Note: This is part one of a three-part series on cholesterol, heart disease risk, and the start of my personal journey towards health optimization via food and dietary strategy.
On March 8, 2019, I made a post on social media (Instagram, Facebook, Twitter) explaining that after a dietary change, I was feeling better than I'd felt in 10 years, and at age 37, was ready to begin a public journey to find the most optimal diet.
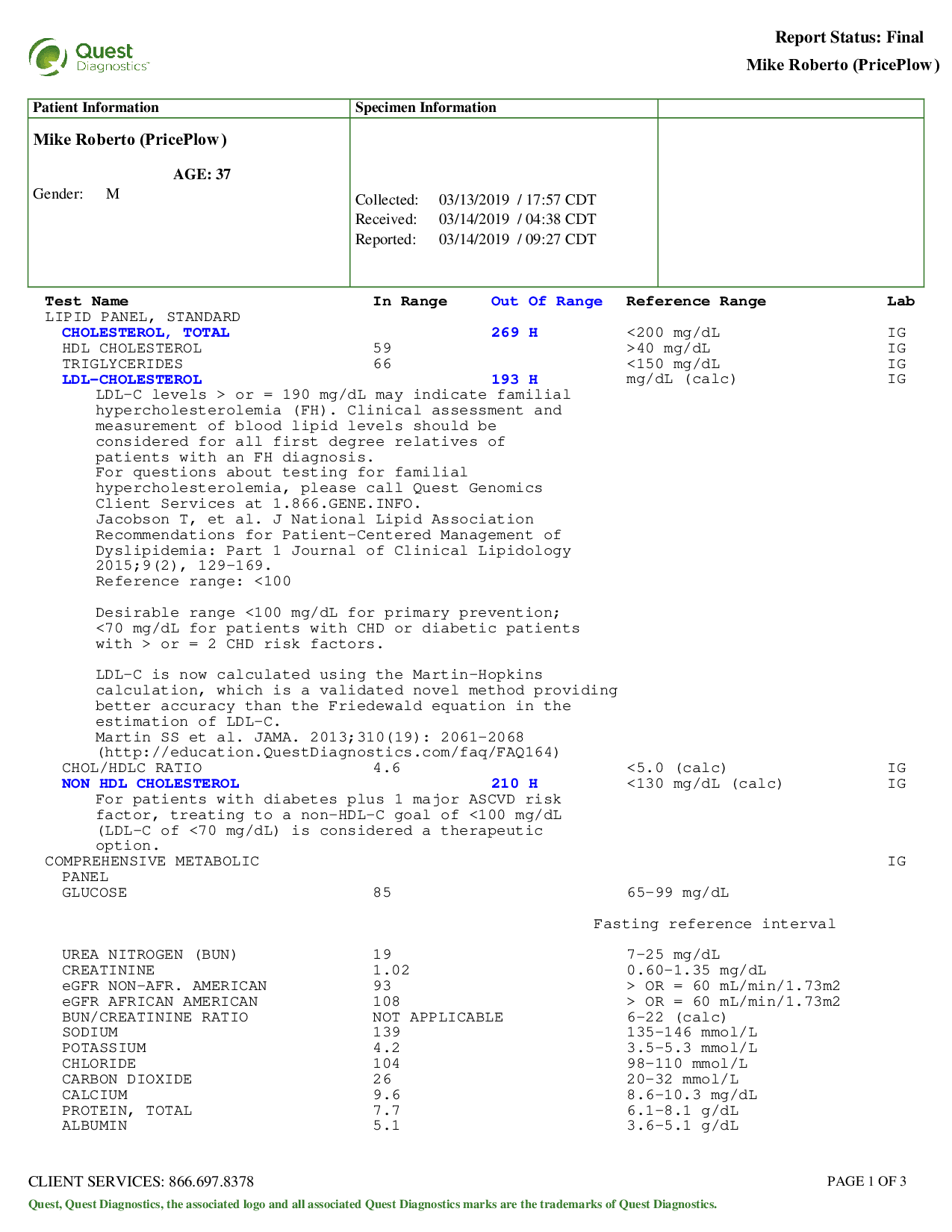
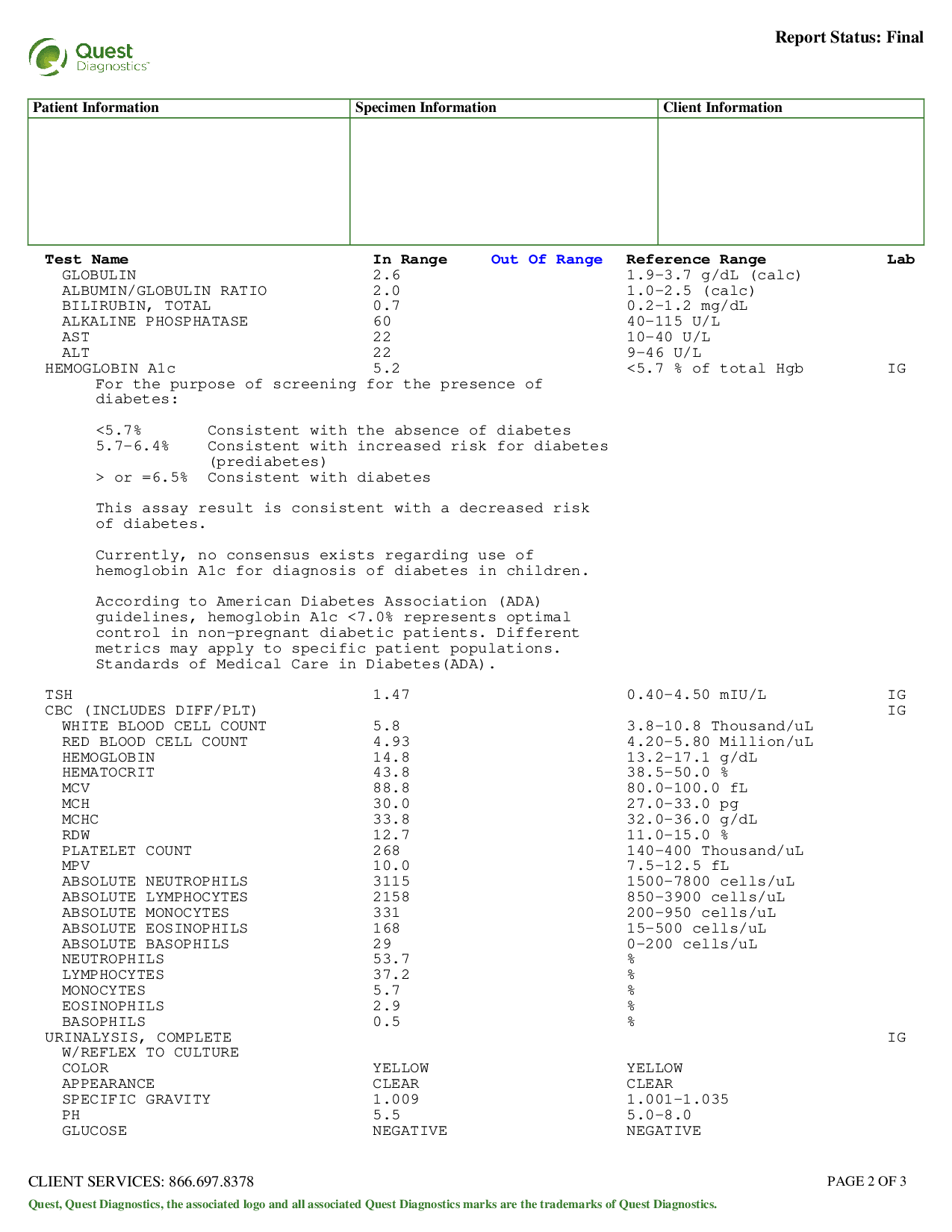
Part of this journey is to show my blood work, so I took advantage of my annual free physical.
Attached are the results:
My blood test results, March 13, 2019:
I was given a general lipid panel, which will be the focus of this post. The relevant numbers:
- Triglycerides: 66
- HDL: 59
- LDL: 193
- Total Cholesterol: 269
- Non HDL: 210
- HbA1c: 5.2
Known Ratios of Interest:
- Chol/HDLC: 4.56 (want to be under 4.5, 4.0 is even better)
- TG/HDL: 1.12 (want to be under 2.0, 1.2 even better)
OMG, LDL-C is high! Fire up the statins!!
I received the following message from the technician:
"LDL cholesterol in range for statin therapy. Needs to come back in to discuss labs and treatment options."
Well they didn't waste any time there. Based upon a single number at a single point in time, it's time to discuss the initiation of a lifetime of drugs. What happened here?
Watch the video while you read
Before going further, if you'd like to watch on YouTube instead of read this, see the video below, as I detail the same story:
Meet the Lipid Hypothesis
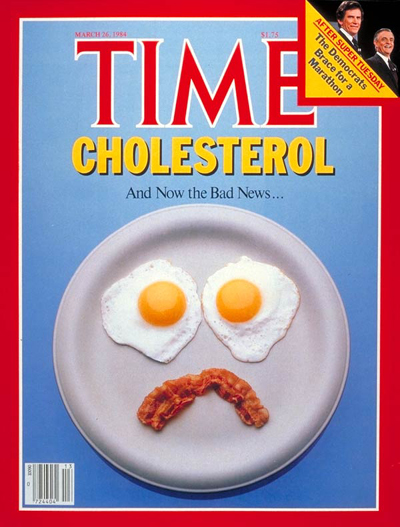
You've probably seen the following image, which Time Magazine published in 1984:
It really started a bit earlier, in 1976, when a study commented that "measures used to lower the plasma lipids in patients with hyperlipidemia will lead to reductions in new events of coronary heart disease".[1] But the situation got really out of control when Time Magazine published the above issue after the 1984 Coronary Primary Prevention Trial (CPPT) showed that "decreasing blood cholesterol... significantly reduces coronary heart disease".[2,3]
Confusing drugs with food with blood levels
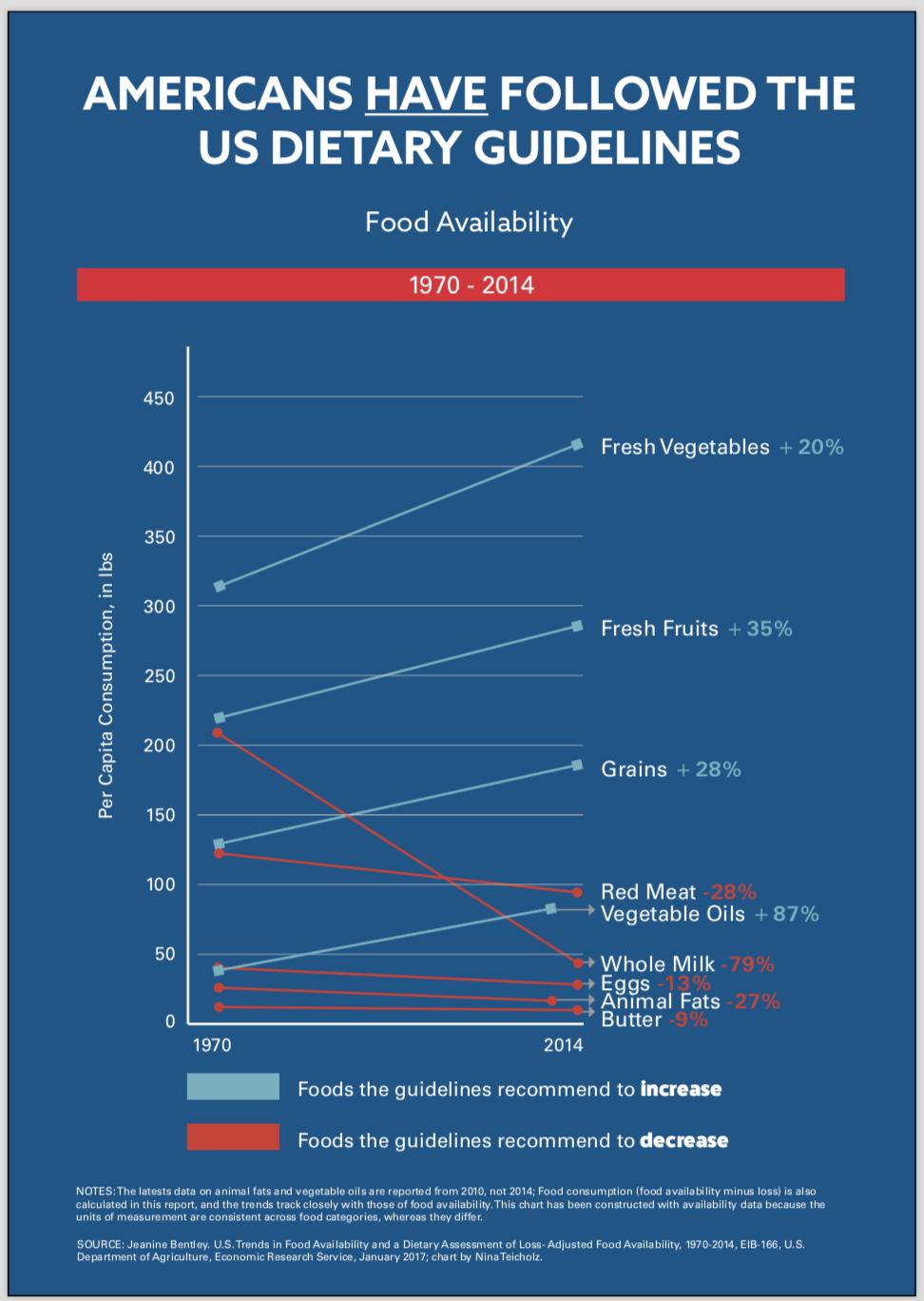
Americans did listen to the food guidelines.. and we got sicker and fatter than ever. Are we sure red meat and cholesterol are really the issue?!
Realize that Time Magazine made a massive (and potentially purposeful) mistake in confusing the lipid hypothesis -- that high cholesterol levels lead to more heart disease -- with a drug intervention. But worse, they connected that drug intervention with food, even though changes in dietary cholesterol only make minor changes in blood cholesterol,[4] especially compared to other dietary changes such as altering carbohydrate intake.[5,6]
Further, that original 1984 drug trial (done using a drug known as cholestyramine) didn't even significantly reduce mortality![2]
But it didn't matter. The magazine ran it, villainizing eggs and red meat, a massive and world-changing media-scare ensued, and that was that. All cholesterol was now bad. You were told to eat less of it, your total cholesterol would decline, and you would be less likely to suffer from heart disease.
America listened... and America got sicker.
But high cholesterol makes healthy people live longer...
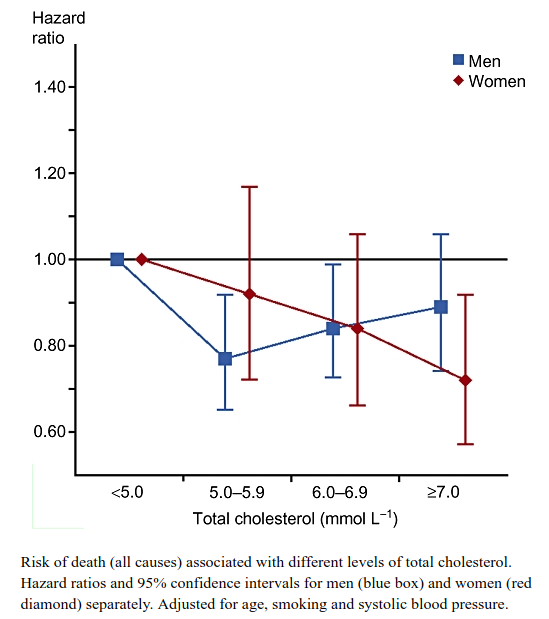
Why are individuals with higher total cholesterol dying slower?! Perhaps it is actually protective or responsive to other problems?![7]
Meanwhile, there was this pesky problem: once you factor for smoking, age, and other confounding risk factors, it keeps turning up that higher total cholesterol leads to less mortality![7,8] Whoops!
So maybe LDL is the problem...
But that's OK, because now there's data showing that LDL cholesterol is the bogeyman! LDL is what's considered the bad cholesterol.[9] If you split the world in half, then the high LDL group is slightly more likely to face heart disease. Time to lower it (and conveniently, we have drugs for that).
Initiate 50 years of drugs?
But is that reasonable? Can you really just look at one number, at one moment in time, and start doling out drugs? I'm 37 years old -- are you just going to drug me for 50 years?! Might the other markers matter?
It turns out that those markers do matter, and in a major way.
When LDL Cholesterol is meaningless
If you aren't familiar with blood work, I have a slightly unique lipid profile that's different from many others with high LDL:
- My triglycerides are low
- My HDL Cholesterol is high (this is indeed the "good cholesterol")
- I am relatively lean and athletic
- My HbA1c is in a very healthy range (5.2)
Effectively, all known numbers are very good except for the one that doctors can easily treat. Am I really at risk for heart disease or early death? High LDL might a slight risk factor for some at-risk individuals (ie those with high inflammation levels),[10] but what happens when you compare it to the strength of the other risk factors?
So let's see what the major research studies have to say when you actually tease out this demographic, especially when they're not on drugs:
-
The Framingham study destroys the LDL notion for many
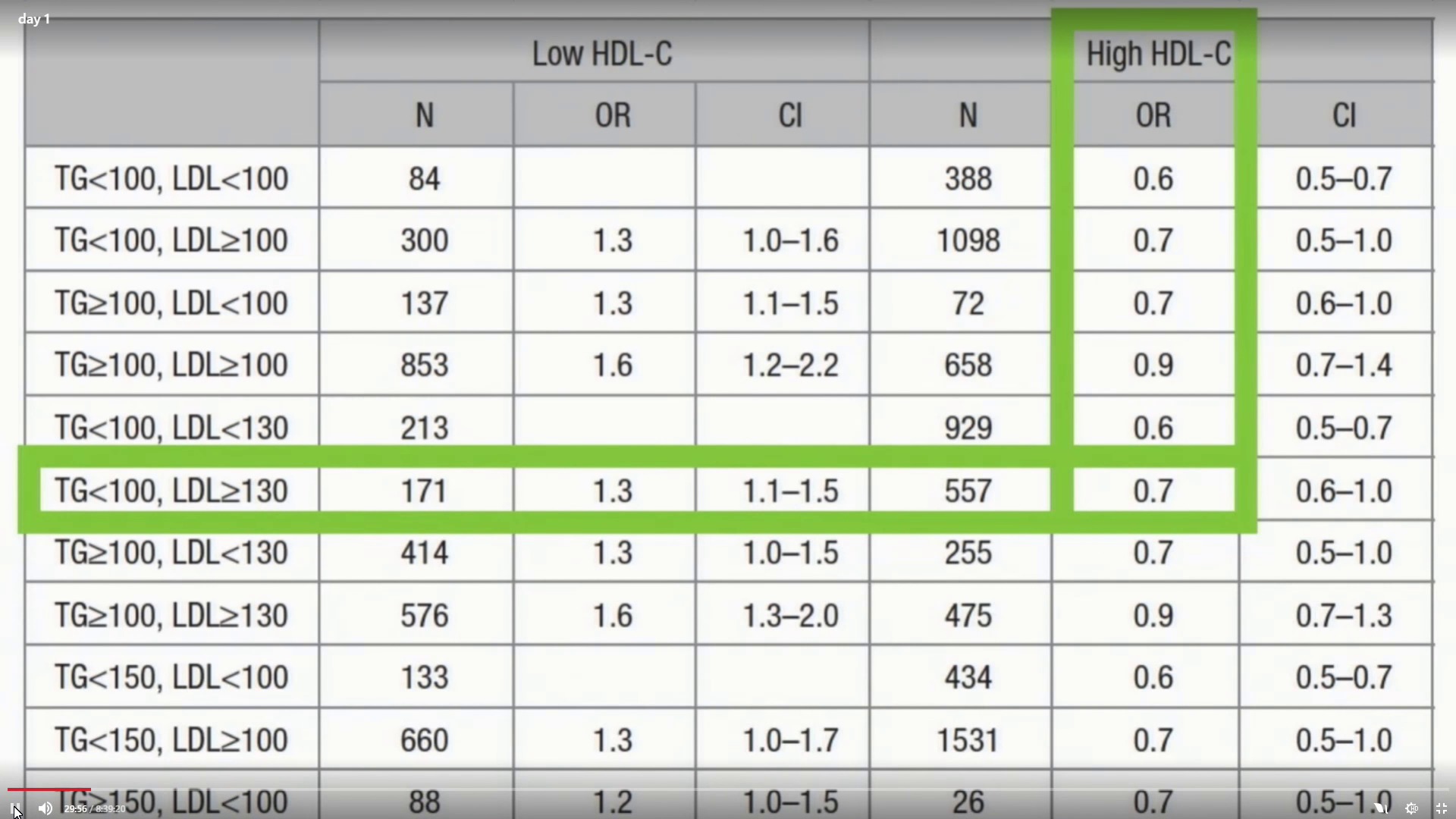
After ten years of monitoring 52,087 Norwegians (ages 20-74), The Framingham Heart Study had a massive amount of data on subjects -- and they were able to exclude anyone receiving lipid medication. Look at what their data showed:[11]
The Framingham Study showed that HDL is the real risk factor, followed by triglyceride. A hazard ratio of 1.0 represents an equal risk between groups. Below 1.0 is less risk, greater than 1.0 is greater risk. At 0.7, my profile suggests less risk than nearly everybody!
If your triglycerides are under 100 (check), your HDL is high (≥40 in men) (check), and LDL is greater than 130 (check), you are LESS LIKELY to get cardiovascular disease!! You can tell this because the OR, or Odds Ratio, is below 1.0, meaning you are less likely to be affected. In fact, there are only a few groups with better risk profiles!
It's the HDL, my drug-dealing doctor
Who's above 1.0, indicating higher risk of disease? The low-HDL groups! Look at the data -- heart disease risk high for low-HDL, heart disease low for high HDL. LDL nearly meaningless in comparison. We'll get into this later, but it turns out that low HDL is a far stronger risk factor than high LDL.
Further, there's another study showing similar risk results:
-
Study Tracking 103,000+ Subjects: LDL not the problem
In 2015, a monstrous study that tracked 103,646 50-75 year old subjects for 8 years was published.[12]
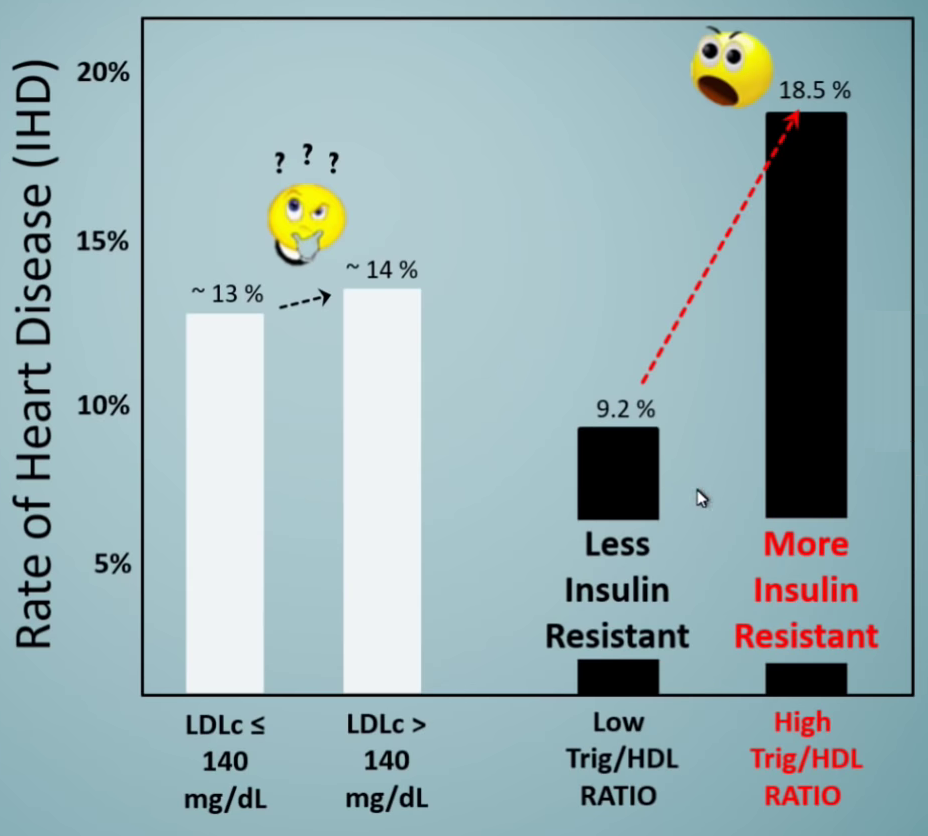
When dividing only by LDL-C, with the low group ≤ 140 and the high group > 140, 13% of the low LDL individuals got ischemic heart disease, while 14% of high LDL got it.
That's simply not significant. Are we sure this is the bogeyman we've made it out to be? What more is happening here?
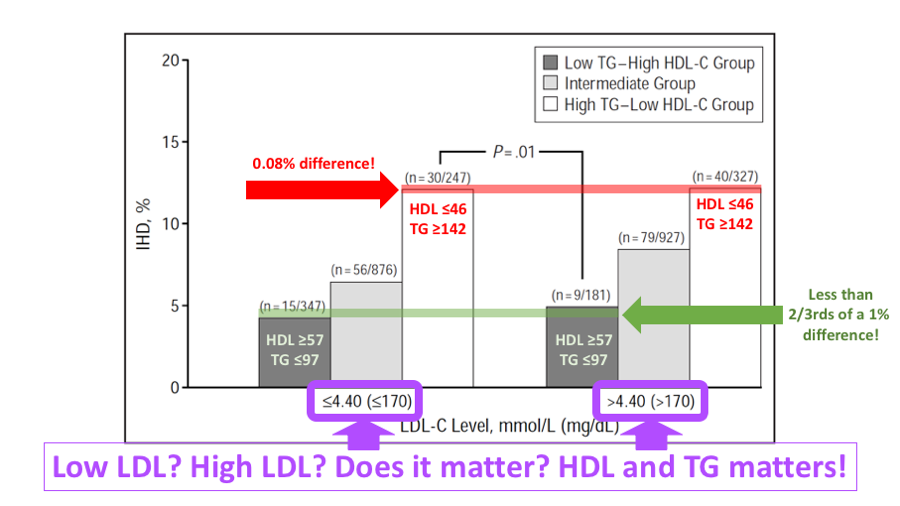
Far more powerful: Triglycerides / HDL ratio
High LDL has nothing compared to higher triglycerides paired with lower HDL,[12] a general marker for insulin resistance. Annotations courtesy Ivor Cummins.[13]
In this study, HDL was once again more powerful. But even stronger than that, the best odds are if you have a Low Triglycerides to HDL ratio, which yielded 9.2%. Compare that to the higher trig/HDL group which had 18.5% disease incidence - twice as many individuals. That is significant. LDL is not.
What's so special about this ratio vs. LDL alone? We discuss that a bit more below, but the quick rundown is that a high Trig/HDL ratio represents insulin resistance, the true problem with our collective metabolic crisis.
-
Meanwhile in China...
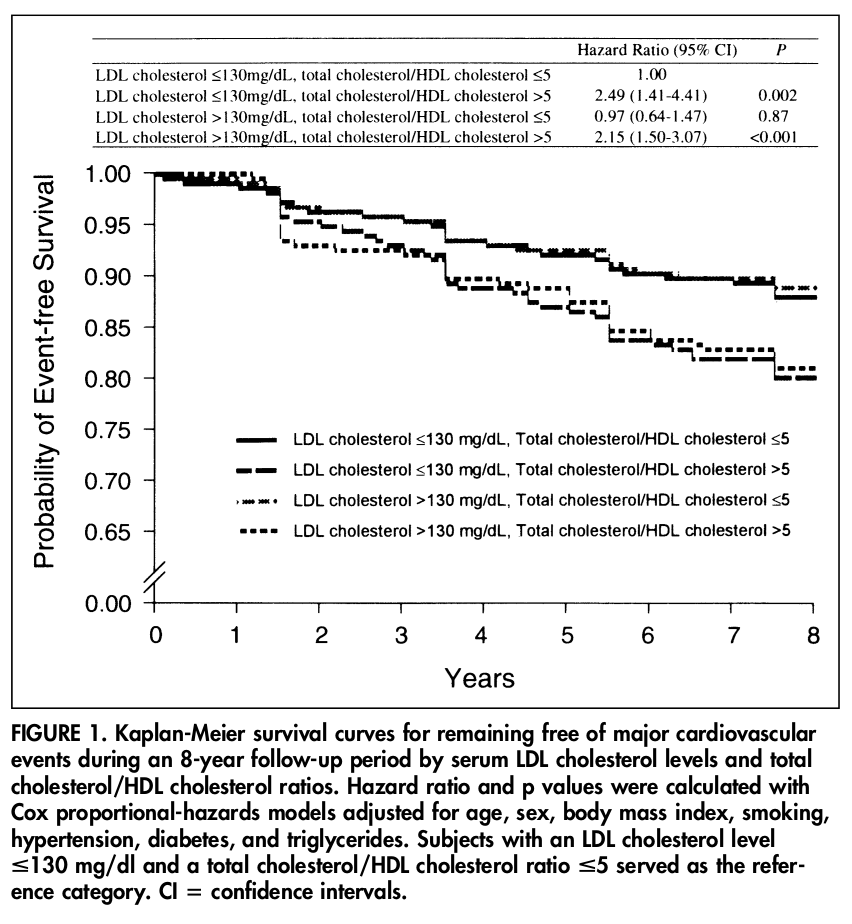
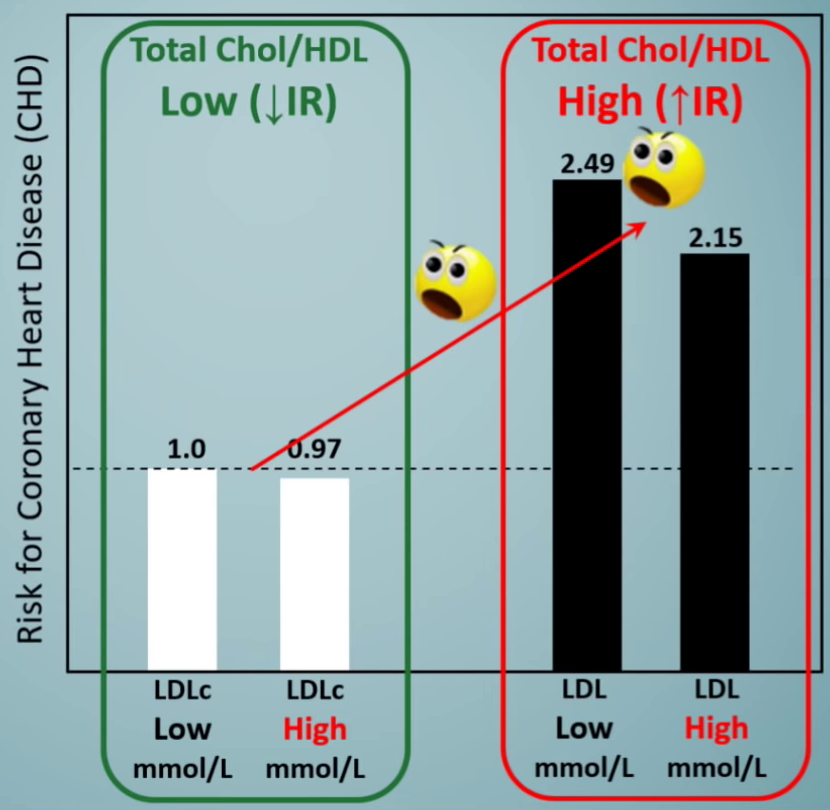
What's this?! The group with higher LDL but a good (lower) total cholesterol / HDL ratio had less heart disease!![14]
Another eight-year study came out of China in 2001 (isn't it crazy we've had this data for so long?),[14] showing that when splitting low LDL-C and high LDL-C at 130mg/dL (and removing subjects on lipid-lowering drugs), the risk for coronary heart disease for the low LDL group was 1.0, and the high LDL group was 0.97, meaning a slightly lower risk.
HDL strikes again: Stratify by Total Cholesterol / HDL
The China study took it a step further. The data above is only for participants with a low total cholesterol to HDL ratio, which indicates little-to-no insulin resistance. What happens with high total cholesterol to HDL groups (meaning HDL is too low, or not enough to make up for a high total)?
This is where the real trouble is! In that group, you'll get two risk multipliers of 2.49 and 2.15 - far worse than the above group with lower insulin resistance!
And even crazier? If you break that group in half by LDL, the high LDL group has the lower risk! High LDL, high total cholesterol / HDL is the group with 2.15 whereas low LDL, high total cholesterol / HDL is 2.49.
Another way of looking at the above data, as annotated by Ivor Cummins.[13] The higher LDL groups actually had less heart disease within their sub-groups, but that wasn't the real story. Ivor further demonstrates that a high total cholesterol to HDL ratio is indicative of insulin resistance, the real culprit. This is discussed in Part 2 of this series.
Lesson learned? LDL alone is basically useless.
In this study, the cutoff between these two groups (total cholesterol / HDL) was 5.0. Recall that my lab test showed 4.56 - part of the low group.
Of the four bars represented above, I am in the lowest risk one. Again, are we sure I'm the one who needs to be drugged up?
-
How about one more observational, non-drugged study? Jeppesen 2001
In 2001, Jeppesen et al published an observational study of 2906 men aged 53 to 74 years free of heart disease at baseline.[15] They followed subjects for eight years, and 229 unfortunately developed ischemic heart disease.
Here, they stratified the data similar to the above, and flat out came to the following conclusion:
Men with conventional risk factors for IHD have a low risk of IHD if they have low TG–high HDL-C levels.[15]
That "conventional" risk factor being LDL, with groups separated at 170mg/dL.
The left three bars represent the low LDL group. The right three bars represent the high LDL group.[15] Are we sure we've pegged the right marker to vilify?! Annotations courtesy Dave Feldman[16]
HDL and Triglycerides at it once again
Once again, there's nearly no difference between high and low LDL groups!! However, your HDL and Triglycerides tell a huge story. The higher HDL (≥ 57), lower triglyceride group (≤97), which is the group where I reside is basically the same between the two LDL groups, and these are the two least-risky places on the chart.
You get the point: LDL on its own is useless.
What's this mean? According to data expert and cardiologist Dr. William P. Castelli, who ran the Framingham study (and wrote a thorough analysis about its data), LDL is a dependent variable![17] It's not a primary means of diagnosis, and it should not be treated as such without looking at everything else. He went on to say that
"Unless LDL levels are very high (300 mg/dl (7.8 mmol/l) or higher), they have no value, in isolation, in predicting those individuals at risk of CHD."
-- Dr. William P. Castelli, Director of the Framingham Heart Study
New research continues to demonstrate this into 2019,[18] but it will take more time to beat this into the minds of the populace.
This is why most risk calculators (which we'll discuss in Part 2 of this series) don't even use LDL as an input! But the repressed doctors who are forced to discuss statins usually don't show you that.
We are looking for causes... not weak associations
Association is not causation. The associations of cardiovascular disease seen with LDL are far weaker than the other factors discussed here and in the next part of this series, and the cholesterol hypothesis is unable to satisfy common criteria for causality.[19]
By the way, you can fudge an LDL test in three days... by eating garbage
Here's a simple fact: there is not a single study on non-drugged individuals showing that the combination of high LDL, low triglycerides, and high HDL ever leads to more heart disease.
Here's what's even crazier. A scientist and cholesterol expert named Dave Feldman found himself in a similar (but more extreme) situation as myself after going on a ketogenic diet. He wondered how bad things could be -- after all, he felt better than ever, something typical to well-adapted low-carb dieters. Was LDL really the problem?
Dave began digging through the research, and started finding the patterns discussed above, where LDL had nothing to do with anything, given his other numbers.
But that wasn't enough for Dave. He began getting countless blood tests. And he started tinkering with his diet. And he found something spectacular.
Dave noticed that if he went on a "prison diet" of just white bread and processed meat -- something most of us would agree doesn't sound too healthy -- he could tank his LDL within a matter of days.
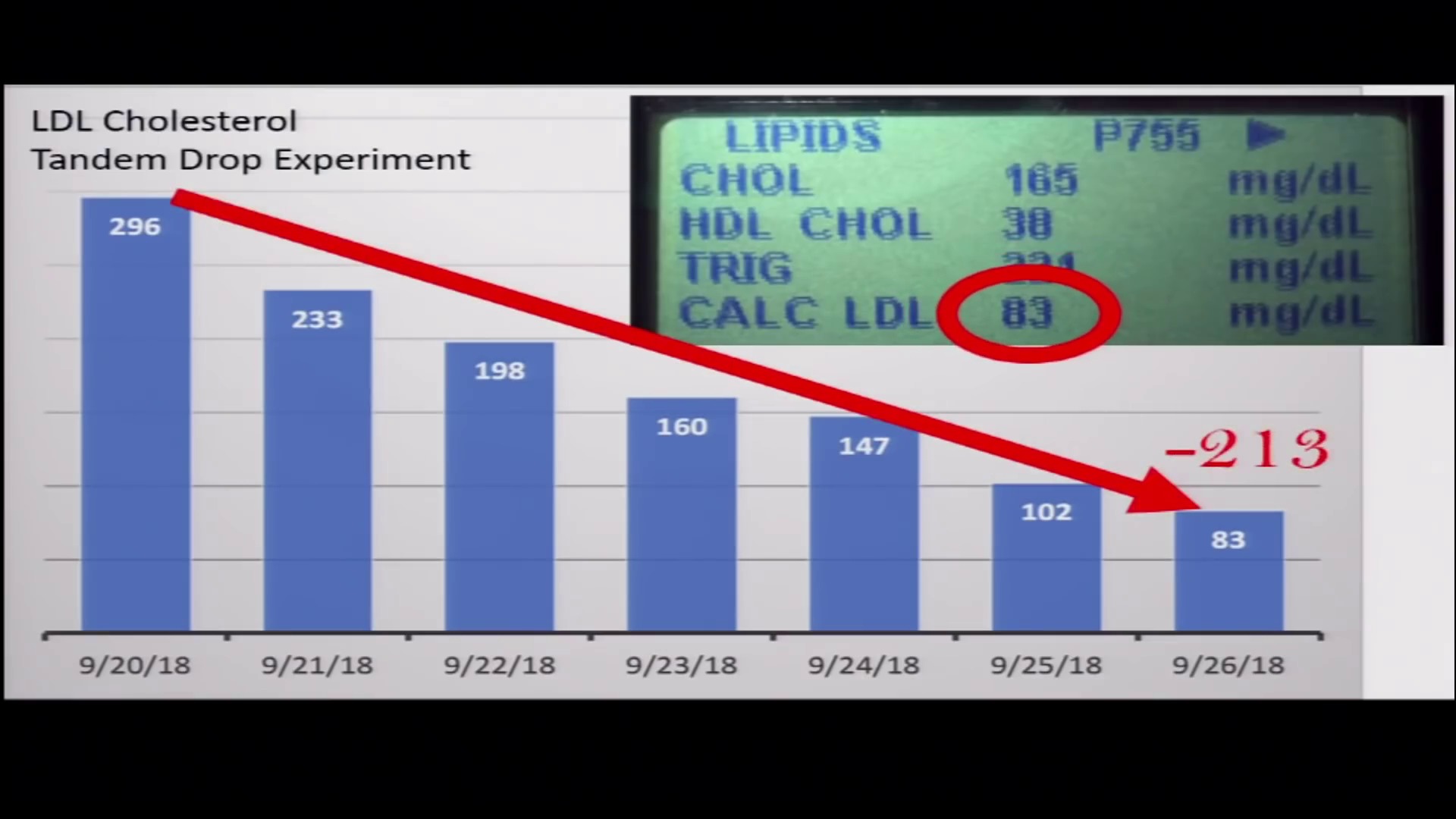
You can literally 'game' an LDL test by eating nothing but Wonder Bread and hot dogs for three days before it. Are we sure we should be trusting such a marker for a lifelong drug prescription? Image Courtesy Dave Feldman[16] and What I've Learned[20]
And he does it both repeatably and reliably. This is all logged on his website[16] and Facebook groups,[21] which we'll discuss in future parts, since Dave has an alternate theory on lipids that seems to make far more sense.
Point being, LDL can be (and is) gamed worse than single-deck blackjack. So are we sure this data point is something we should be basing lifetime drug decisions on? Shouldn't we expect a more stable response? And if short-term diet alters it, how confident can you really be in your "diagnosis"?
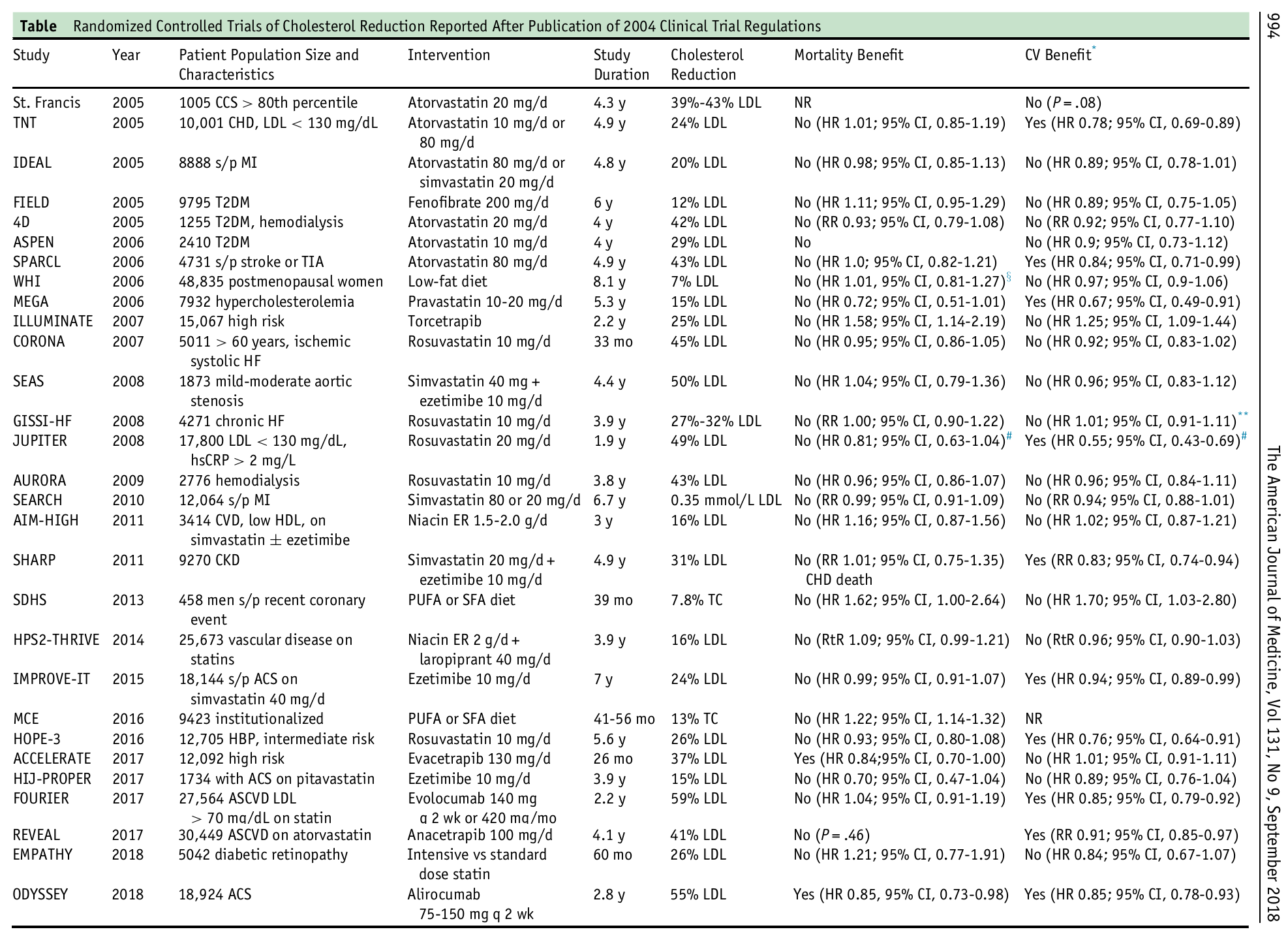
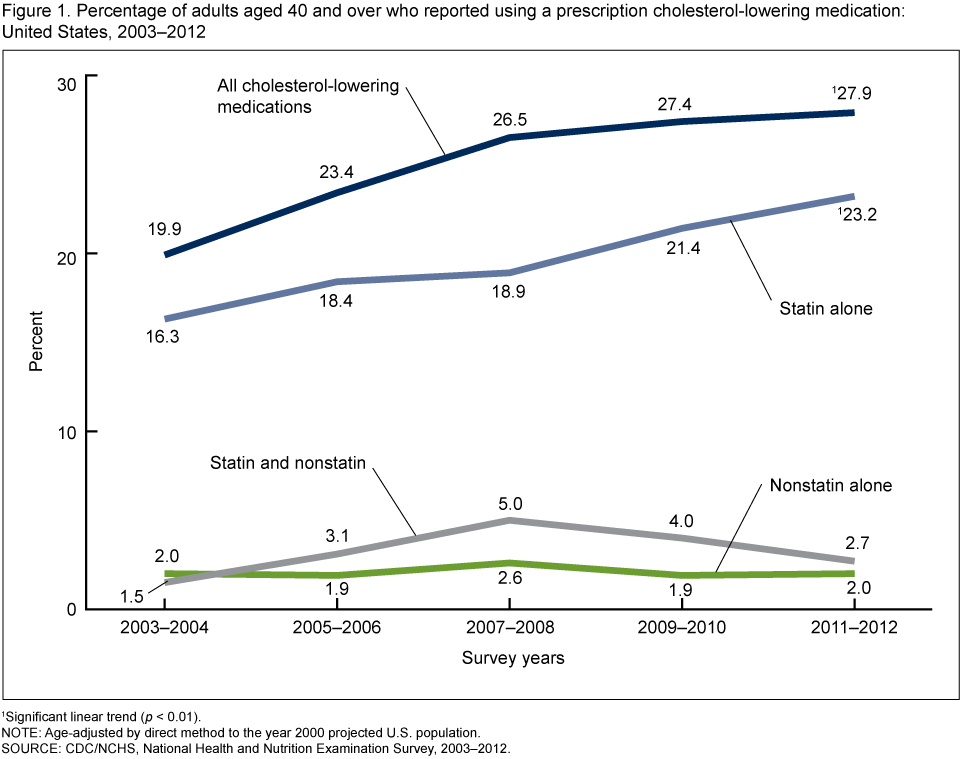
So what happens when you lower LDL with statin drugs?
Sadly, we've been selling drugs to fudge this codependent number for decades, and all things told, it's been a relatively safe way for the pharma complex to make billions of dollars. Given the information above regarding my personal situation, I'll avoid all of the miserable side effects.
But since this whole mess was perpetrated upon us, there have been several studies tracking the success (or lack thereof) of LDL-lowering drugs. And look at what happens:
Now seriously, if dropping LDL for every single person is so important, why is it having so little effect on mortality and a seemingly random effect on cardiovascular disease?!
Because, once again, LDL IS NOT THE PROBLEM!!
Meet The LDL Paradox
Researchers who still buy into the nonsensical LDL-based lipid hypothesis get perplexed when real world results don't emulate what they expect from the numbers. So much so that they call it the "LDL Paradox".[23]
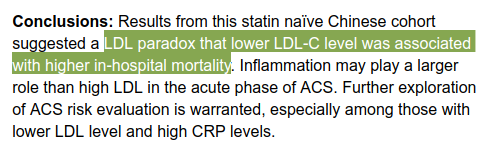
This recent study found an 'LDL Paradox', where low LDL patients died far more frequently in the hospital.[23] You sure this is a "paradox"??
A study published in November of 2018 showed that the lowest LDL group had the highest in-hospital mortality! Compare a whopping 9.7% mortality rate in the lowest LDL group against 2.7% and 3.5% in higher LDL groups![23] In that study, it turned out that CRP (C-Reactive Protein, a key marker for inflammation) was an even stronger driving force, but LDL may actually be protective for many, especially the elderly who are often prescribed statins to lower it!
So the study chalks it up to an "LDL paradox" and that further exploration is required, especially with respect to CRP's effects alongside LDL.
Here's a hint, folks: it's not a "paradox"! There is no paradox! It's simply an incomplete, wretched theory that's been used to sell far too many people drugs they don't need. Every time we look, there's a stronger variable alongside LDL.
2023 Update: 32% lower mortality in veterans with LDL over 190
An update in 2023 also shows this "paradoxical" finding -- a newer cohort study on almost 1500 male veterans showed that "higher TC [total cholesterol] and LDL-C were independently and paradoxically associated with lower risk of all-cause mortality and longer survival time in men" -- and the numbers are staggering, with a whopping 32% lower death rate in men with LDL over 190![24]
The real paradox: your doctor's weapons are practically useless with low-carbers
And if you're a low-carb dieter with numbers like me, your doctor is basically useless to help you, because they have to follow the "standard of care", and that dictates the statin conversation if your LDL is high - irregardless of HDL and Trigs!
Simply put, this game is not setup for low-carb dieters, and you should seek a second or third opinion from someone who knows this before playing.
High LDL, Low Trigs, and high HDL? Find a single study.
Here's a simple fact:
There is not a single study on non-drugged individuals showing that the combination of high LDL, low triglycerides, and high HDL ever leads to more heart disease.
Not a single one!
This is actually a public challenge made by Feldman (mentioned above), who is willing to pay $1000 to anyone who finds such a study. He posted that challenge quite a while ago, and a year in, nobody has found any such data.
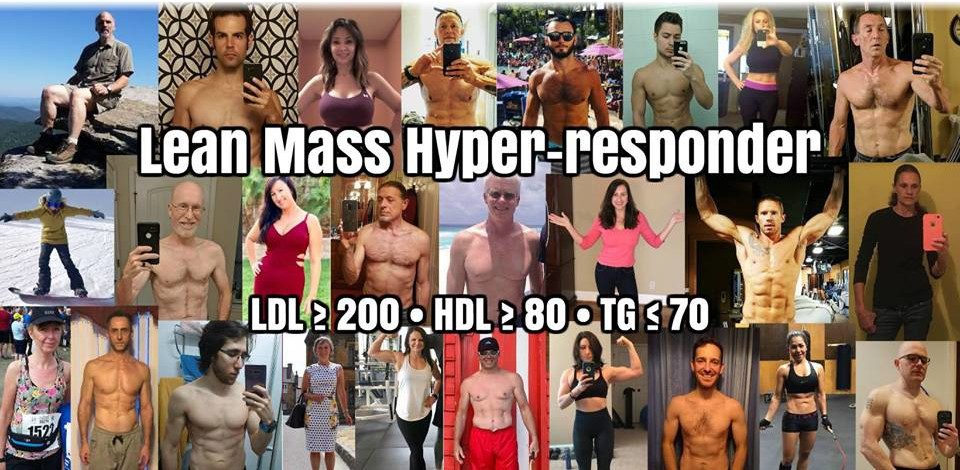
Meet the "Lean Mass Hyper-Responders"
Dave has a term for individuals similar to myself, who have high LDL but also high HDL and low triglycerides when going low-carb: Lean Mass Hyper-Responders.[25] We're a whole new phenotype of individual, and what we're seeing is that the conventional rules don't apply to individuals like us when on the keto diet.
Most of these "LMHR" individuals exhibit the following traits:
- They're nearly always "lean" by today's standards (ie body fat ≤20% for men and ≤23% women)
- Usually moderately to very fit and athletic
- Report feeling better than they ever have when going low carb
- Almost NEVER get sick.
While my LDL is actually slightly too low to fit Dave's true "LMHR" definition, I fit every other scenario. Interesting, no?
Dave Feldman and Cholesterol Code on a Mission
Even more interesting is that Dave isn't stopping there, even though he's now quite confident that his low carb diet -- with increased LDL and all -- isn't going to kill him. He's actually taken his research and experimentation further, driving a new theory that our society's entire view of cholesterol is simply wrong.

Along with his team at Cholesterol Code, a scientist named Dave Feldman is flipping the lipid hypothesis on its head.
While out of the scope of this document, Dave provides an alternative theory that makes sense for all individuals and dieters, and he calls it the "Lipid Energy Model".[26] The above traits effectively represent individuals with less body fat, less glycogen stores, yet higher energy demands. In that situation, what happens: more energy transporters required.
And given the fourth point above, LDL may just be protective, not harmful. Godspeed, Dave.
Don't blame the ambulance for the accident
So what is the problem? What are the real risk factors? We touched upon some things above, but we'll dive a bit deeper, in case your other numbers are indeed problematic.
Those actual risk factors will be covered in more depth in part two of this series, which will be linked here when the post is published. Until then, subscribe to our YouTube channel and follow us on Instagram, Facebook, and/or my personal Twitter.
PS: And for the sake of temporary closure regarding my personal situation, I requested further testing from the nurse practitioner who wanted to put me on statins, such as a Coronary Artery Calcium (CAC) Test, NMR (Advanced LipoProtein Test to better count and determine particle sizes), and mentioned checking insulin and doing a glucose challenge test.
Alas, those requests were all rejected, and I summarily fired this office as my primary care provider, finding a doctor and coach more aware of the relevant research.
The above tests will give you a hint of some of the items to come in the next post. Stay tuned!
Update on July 24, 2019: Despite my general non-concern with this lipid profile for at least part of the year, I wanted to see what would happen if I placed 100g net carbs around my AM workouts. Behold in the updated posts, "How I "Fixed" My Cholesterol Levels with a Low-Carb Diet" and the associated video, "Reducing LDL Cholesterol with a Low-Carb Diet (But Not TOO Low!)"


Comments and Discussion (Powered by the PricePlow Forum)