When the Black Magic Supply team releases a product, they're either going all in on high-intensity formulation strategies or bringing us something incredibly new from "beyond the ether" as it were originally prophesied in their momentous launch years ago.
We've been excited about the new Black Magic Villain pre-workout supplement, which brings a new high-energy twist compared to their famous BZRK formula, but there's more to fitness life than just energy. There's also sleep.

Black Magic Supply presents Dusk to Dawn, a wildly unique sleep aid featuring a new ingredient in Cocculus laurifolius and an older, repurposed one in theacrine! We discuss how it all works here.
Dusk to Dawn: A wildly unique sleep aid from Black Magic Supply
For today's formula coverage, Black Magic Supply brings us Dusk to Dawn, a novel capsule-based sleep aid. Inside, we're seeing a few novel takes: the appearance of a promising new ingredient in Cocculus laurifolius as well as a unique inclusion of theacrine, which isn't commonly found in sleep aids... but perhaps should be!
Dusk to Dawn relies on both herbal ingredients (like Cocculus and valerian) as well as single-molecule compounds like 5-HTP and a small hit of melatonin (2 milligrams). Beyond that, we get a decent hit of magnesium glycinate, which we'll basically never turn down before bed!
If you want to learn more, read on – but first, let's check the PricePlow news and deals:
Black Magic Dusk To Dawn – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.
Black Magic Supply Dusk to Dawn Ingredients
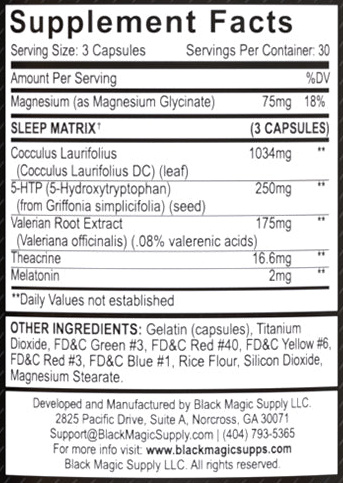
In a single, 3-capsule serving of Dusk to Dawn from Black Magic Supply, you get the following:
-
Cocculus Laurifolius (Cocculus Laurifolius DC) (leaf) – 1,034 mg
We've got some new stuff in here, and an ingredient in theacrine that's often used in pre-workouts - this article explores it all!
Cocculus laurifolius is a plant that's been studied for its anticonvulsant and anxiolytic properties.[1,2]
The basic mechanism of action behind Cocculus is its ability to act on the central nervous system's GABAergic pathways.[1,2] This is a mechanism of action shared by many popular anti-anxiety supplements like theanine, magnesium, and glycine.
Another way of putting it is that these supplements are anti-excitotoxic. Thanks to their upregulation of GABA, or downregulation of GABA's antagonist glutamate, they help prevent excitotoxicity, which is the uncontrolled, sporadic neuronal firing that can produce neuroinflammation, seizures, and even permanent brain damage.[3,4] In its milder forms, excitotoxicity manifests as irritability, hyperactivity, or anxiety.[5-7]
The GABAergic activity of Cocculus was shown in a study where researchers gave rats strychnine, which is a GABA antagonist and induces excitotoxic seizures that can be fatal. As it turns out, rats who got Cocculus showed significantly delayed seizure onset, longer survival times, and a higher survival rate than rats who got a placebo.[1] This implies that Cocculus is GABAergic enough to preserve GABA function in the face of strychnine exposure. The flavonoids in Cocculus appear to play a part in stabilizing neurons as well.[1]
The anti-anxiety effects of Cocculus were shown in a mouse study in which researchers compared the behavior of Cocculus-treated mice with controls.[2] There was also a group that got diazepam, a powerful anti-anxiety drug that's also sold under the name Valium.
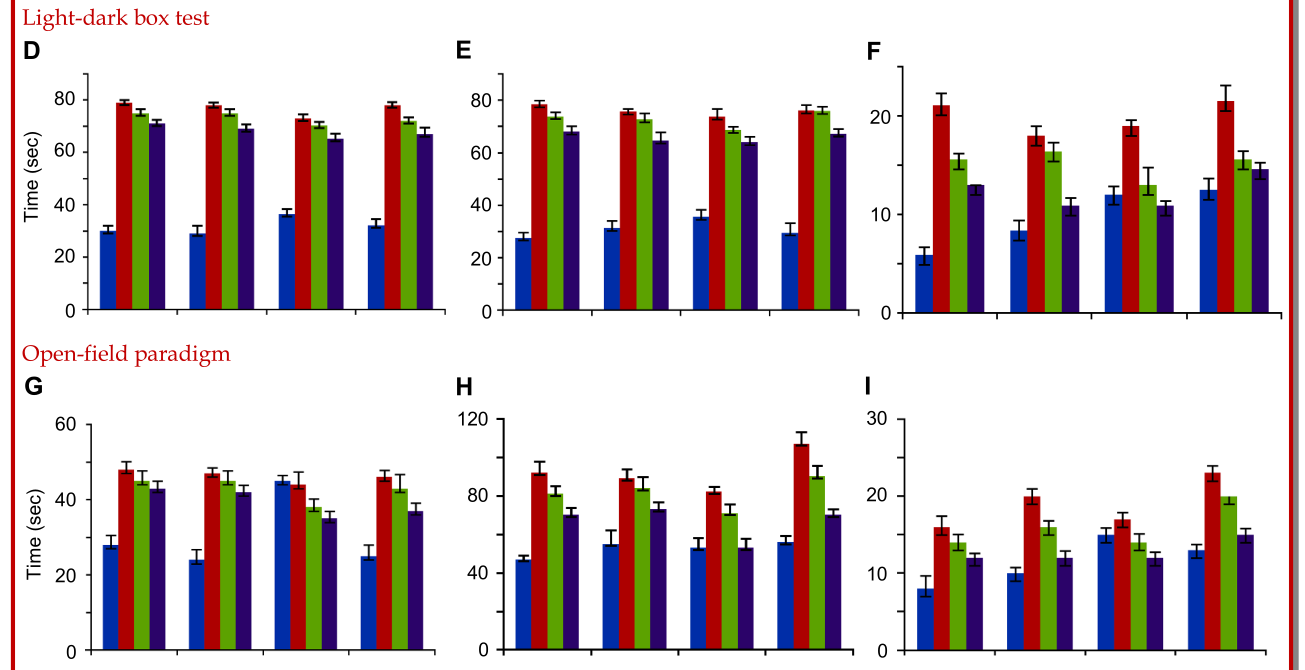
Anxiety was assessed by the light-dark box test and the open field paradigm. In these tests, mice who spend more time in the dark, or less time in the open, are thought to exhibit signs of anxiety.
Mice administered ethanolic extracts of Cocculus (ECL) showed significant reductions in anxious behavior, compared to the control group. The Cocculus mice spent more time in lighted or open areas than they did in dark or sheltered spaces.[2] Blue bars are the control group, red bars are for the diazepam group, green bars are for the 200 mg/kg ECL group, and black bars are for the 400 mg/kg ECL group.[2] D) percentage number of entries, E) percentage time spent and F) total number of rearing in light area in light-dark box test; G) number of center square crossings, (H) number of peripheral square crossings and I) total number of rearings in open-field paradigm.[2]
Compared to the control mice, those who got diazepam exhibited far less avoidant and more exploratory behavior, spending more time in open and lighted areas than controls. That's not terribly surprising. What is surprising is that the ECL extract did almost as well as the diazepam at improving certain behavior indicators.[2]
For example, mice who got ECL spent almost as much time in lighted areas as mice who got diazepam (this is shown in figure E).[2] They also showed significantly more rearings (standing on their hind legs to survey the environment) in both lighted areas and open areas (figures F and I, respectively).[2]
In addition, Cocculus laurifolius contains constituents that may function as muscle relaxants,[8] which is fitting for a sports nutrition brand like Black Magic Supply, whose customers are generally the type that train quite hard (as evidenced by their BZRK and Villain pre-workouts).
-
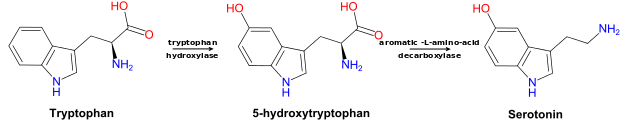
5-HTP (5-hydroxytryptophan)(from Griffonia simplicifolia Extract) (Seed) – 250 mg
Synthesis of the neurotransmitter serotonin requires 5-HTP as a precursor -- and serotonin is a natural precursor to melatonin. Since serotonin and melatonin help regulate the circadian rhythm,[9] this makes 5-HTP a potentially useful supplement for improving sleep quality.
At least one double-blind, randomized, placebo-controlled study has borne this out. Older adults who took 5-HTP for three months had about a 14% better global sleep score (GSS) by the end of the study period, compared to the placebo group.[9] The kicker is that this study only used a 100-milligram daily dose of 5-HTP – that's less than half the amount in Dusk to Dawn!
One study on 5-HTP supplementation in children suffering from chronic night terrors found that 93.5% of participants saw improvement in their condition.[10] The children were prescribed 2 mg/kg per day – that's in the same ballpark as a 250-milligram dose for an adult.
We often see 50-100 milligram doses of 5-HTP in sleep aids, so this is impressive. We often consider it a nice way of creating a "time-released" serotonin and melatonin, since it can help promote their synthesis downstream.
-
Valerian Root Extract (Valeriana officinalis) (.08% valerenic acids) – 175 mg
Valerian root, known officially as Valeriana officinalis, is an herb that grows in Europe, Asia, and North America. It's used to manage symptoms of anxiety and insomnia.[11] The root of valerian is rich in antioxidants, particularly valerenic acid and isovaleric acid, its primary bioactive constituents.[11] Both compounds have been found to upregulate GABA, leading to feelings of increased relaxation and decreased feelings of perceived stress and anxiety.[11]
Valerian doesn't necessarily help you fall asleep faster – research on its ability to improve time to onset of sleep is a mixed bag[12-15] – but it does seem to significantly improve sleep quality.[12,15]
-
Theacrine – 16.6 mg
Theacrine as a sedative is an interesting subject in the supplement industry. There's been a fair amount of controversy over whether theacrine is stimulating or sedative, but, as it turns out, the answer is... both. It's stimulating in high doses, and sedating in low doses![16]
Animal research indicates that theacrine, when co-administered with the depressant phenobarbital, can increase the duration of sleep induced by phenobarbital. Caffeine, the famous stimulant, has the opposite effect when given with phenobarbital![17]
This makes theacrine a very interesting play in a sleep aid. Some users anecdotally feel very sleepy when using it - even in pre-workout supplements next to caffeine - so to them, it makes sense here. But for those who like its effects next to stimulants, a low-dose like this in a sleep aid may just surprise them.
We'd love to specify the mechanism of action here, but nobody knows yet! It remains to be elucidated by science.[16] Theacrine is known to help optimize 5-HTP production, though, so regulating circadian function through serotonin probably has something to do with it.
Overall, we have been waiting quite a while for someone to give this a shot - and we're happy Black Magic Supply did it with Dusk to Dawn. They definitely didn't put a boring product together here!
-
Melatonin – 2 mg
The hormone melatonin plays a central role in governing the body's circadian rhythm. Its secretion is a signal that it's time to sleep,[18] and repeated melatonin exposures, at a particular time of day, can be used to set your body's natural bedtime, which is why the hormone is often used to manage jet lag.[19]
Melatonin's interaction with blue light
Melatonin sets your body's internal clock for waking and sleeping[18] by interacting with light in your environment. This happens because arylalkylamine N-acetyltransferase, the enzyme responsible for producing melatonin, is downregulated when light hits your eyes. In nature, this happens while the sun is up.[20] Morning light helps wake us up partly by suppressing melatonin production.[21]
The color (or, more technically, wavelength) of light that's primarily responsible for suppressing melatonin is blue light.[22] This should make intuitive sense, as blue skies are what we usually see in the middle of the day.
The tricky, and unfortunate, thing is that not only natural light does this. Blue light from technological sources like TV screens, computer monitors, and, most troublingly, cell phones can also downregulate the enzyme.[23]
Fortunately, when taken at the right time before bed, melatonin supplements can help correct this problem. Melatonin has been shown to significantly increase sleep quality without significant adverse effects, particularly in older adults.[24]
Other studies have found that melatonin supplementation can help mitigate sleep disturbances like migraines and insomnia.[25,26]
Because it has persistent effects on the circadian clock, it's important to only take melatonin at your intended regular bedtime, and combine it with good sleep hygiene practices like avoiding blue light exposure in the evening.[27]
-
Magnesium (as Magnesium Glycinate) – 75 mg (18% DV)
Magnesium is an essential mineral with many metabolic benefits. Restoring magnesium levels, even in cases of mild or subclinical deficiency, can have significant positive effects on crucial aspects of health, like blood sugar, insulin production, and insulin sensitivity.[28-34]
Again, even mild deficiencies in magnesium can lead to or worsen stress and anxiety,[35-37] which obviously isn't great for sleep quality. One study in seniors found improvements in sleep EEGs (brain wave recordings) from magnesium supplementation.[38]
Why magnesium glycinate?
Magnesium glycinate, which is a magnesium molecule bound to the amino acid glycine, is our favorite form of magnesium thanks to its very high bioavailability, and the fact that we love glycine. It's far more bioavailable than cheaper, more common forms like magnesium oxide.[39]
As glycine is GABAergic,[40] supplementing with glycine itself can also reduce stress and decrease time to sleep onset. However, the doses used are typically much larger than what's in Dusk to Dawn, usually on the order of at least 3 grams per day.[41-51]
Still though, we have some glycine, so it should help a bit.
The prevalence of magnesium deficiency
Are you ready for the new Black Magic Supply VILLAIN pre-workout
Because magnesium is involved in so many different processes, magnesium deficiency is tough to diagnose, but usually takes the form of fatigue, insulin resistance, and suboptimal cardiovascular function.[52,53]
It seems like many (if not most) of us are dealing with these symptoms today. So how common is magnesium deficiency?
The first thing to know is that Americans used to get a lot more magnesium from our food than we do today. This is because the magnesium content of soil and,hence, the food we produce on our soil, has declined precipitously in the last 100 years.[52,54-58]
Another challenge is that the diagnostic threshold for magnesium deficiency may not be adequate – 0.75 mmol/L serum magnesium is considered sufficient, but some research shows that levels below 0.863 mmol/L increase risk of diabetes by more than 300%.[59] This means there are probably lots of undiagnosed magnesium deficiency cases out there.
One study points out that magnesium deficiency prevalence is probably getting worse. As of 2006, only 48% of the U.S. population was consuming the recommended amount of magnesium, down from 56% in 2002.[60]
Long story short: this is a solid boost of magnesium and glycine... but check your diet -- you may actually want more!
Dosage and Timing
Take 1-3 capsules 30 minutes before bed. Since Dusk to Dawn contains a new ingredient in Cocculus, it's not a bad idea to start light. Additionally, melatonin tolerances vary, so that could help drive the dosage here - if 2 milligrams of melatonin is too much, 1-2 capsules could support a more refreshed wakeup.
Dusk to Dawn: A new and unique sleep aid
This is an extraordinarily interesting formula, with more departures from the norm than usual. Cocculus is an ingredient we've never covered in a sleep formula before – the research is promising (yet we definitely want more), so we're excited to hear feedback from consumers and industry professionals on this formula's effectiveness.
Using low-dose theacrine is a very savvy move we've long been waiting for someone to take a stab at. Partisans have spilled a lot of ink denying that theacrine has sedative effects despite compelling evidence that it does, so it's ironic and refreshing to see the low-dose application being embraced here.
The dose of 5-HTP is also awesome – way beyond the 50-100 milligrams typically used. Valerian also has a well-researched track record -- you can definitely use a couple extra botanicals when using capsules.
Finally, magnesium is a great ingredient for this application, too, and it's especially nice that Black Magic has opted for one of the best (if not the best) forms of this mineral, which is magnesium glycinate. We normally recommend higher doses, but this is a capsule-based product and quality forms of magnesium take up a lot of space. So if you need more magnesium, and you very well may, you can always add more separately.
With that said, this is a phenomenally unique product and we're excited to give it a whirl.
Black Magic Dusk To Dawn – Deals and Price Drop Alerts
Get Price Alerts
No spam, no scams.
Disclosure: PricePlow relies on pricing from stores with which we have a business relationship. We work hard to keep pricing current, but you may find a better offer.
Posts are sponsored in part by the retailers and/or brands listed on this page.






Comments and Discussion (Powered by the PricePlow Forum)