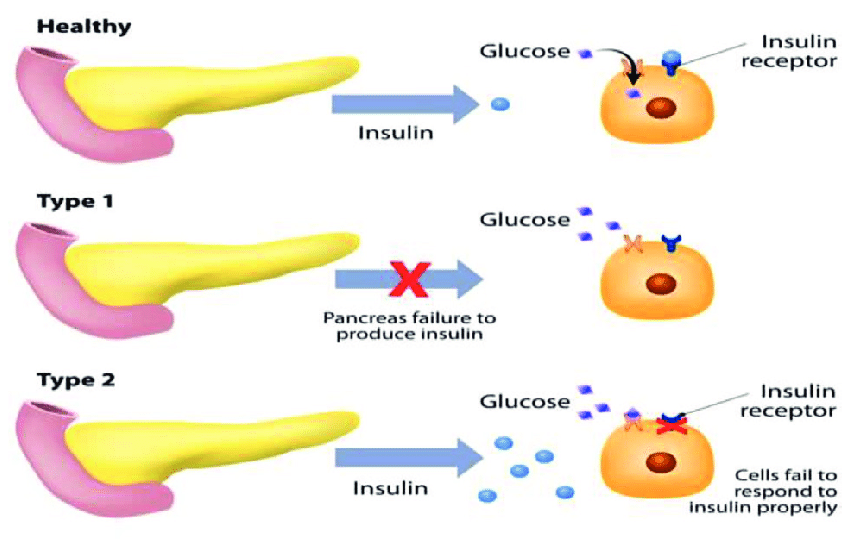
During insulin resistance, glucose builds up in your bloodstream because your cells can't take up glucose in response to insulin secretion. As a result, your blood glucose level rises and impairs fat burning.[9]
Over time, this can lead you to pack on some serious pounds, along with numerous diseases to follow the low-energy state.[10] It's a vicious cycle.
On the other hand, if you're insulin sensitive, then your body can put carbs where they belong, in muscle tissue[5] as glycogen or as energy for the anabolic response.[11] Your blood glucose and insulin levels stay under control, and your body burns some body fat for energy every day, as it should.
So on top of improving our diet, it'd be great if we had supplements that could make us more insulin sensitive, right?
As it turns out, we do – they're called glucose disposal agents, and berberine is one of them. For a while, we called it the best of them... until we learned about dihydroberberine. Let's explore, first getting into berberine itself:
Berberine: Discouraging Obesity Through Insulin Sensitivity
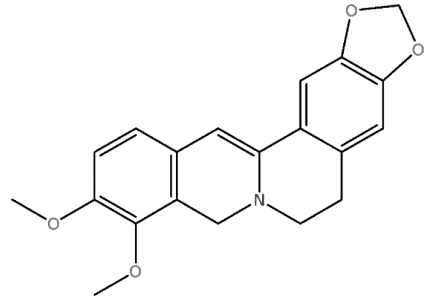
Berberine is an ammonium compound that's usually sourced from the Berberis family of shrubs. It has a long history of use treating metabolic disease in traditional Chinese medicine (TCM) and Ayurvedic medicine.[12,13]
Berberine improves glucose metabolism
Berberine increases whole-body insulin sensitivity, which is a fancy way of saying it can make all of your cells more insulin sensitive.
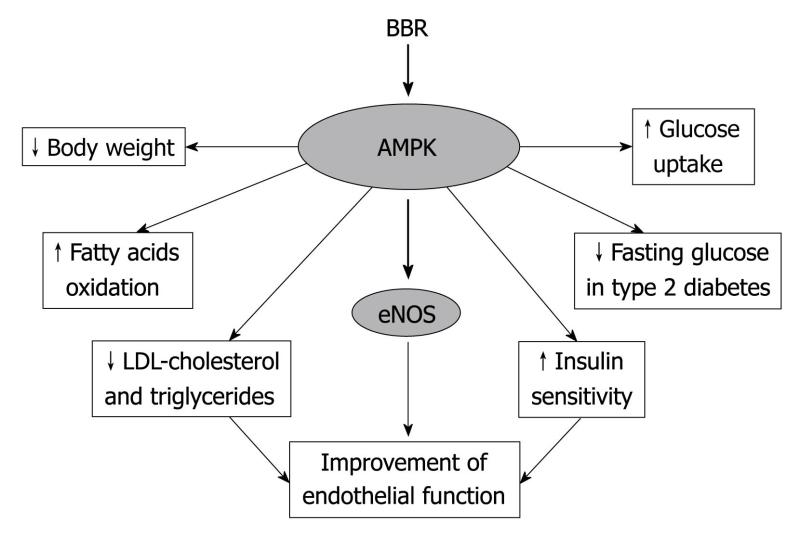
A diagram showing berberine's direct and indirect mechanisms of action. Although it's buried at the bottom of the chart, AMPK activation is what we're most concerned with, followed by adipogenesis downregulation.[14]
The upshot of higher insulin sensitivity is that, following a meal, your blood sugar peaks at lower levels. Also, your body produces less insulin to accomplish the job of getting glucose into your cells, where it can be burned as useful energy.[15-18]
Berberine does this by activating adenosine monophosphate kinase (AMPK), an enzyme that responds to certain signals (such as insulin) by shuttling nutrients into cells.[19] We often call AMPK the "we need energy now" enzyme for cells.
Berberine also prevents your body from making new fat cells
Additionally, berberine can downregulate a gene called proliferator-activated receptor-γ (PPARγ),[14] which has been known as one of the body's fat-storage master switches ever since it was discovered that when PPARγ was deleted in mice, they became totally devoid of body fat.[20]
Less PPARγ activity through berberine supplementation basically means that your body stores less energy as fat since shutting off the gene also turns off your body's machinery for creating new fat cells.[20]
The research on berberine supplementation: What it does
Berberine is possibly the most underrated supplement in the world. It creates a fantastic series of metabolic reactions that every carb-user should know about.
Research on berberine supplementation consistently finds that it not only increases insulin sensitivity throughout the body (but particularly in muscle tissue)[18] – it can also decrease glucose absorption,[21] positively affect the composition of gut microbiome, improve lipid metabolism,[16] and help control hepatic gluconeogenesis. The latter has been linked to insulin resistance and metabolic syndrome.[17,22]
Berberine also has anti-inflammatory and antioxidant properties,[21] both of which are crucial for metabolic health. Chronic inflammation, in particular, can eventually lead to type 2 diabetes and is associated with the onset of insulin resistance and metabolic syndrome.[23]
For a much longer discussion on how berberine works and why insulin sensitivity matters so much, check out GlucoVantage: Dihydroberberine for Superior Insulin Sensitivity.
So far, so good. But there are issues.
The Problem: Berberine’s Bioavailability
Thus far, berberine sounds awesome, and indeed, one study even points out that its ability to improve glucose metabolism is on par with that of metformin, a famously effective anti-diabetic drug.[24]
There's just one catch: Very large doses of berberine are required to achieve the therapeutic effects we're often looking for. In the same study we just cited, researchers had to give doses of 1.5 grams per day to study participants[24] -- three large capsules worth.
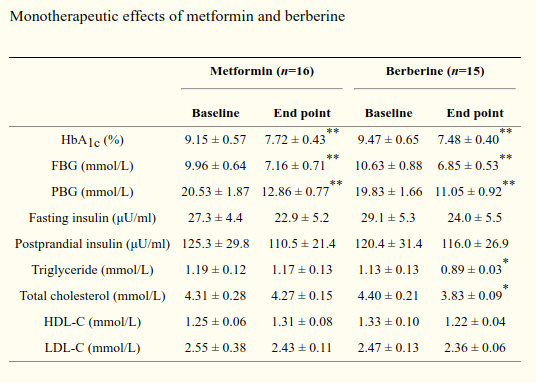
One could very easily argue that berberine outperformed metformin in most measures![24] But at this dose... GI upset can definitely occur. Let's see about an end-run to lower the amount of material taken.
Doses in this range reliably produce gastrointestinal upset, as the study authors had occasion to discover. They reported that about 35% of the subjects taking berberine had some kind of unwanted digestive symptoms.[24]
Another way of stating the problem would be: Berberine's bioavailability is too low to achieve the desired therapeutic effect with doses that are well-tolerated in the general population.
The Solution: Dihydroberberine
So that brings us to dihydroberberine (DHB), a patented metabolite of berberine[1,2] that is significantly more bioavailable than berberine itself.[2,25]
Dihydroberberine: A Better Berberine. This article focuses specifically on the higher-bioavailability berberine metabolite, but you can always go back and read our original berberine article to learn more about berberine itself.
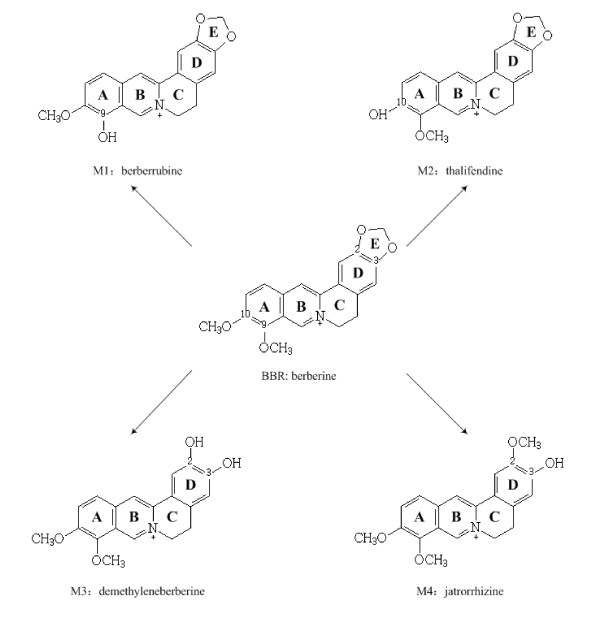
The basic reason for this is that dihydroberberine is already a part of your body's default berberine metabolism cycle – your gut flora actually converts berberine into DHB in order to get it absorbed into the bloodstream. After that, your body converts DHB back into berberine so that it can have the desired effect on your cells.[2]
Why does this cause gastrointestinal upset? Because the process of converting berberine into DHB is slow, meaning that when you take a big dose, a lot of unconverted berberine builds up and hangs around waiting to be converted into DHB. It's the backlogged, unprocessed berberine that seems to cause the GI distress.
Additionally, berberine exhibits low solubility in water, meaning that it's quite difficult for your intestinal cells to absorb it.[26,27]
Solution? Take dihydroberberine directly!
Skipping right a dihydroberberine / GlucoVantage based supplement provides a way to bypass that rate-limited conversion process -- and thus, greatly reduced risk of GI upset.
That's why dihydroberbine has five times the bioavailability of taking regular berberine.[2] It gets absorbed directly into your bloodstream, where your body can start converting it back into and utilizing the berberine.
DHB outperforms berberine
Dihydroberberine gets absorbed better and faster and then converts back to berberine in plasma anyway!
Research consistently shows that DHB does much better than berberine when it comes to improving body composition, blood triglycerides, and insulin sensitivity – and it does so at a much lower dose than berberine itself.[2,28]
So DHB causes fewer side effects than berberine,[2,28] and also helps reduce arterial plaque whereas berberine may not.[25] DHB also reduces cardiovascular inflammation to a much greater extent than berberine.[25,29]
It seems clear that dihydroberberine is simply the better option.
But let's dig a bit deeper to understand what's really going on under the hood when taking a GlucoVantage supplement.
Why GlucoVantage Dihydroberberine is 5x Better Than Berberine
The conversion "end-around" described above theoretically makes sense, but how do we know dihydroberberine outperforms berberine so well? To answer this question, we're going to get deep in the weeds on one particular study.
This study was conducted primarily in male Dewey Sprague rats by a team of researchers in 2015.[2] It was a follow-up to a 2008 study that concluded that dihydroberberine demonstrated improved efficacy over berberine "likely due to enhanced oral bioavailability", but diving into the exact mechanism wasn't in the scope of their research.[28] In this 2015 study, that was the exact intention.
The study that showed ~5x better bioavailability.[2] This study will be the topic of today's article.
Now ordinarily, we issue a disclaimer when applying the results of animal studies to humans, but in this case we're very confident that there is little difference between rat and human metabolism of berberine. Let's see why and how they approached that:
Methods: Experimentally mimicking the healthy human gut microbiome
The reason for this is that the researchers worked with bacterial strains isolated from the digestive tract of the rats, and all 14 of the strains named by the researchers, with the exception of perhaps one,[30] have been identified as a normal part of healthy people's gut microbiome.[31-40]
Four of the 14 strains – namely Lactobacillus casei, Lactobacillus acidophilus, Bifidobacterium longum, and Bifidobacterium breve – are recognizable to many of our readers because they're probiotic bacterial strains with a ton of research attesting to their beneficial effect on human health.[40]
Many of us have supplemented with one of these four strains before, or consumed them in lacto-fermented foods. So if your gut health is on point, you're almost certainly carrying one or more of them around right now.
How is the berberine to dihydroberberine conversion occurring?
The basic question motivating this study was, "What organ in the body is responsible for converting berberine to dihydroberberine?"
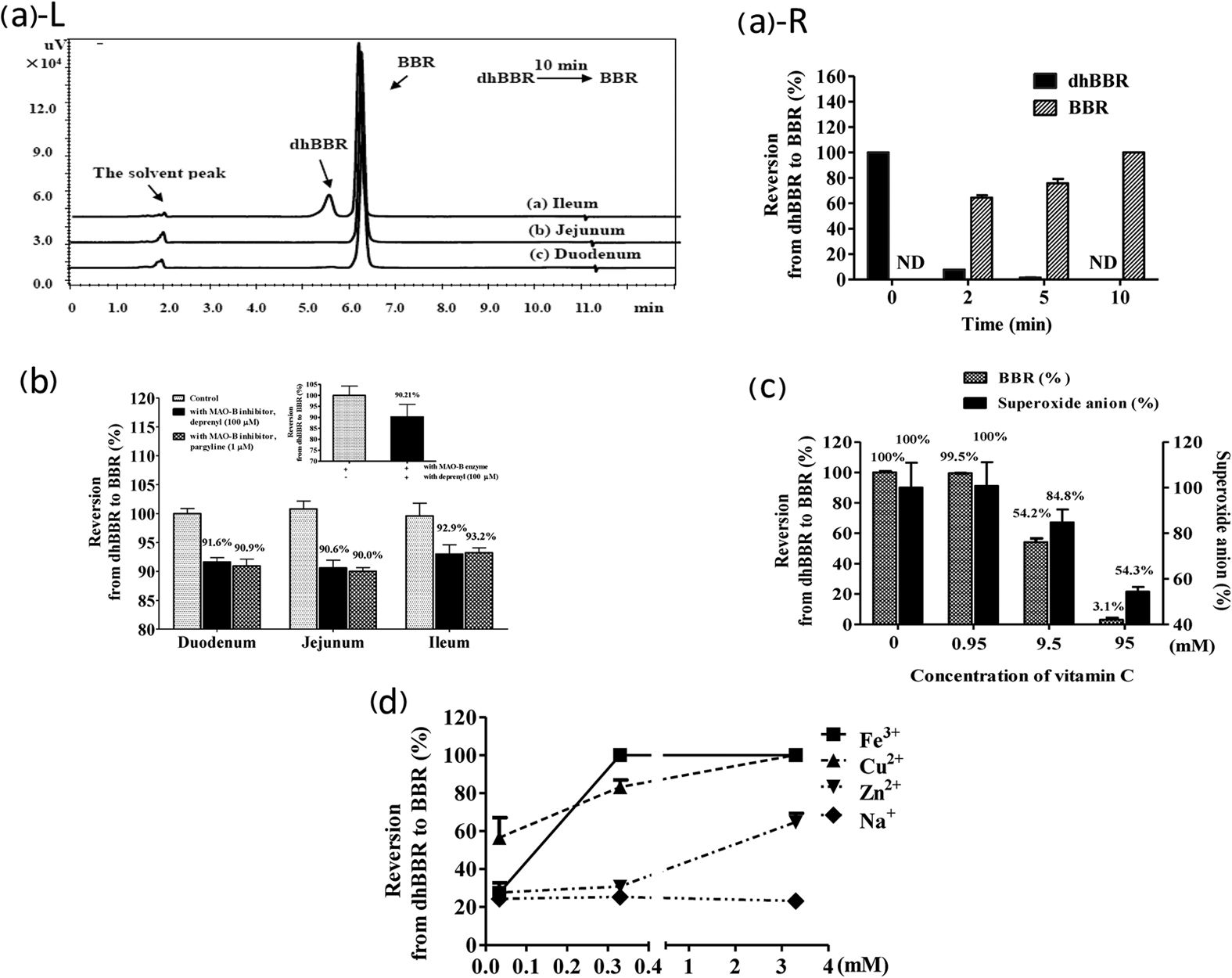
The first observation made by the researchers, which set up their subsequent experiments, was that high amounts of DHB were excreted in feces, even though it was not detected in bile or urine samples.[2]
They then administered berberine to the rats, and examined their organ tissue 24 hours later for signs of DHB. The finding was that DHB showed up in intestinal tissue, but not in any other organs.[2]
These two facts suggest an intestine-specific mechanism behind berberine-to-dihydroberberine conversion, so that's what the researchers set out to investigate.
Berberine-to-DHB conversion observed in bacterial cultures
Next, they isolated the 14 bacterial strains we discussed earlier, and applied berberine to the cultures. The idea was that if the isolated gastrointestinal bacteria failed to convert berberine to DHB, then they could be discounted as the "organ" responsible for DHB conversion.
The result: All 14 of the isolated strains did convert berberine to DHB![2]
The obvious conclusion to draw is that intestinal microflora are the "organ" responsible for converting berberine to DHB – but this is science, so we need to subject that theory to a bit more examination before seriously entertaining it.
Pre-treatment with antibiotics significantly reduced berberine to DHB conversion
So if intestinal bacteria are driving berberine to DHB conversion, then it seems logical that killing off intestinal bacteria should reduce the amount of DHB produced.
That's what the researchers set out to test next.
They pre-treated the rats with antibiotics, which reduced the bacterial flora population of their intestine by "two logs".[2] (Two logs here means two factors of 10 – i.e. 100 times.) So there were 100 times fewer bacteria than usual after antibiotic pretreatment.[2]
This created what's called a pseudo-germ-free (PGF) environment in the rats. "Pseudo" indicates that they aren't really germ free – there were tons of bacteria before antibiotic treatment. It's impossible to kill all the bacteria in an animal's gut, and populations will eventually rebound after antibiotic treatment is finished. But it's close enough to germ-free, since the vast majority of microbes have been killed off, to be consistent with the results of truly germ-free animals, which cost much more to produce.[43]
Upon the conclusion of three days' antibiotic pretreatment, the rats were administered a hefty dose of berberine. Then the researchers collected the rats' feces and analyzed the samples for another three days.[2]
The result was that the rats who had not been treated with antibiotics produced 3-times as much DHB as the PGF rats did.[2]
Another interesting thing to note is that the pseudo-germ-free rats also excreted much more unconverted berberine in their feces than the antibiotic-free rats. This is consistent with what we'd expect to see when berberine is converted into DHB.[2]
The berberine paradox: those who need it most, metabolize it the worst
This teaches us something we discuss in the conclusion, but must mention now -- berberine metabolism requires great gut health, but those who need berberine the most (ie the metabolically dysfunctional and insulin resistant) most commonly have poor gut health.[44] This is yet another reason to go straight to dihydroberberine!
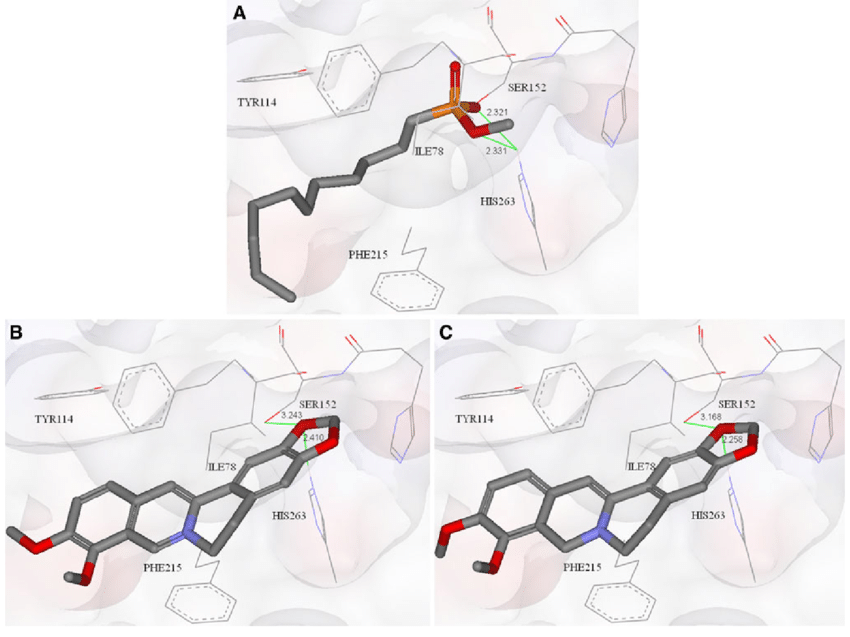
Berberine has a high affinity for nitroreductase, a key digestive enzyme
Now that we can see the bacteria are converting berberine into DHB, we might ask how they're doing this. The answer is that these bacteria produce key digestive enzymes, like nitroreductase and azoreductase, both of which are also found in the human digestive tract,[45,46] that help convert ingested nutrients into usable metabolites.
To test the idea that these enzymes could be driving berberine to DHB conversion in mammalian intestines, the researchers tested berberine's affinity for nitroreductase. They found that this affinity is high, which gives us some more insight into how exactly berberine metabolism is taking place.[2]
In fact, the researchers actually incubated berberine with just nitroreductase, and found that the enzyme alone was capable of generating detectable levels of DHB after four hours.[2]
Furthermore, adding a nitroreductase inhibitor to this culture prevented the conversion of berberine to DHB![2]
So it seems pretty clear that nitroreductase is the tool that your digestive bacteria are using to create DHB from berberine.
DHB is converted back into berberine before absorption into the blood
OK, so we can make lots of dihydroberberine from berberine using healthy gut flora.
That's great, but is taking DHB directly really going to give us the same benefit as berberine? After all, it's not the same molecule. Its effects might be different and maybe other metabolites are involved elsewhere.
This isn't a concern because as the study authors found, DHB gets converted back into berberine after it's absorbed into the bloodstream.
Their method for demonstrating this was simple: After giving their rats a bunch of straight DHB, the study authors measured the rats' berberine and DHB blood plasma levels. Their finding was that berberine levels rose, but DHB was almost undetectable.[2]
This suggests that a total conversion of DHB back into berberine occurred in the intestinal wall.[2] If you take DHB, the body ultimately gets to the same destination, but with less work and less waste!
Here's what the study's authors stated (dhBBR is dihydroberberine and BBR is berberine):
The findings suggest that a nearly complete reversion of dhBBR into BBR most likely occurred in the well of the intestine, resulting in a low level of dhBBR and a high level of BBR in blood. The absorption rate of dhBBR (200 mg/kg, oral) was then compared with that of BBR (200 mg/kg, oral). As shown in Fig. 3c, the blood level of BBR in the dhBBR-treated rats exhibited AUC(0-t) and Cmax values that were 4.8- and 3.25-fold higher than those of the BBR-treated rats, respectively, indicating a higher intestinal absorption of dhBBR as compared with that of BBR.[2]
Figure 3c is shown below:
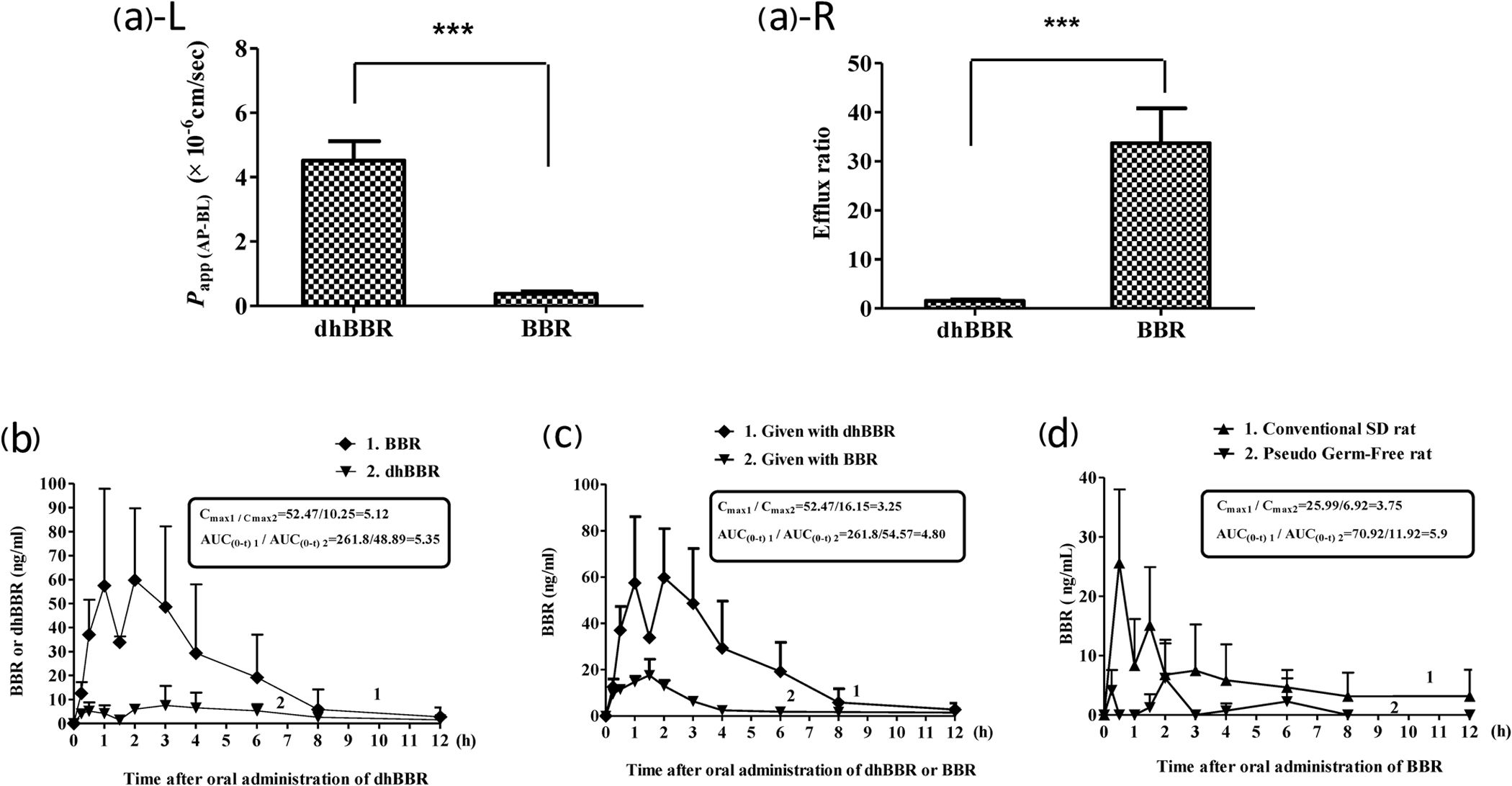
Simply put by the researchers: "DhBBR [Dihydroberberine] has a better intestinal absorption than BBR."[2]
Thus, the AUC, or area under the curve, led to 4.8 times more berberine in the blood over time, and a 3.25 greater amount at its peak. This means it not only worked faster and stronger, but longer as well. The researchers round up a bit and write "5-fold" in the article.[2]
Bacterial conversion of berberine to DHB drives berberine absorption
If absorbing berberine depends on converting it to DHB and back again, and this conversion process is initiated by intestinal bacteria, then it stands to reason that if the intestinal bacteria can't do this, the host won't be able to absorb berberine at all.
Meet Tributyrin: The Gut Health Optimizer that generates the critical short chain fatty acid, butyrate. As we can see, gut health is important if you take standard berberine. We opt for dihydroberberine, though.
To test this, the researchers went back to their pseudo-germ-free (PGF) rats – the ones whose intestinal bacteria had been substantially killed off with antibiotics beforehand – and gave them regular berberine. Then they measured the PGF rats' blood levels of berberine.
They found exactly what we'd expect. The rats with impaired microflora showed very little change in berberine blood levels in response to oral berberine supplementation.[2]
This was further illustrated in another experiment where the researchers took diabetic mice and divided them into two groups, only one of which got the PGF antibiotic pretreatment. Both groups were given berberine.
In theory, the diabetic PGF mice should show less of an improvement in glucose metabolism than the control mice, because without healthy gut flora to convert berberine into DHB, they should absorb less berberine than the control mice.
And that's exactly what the researchers found – the PGF diabetic mice responded less to berberine treatment than the non-PGF mice with diabetes.[2]
Conclusion: Dihydroberberine - The Brilliant Berberine End-Run
The big takeaway from all this is that the efficacy of berberine for any given person will depend largely on their gut health.

The effective Dihydroberberine Dosage is 30% the dose of standard berberine, giving it far more applications and less GI discomfort!
That matters a lot, because the population most in need of glucose disposal agents like berberine – type 2 diabetics – is also at great risk of having gut flora disturbances.[44]
In fact, many researchers now believe that impaired gut microbiome health is one cause — perhaps even the primary cause — of insulin resistance and diabetes onset.[47,48]
It seems pretty clear that a lot of prediabetic or diabetic people, turning to a metformin-caliber supplement like berberine for relief, could end up disappointed as their messed-up gut flora will prevent them from absorbing enough of it to achieve the desired therapeutic effect.
The reason we like dihydroberbine GlucoVantage so much is not just that it causes fewer side effects than berberine, which it does. It's more that dihydroberberine is a brilliant metabolic end-run around the gut flora problem – by supplementing with DHB directly instead of relying on your gut flora to convert berberine into DHB, you're bypassing any potential issues caused by your gut flora composition.

GlucoVantage from NNB Nutrition is a pure form of Dihydroberberine (DHB) and is known as "The Super Berberine".
But more importantly: We want our readers to understand how crucial it is to keep your gut flora in prime condition. This isn't the place for that discussion, but you can see some of the background of healthy gut function in our article titled Tributyrin: The Gut Health Optimizer, which describes a process and ingredient that may help.
Yes, supplements like DHB can go a long way toward improving metabolic health. But as they say, an ounce of prevention is worth a pound of cure. Get enough exercise, eat lacto-fermented foods, avoid toxic gut-disrupting processed oils,[49] and feed your gut flora tons of prebiotic fiber – keep them happy and you might avoid needing a glucose disposal agent altogether.
But when you do want a glucose disposal agent to drive those carbs into muscle tissue - if we once called berberine the king, then GlucoVantage dihydroberberine is the emperor.
Alpha Lion Gains Candy GlucoVantage – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.


Comments and Discussion (Powered by the PricePlow Forum)